Biological Activity of Propolis-Honey Balm in the Treatment of Experimentally-Evoked Burn Wounds
Abstract
:1. Introduction
2. Results and Discussion
2.1. Clinical Assessment
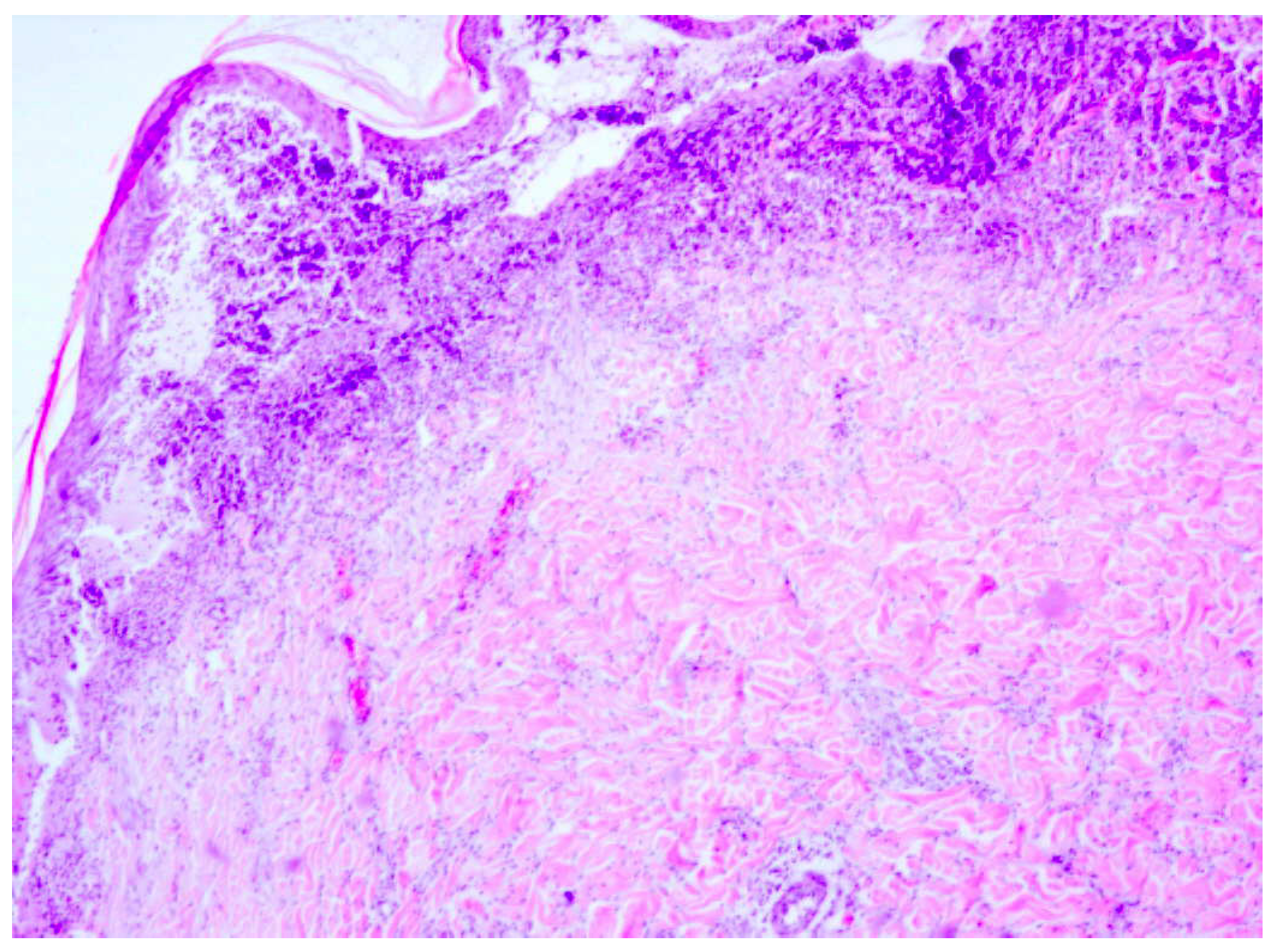
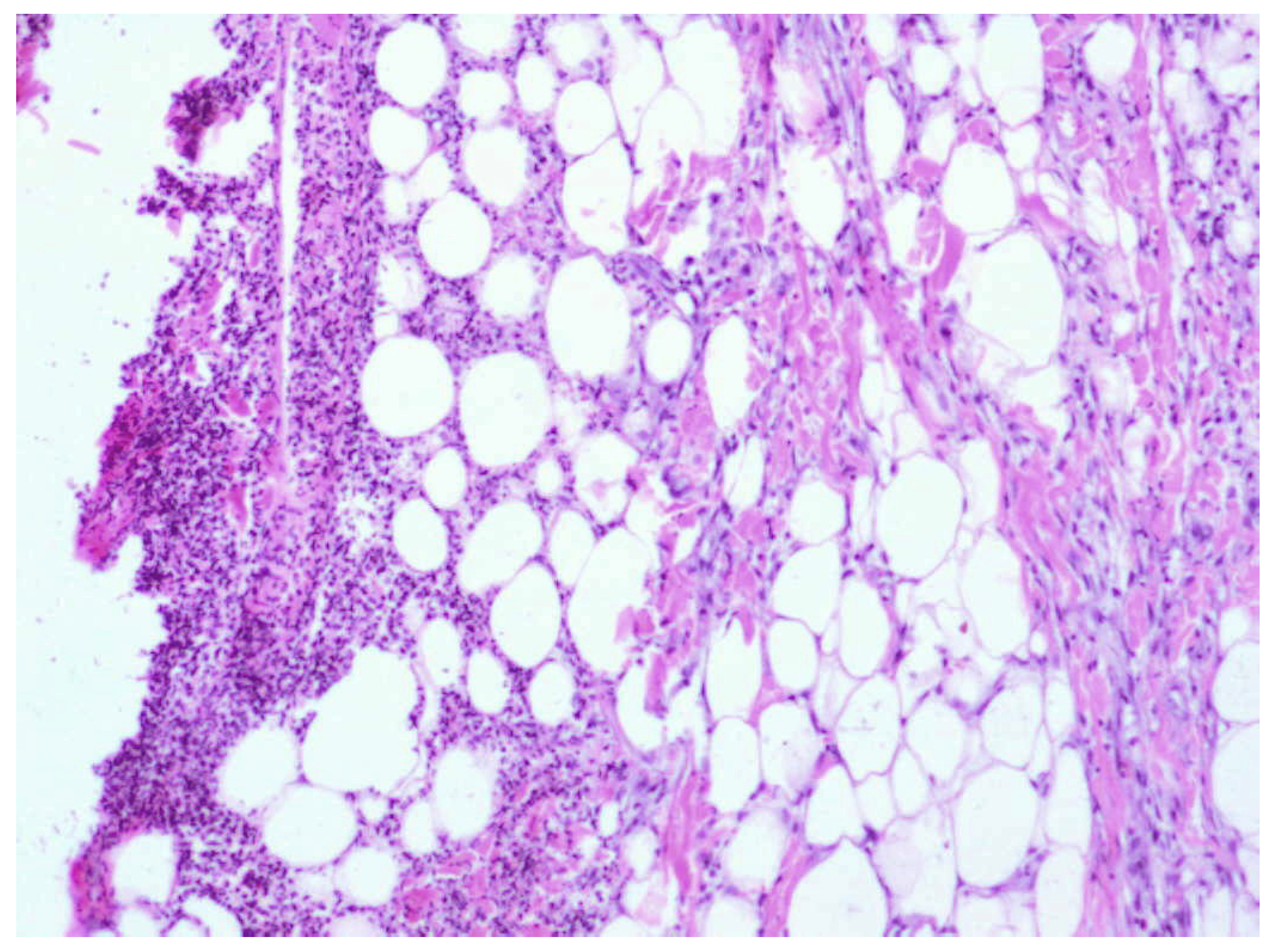
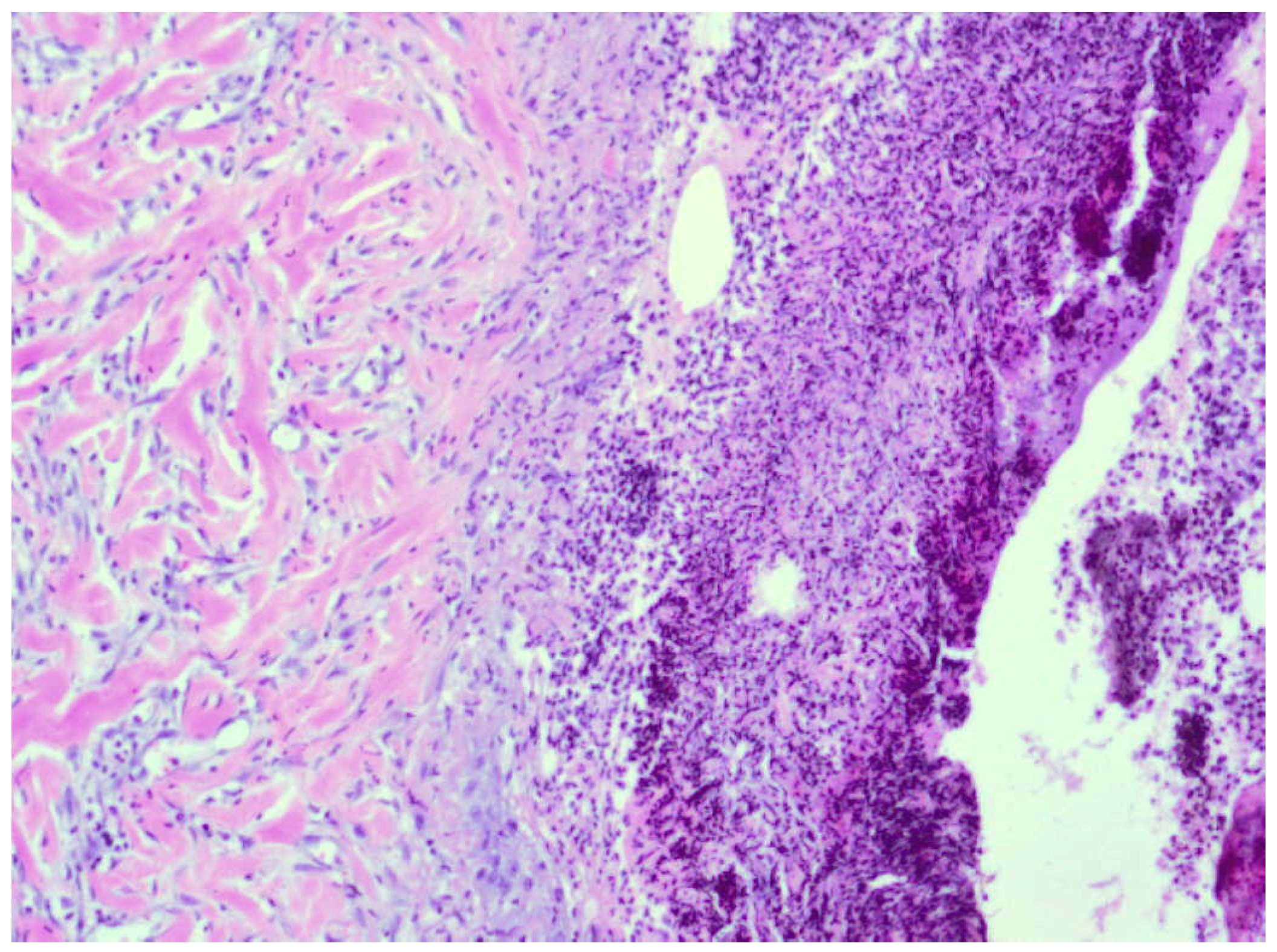
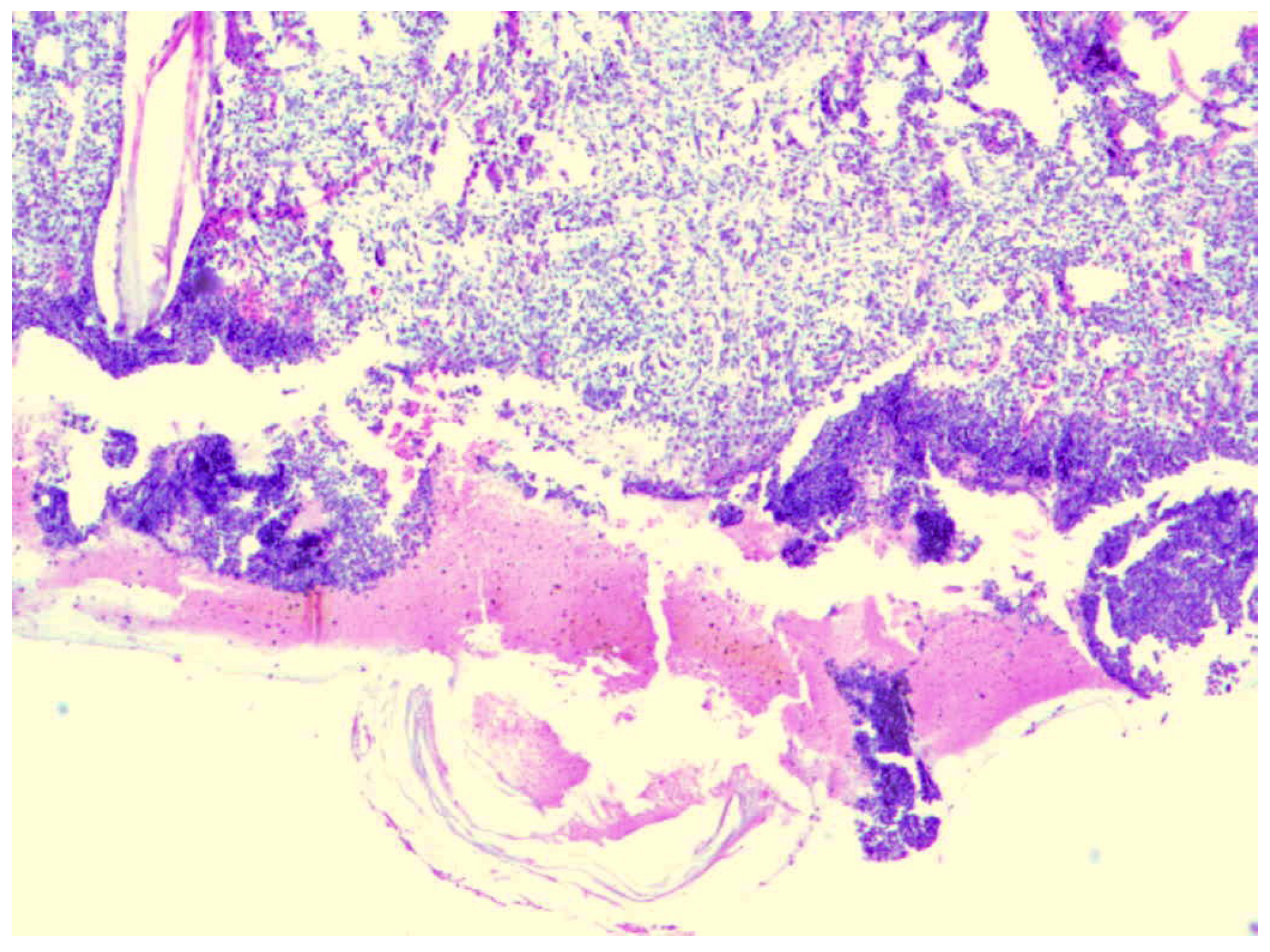
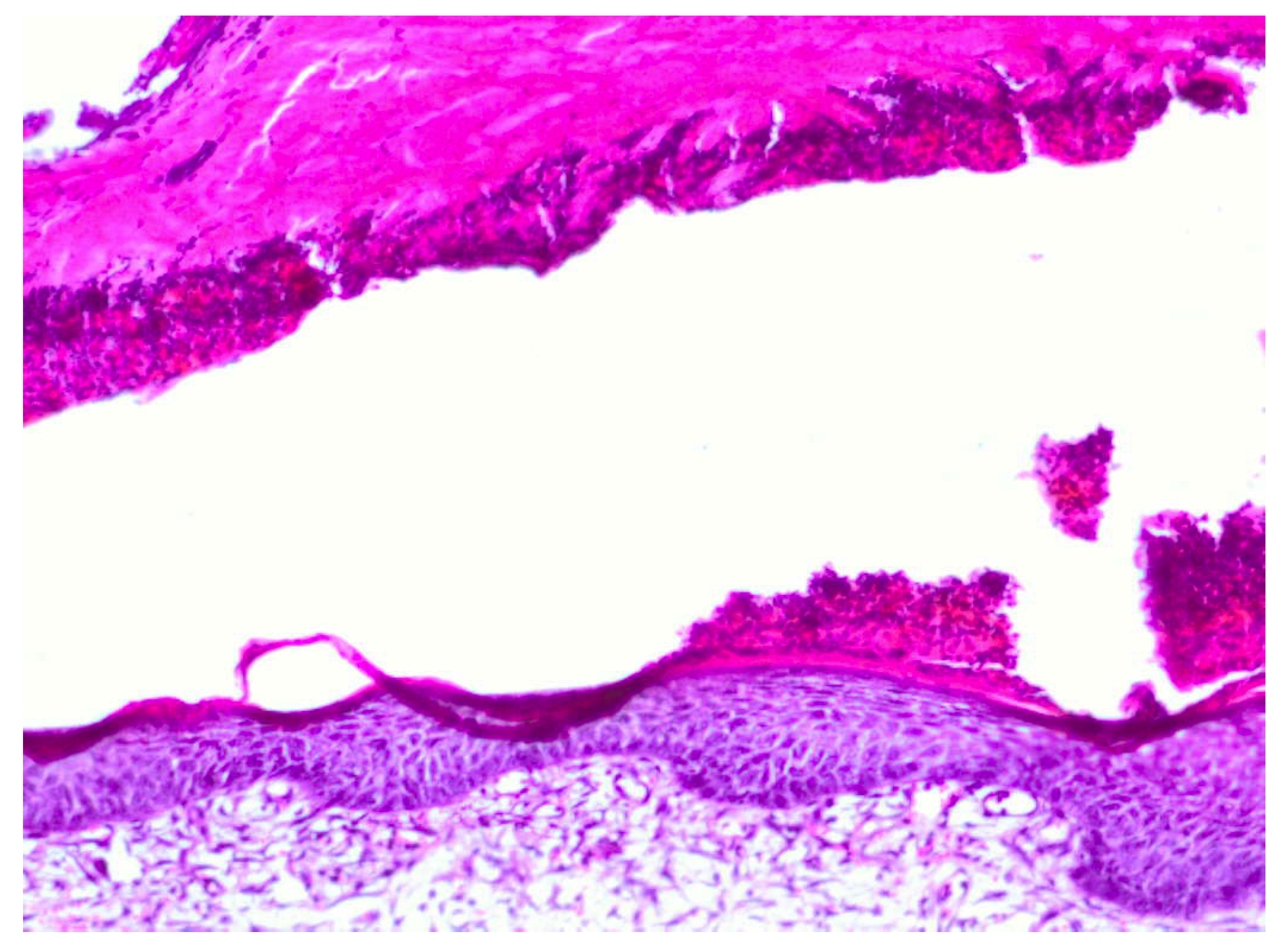
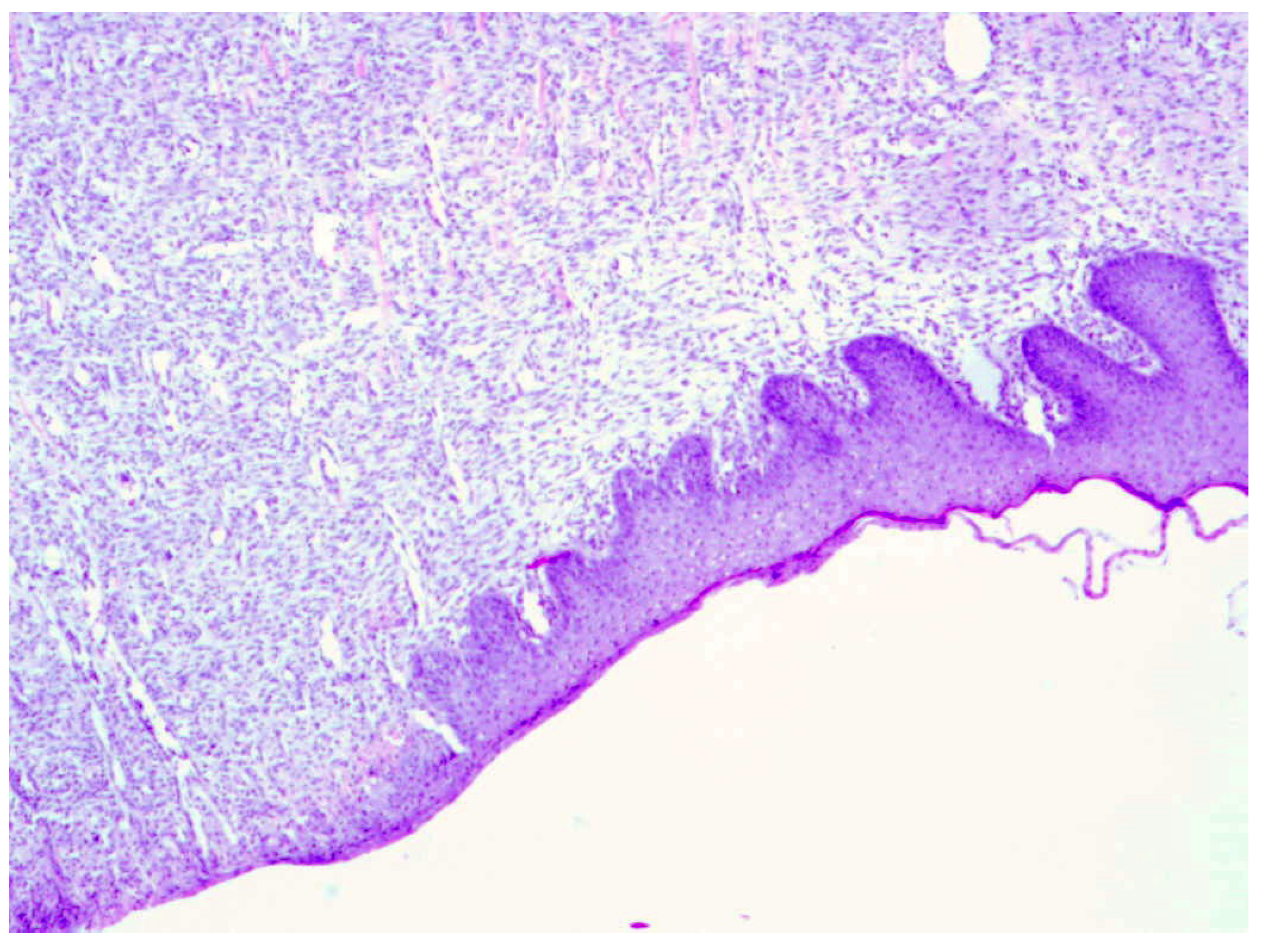
2.2. Histopathological Test Results


2.3. Biochemical Test Results
| Healthy skin | Burn wounds | ||||
|---|---|---|---|---|---|
| 0.9% NaCl | Dermazin | 1% Sepropol | 3% Sepropol | ||
| hydroxyproline [g/mg dry mass ± SD] | 58.2 [±0.73] | 45.5 [±0.67] | 57.5 [±0.81] | 64.2 [±0.47] | 68.4 [±0.63] |
| collagen [g/mg dry mass] | 464 | 360 | 456 | 512 | 544 |
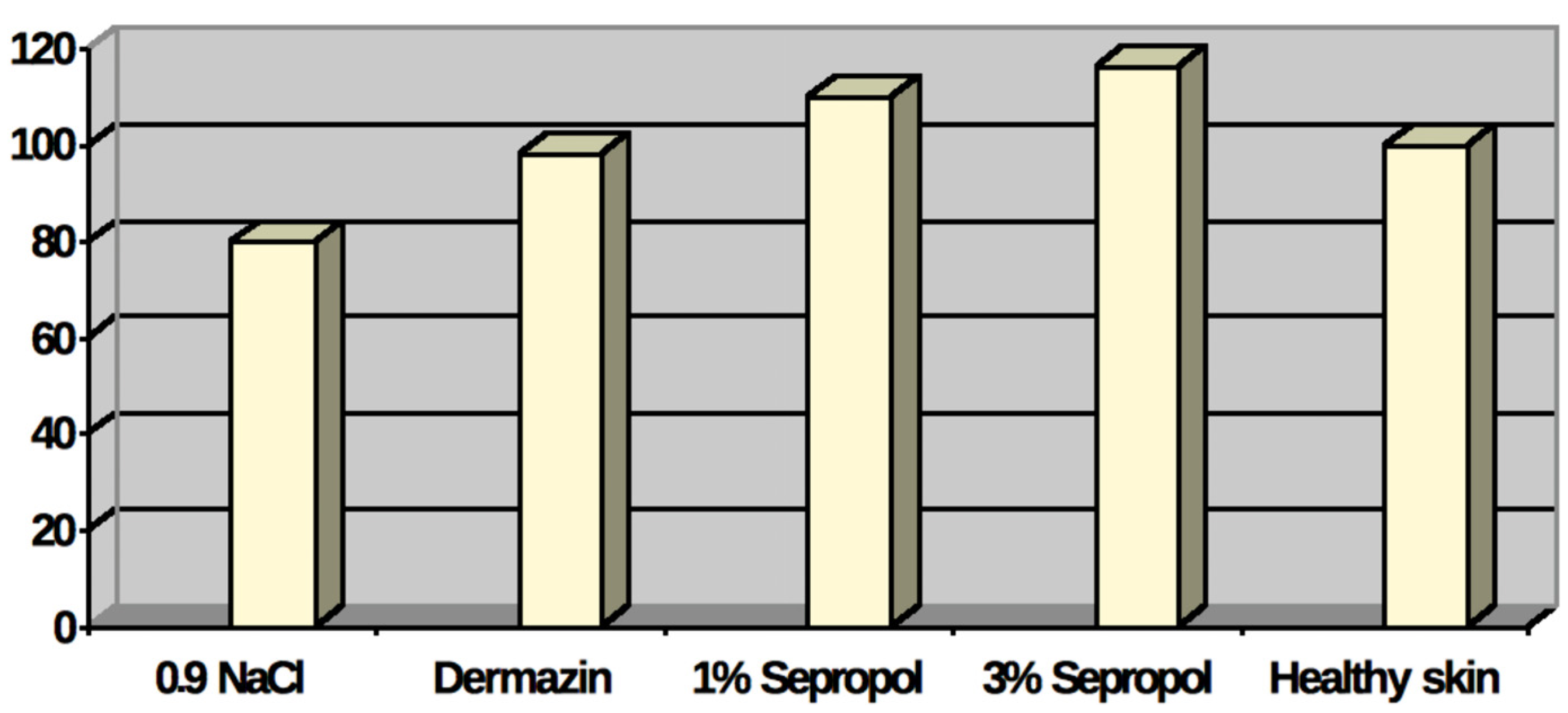
2.4. Statistical Analysis
| Variable | Variance analysis (Determined effects are significant with p < 0.0500) | |||||||
|---|---|---|---|---|---|---|---|---|
| SS effect | df effect | MS effect | SS error | df error | MS error | F | p | |
| Hydroxyproline level | 2745.234 | 4 | 686.311 | 216.000 | 32 | 6.750 | 101.676 | 0.0000 |
| Method | LSD test; Variable (Determined differences are significant with p < 0.05000) | ||||
|---|---|---|---|---|---|
| {1} M = 45 | {2} M = 57 | {3} M = 64 | {4} M = 68 | {5} M = 58 | |
| NaCl 0.9% {1} | 0.000000 | 0.000000 | 0.000000 | 0.000041 | |
| Dermazin {2} | 0.000000 | 0.000002 | 0.000000 | 0.717403 | |
| Sepropol 1% {3} | 0.000000 | 0.000002 | 0,002603 | 0.035857 | |
| Sepropol 3% {4} | 0.000000 | 0.000000 | 0.002603 | 0.000922 | |
| Healthy skin {5} | 0.000041 | 0.717403 | 0.035857 | 0.000922 | |
3. Experimental
3.1. Reagents
3.2. Therapeutic Agents
3.3. Tissue Materials
3.4. Histopathological Test
3.5. Biochemical Test
4. Conclusions
Acknowledgments
Conflicts of Interest
References
- Heimbach, D.; Engrav, L.; Grube, B.; Marvin, J. Burn depth: A review. World J. Surg. 1992, 16, 10–15. [Google Scholar] [CrossRef]
- Moore, O.A.; Smith, L.A.; Campbell, F.; Seers, K.; Moore, R.A. Systematic review of the use of honey as a wound dressing. BMC Complement. Altern. Med. 2001, 1, 2–8. [Google Scholar] [CrossRef] [Green Version]
- Najafi, M.F.; Vahedy, F.; Seyyedin, M.; Jomehzadeh, H.R.; Bozary, K. Effect of the water extract of propolis on stimulation and inhibition of different cells. Cytotechnology 2007, 214, 129–134. [Google Scholar]
- Stojko, A. Treatments Based on Bee Products (Apitheraphy). In Medycyna Naturalna; Janicki, K., Rewerski, W., Eds.; PZWL: Warszawa, Poland, 2001; pp. 105–113. [Google Scholar]
- Stojko, J.; Stojko, R.; Szostak, R.; Stojko, A.; Wróblewska-Adamek, I.; Szaflarska-Stojko, E.; Kabała-Dzik, A. Observations on the possibile uses of the ApiPanten preparation In the therapy of burn wounds. Ann. Acad. Med. Siles. 2004, 58, 117–120. [Google Scholar]
- Pytel, A.; Strzałka, B.; Fila, A.; Stojko, A.; Mazurek, U.; Wilczok, T. Zmiany Dynamiki Ekspresji Histonu H3 W Gojacej Sie Ranie Oparzeniowej Pod Wpływem Preparatu Propol-O; 37 Zjazd Polskiego Towarzystwa Biochemicznego: Toruń,Poland, 2001. [Google Scholar]
- Kędzia, B. Chemical composition of Polish propolis. Part 2. New study. Post. Fitoter. 2009, 2, 122–128. [Google Scholar]
- Scazzocchio, F.; D`Auria, F.D.; Alessandrini, D.; Pantanella, F. Multifactorial aspects of antimicrobial activity of propolis. Microbiol. Res. 2006, 161, 327–333. [Google Scholar] [CrossRef]
- Silici, S.; Kutluca, S. Chemical composition and antibacterial activity of propolis collected by three different races of honeybees in the same region. J. Ethnopharmacol. 2005, 99, 69–73. [Google Scholar] [CrossRef]
- Uzel, A.; Sorkun, K.; Oncag, O.; Coculu, D.; Gensay, O.; Salih, B. Chemical composition and antimicrobial activities of four different Anatolin propolis samples. Microbiol. Res. 2005, 160, 189–195. [Google Scholar] [CrossRef]
- El-Bassuony, A.; AbouZid, S. A new prenylated flavonoid with antibacterial activity from propolis collected in Egypt. Nat. Prod. Commun. 2010, 5, 43–45. [Google Scholar]
- Lu, L.C.; Chen, Y.W.; Chou, C.C. Antibacterial activity of propolis against Staphylococcus aureus. Int. J. Food Microbiol. 2005, 102, 213–220. [Google Scholar] [CrossRef]
- Cardoso, R.L.; Maboni, F.; Machado, G.; Alves, S.H.; De Vargas, A.C. Antimicrobial activity of propolis extract against Staphylococcus coagulase positive and Malassezia pachydermatis of canine otitis. Vet. Microbiol. 2010, 142, 432–434. [Google Scholar] [CrossRef]
- Salomao, K.; Pereira, P.R.S.; Campos, L.C.; Borba, C.M.; Caballo, P.H.; Marcucci, M.C.; de Castro, S.L. Brazilian propolis: Correlation between chemical composition and antimicrobial activity. Evid. Based Compl. Alt. 2008, 5, 317–324. [Google Scholar] [CrossRef]
- Viuda-Martos, M.; Ruiz-Navajas, Y.; Fernandez-Lopez, J.; Perez-Alvarez, J.A. Functional properties of honey, propolis and royal jelly. J. Food Sci. 2008, 73, 117–124. [Google Scholar]
- Tomoi, S.; Go, M. The Nutraceutical Benefit, Part III: Honey. Nutrition 2000, 16, 468–469. [Google Scholar] [CrossRef]
- Ahmed, A.K.; Hoekstra, M.J.; Hage, J.J.; Karim, R.B. Honey-medicated dressing: transformation of an ancient remedy into modern therapy. Ann. Plast Surg. 2003, 50, 143–148. [Google Scholar] [CrossRef]
- Mashhood, A.A.; Khan, T.A.; Sami, A.N. Honey compared with 1% silver sulfadiazine cream in the treatment of superficial and partial thickness burns. J. Pak. Assoc. Dermatol. 2006, 16, 14–19. [Google Scholar]
- Bangroo, A.K.; Khatri, R.; Chauhan, S. Honey dressing in pediatric burns. J. Indian Assoc. Pediatr. Surg. 2005, 10, 172–175. [Google Scholar] [CrossRef]
- Dunford, C.; Cooper, R.; Molan, P.; White, R. The use of honey in wound management. Nurs. Stand. 2000, 15, 63–68. [Google Scholar] [CrossRef]
- Anand, A.; Shanmugam, J. Antistaphylococcal properties of natural honey. Biomedicine 1998, 18, 15–18. [Google Scholar]
- Subrahmanyam, M.; Hemmady, A.R.; Pawar, S.G. Antibacterial activity of honey on bacteria isolated from wounds. Ann. Burns Fire Disasters 2001, 14, 22–24. [Google Scholar]
- Wahdan, H.A. Causes of the antimicrobial activity of honey. Infection 1998, 26, 26–31. [Google Scholar] [CrossRef]
- Karayil, S.; Deshpande, S.D.; Koppikar, G.V. Effect of honey on multidrug resistant organisms and its synergistic action with three common antibiotics. J. Postgrad. Med. 1998, 44, 93–97. [Google Scholar]
- Irish, J.; Carter, D.; Blair, S. Honey Prevents Biofilm Formation in Staphylococcus aureus. In 8th Asian Apicultural Association Conference, Perth, Australia, 20–24 March 2006.
- Okhiria, O.; Henriques, A.; Burton, N.; Peters, A.; Cooper, R.A. The Potential of Manuka Honey for the Disruption of Biofilms Produced by Strains of Pseudomonas aeruginosa Isolated From Wounds. In Proceedings of the 155th Meeting of the Society for General Microbiology, Dublin, Ireland, 6–9 September 2004.
- Venkatachala, M.; Thangam, M. Bactericidal activity of different types of honey against clinical and environmental isolates of Pseudomonas aeruginosa. J. Alter. Complem. Med. 2007, 13, 439–441. [Google Scholar] [CrossRef]
- Khan, F.R.; Abadin, Z.U.; Rauf, N. Honey: Nutritional and medicinal value. Int. J. Clin. Pract. 2007, 61, 1705–1707. [Google Scholar] [CrossRef]
- Subrahmanyam, M. Honey, a nutritious food and valuable medicine. Sci. Ind. 2006, 2, 6–8. [Google Scholar]
- Frankel, S.; Robinson, G.E.; Berenbaum, M.R. Antioxidant capacity and correlated characteristics of 14 unifloral honeys. J. Apic. Res. 1998, 37, 27–31. [Google Scholar]
- Tonks, A.; Cooper, R.A.; Price, A.J.; Mo1an, P.C.; Jones, K.P. Stimulation of TNF -alpha release in monocytes of honey. Cytokine 2001, 14, 240–242. [Google Scholar] [CrossRef]
- Subrahmanyam, M.; Sahapure, A.G.; Nagane, N.S.; Bhagvat, V.R.; Ganu, J.V. Free radical control—The main mechanism of the action of honey in burns. Ann. Burns Fire Disasters 2003, 16, 135–138. [Google Scholar]
- Tonks, A.J.; Cooper, R.A.; Jones, K.P.; Blair, S.; Parton, J.; Tonks, A. Honey stimulates inflammatory cytokine production from monocytes. Cytokine 2003, 21, 242–247. [Google Scholar] [CrossRef]
- Lineen, E.; Namias, N. Biologic dressing in burns. J. Craniomaxillofac. Surg. 2008, 19, 923–928. [Google Scholar]
- Molan, P.C. Potential of honey in the treatment of wounds and burns. Am. J. Clin. Dermatol. 2001, 2, 13–19. [Google Scholar] [CrossRef]
- Molan, P.C. Re-introducing honey in the managment of wounds and ulcers—Theory and practice. Ostomy Wound Manage. 2002, 48, 28–40. [Google Scholar]
- Ingle, R.; Levin, I.; Polinder, K. Wound healing with honey—A randomized control trial. S. Afr. Med. J. 2006, 96, 831–835. [Google Scholar]
- Jull, A.B.; Rodgers, A.; Walker, N. Honey as a topical treatment for wounds. Cochrane Database Syst. Rev. 2008, 8, CD005083. [Google Scholar]
- Miri, M.R.; Hemmati, H.; Shahraki, S. Comparison of efficacy of honey versus silver sulphadiazine and acetate mafenid in the treatment of contaminated burn wounds in piggies. Pak. J. Med. Sci. 2005, 21, 168–173. [Google Scholar]
- Molan, P.C. The evidence supporting the use of honey as a wound dressing. Int. J. Low. Extrem. Wounds 2006, 5, 40–54. [Google Scholar] [CrossRef]
- Wijesinghe, M.; Weatherall, M.; Perrin, K.; Beasley, R. Honey in the treatment of burns: A systematic review and meta-analysis of its efficacy. N. Z. Med. J. 2009, 22, 47–60. [Google Scholar]
- Subrahmanyam, M. Honey-impregnated gauze versus amniotic membrane in the treatment of burns. Burns 1994, 20, 331–333. [Google Scholar] [CrossRef]
- Subrahmanyam, M. Storage of skin grafts in honey. Lancet 1993, 341, 63–64. [Google Scholar] [CrossRef]
- Gregory, S.R.; Piccolo, N.; Piccolo, M.T.; Piccolo, M.S.; Heggers, J.P. Comparison of propolis skin cream to silver sulfadiazine: A naturopathic alternative to antibiotics in treatment of minor burns. J. Altern. Complem. Med. 2002, 8, 77–83. [Google Scholar] [CrossRef]
- Pessolato, A.G.; Martins Ddos, S.; Ambrósio, C.E.; Mançanares, C.A.; de Carvalho, A.F. Propolis and amnion reepithelialise second-degree burns in rats. Burns 2011, 37, 1192–1201. [Google Scholar] [CrossRef]
- Berretta, A.A.; Nascimento, A.P.; Bueno, P.C.; Vaz, M.M.; Marchetti, J.M. Propolis standardized extract (EPP-AF®), an innovative chemically and biologically reproducible pharmaceutical compound for treating wounds. Int. J. Biol. Sci. 2012, 8, 512–521. [Google Scholar]
- Cole, N.; Sou, P.W.; Ngo, A.; Tsang, K.H.; Severino, J.A.; Arun, S.J.; Duke, C.C.; Reeve, V.E. Topical Sydney propolis protects against UV-radiation-Induced inflammation, lipid peroxidation and immune suppression in mouse skin. Int. Arch. Allergy Immunol. 2010, 152, 87–97. [Google Scholar] [CrossRef]
- Al-Waili, N.S.; Saloom, K.Y. Effects of topical honey on post-operative wound infections due to Gram-positive and Gram-negative bacteria following Caesarean sections and hysterectomies. Eur. J. Med. Res. 1999, 4, 126–130. [Google Scholar]
- Subrahmanyam, M. A prospective randomized clinical and histological study of superficial burn wound healing with honey and silver sulfadiazine. Burns 1998, 24, 157–161. [Google Scholar] [CrossRef]
- Hoekstra, M.J.; Hupkens, P.; Dutrieux, R.P.; Bosch, M.M.C.; Brans, T.A.; Kreis, R.W. A comparative burn wound model in the New Yorkshire pig for the histopathological evaluation of local therapeutic regimens: silver sulfadiazine cream as a standard. Br. J. Plast. Surg. 1993, 46, 585–589. [Google Scholar] [CrossRef]
- Prockop, D.J.; Underfriend, S. A specific method for the analysis of hydroxyproline in tissues and urine. Anal. Biochem. 1960, 1, 228–239. [Google Scholar] [CrossRef]
- Sample Availability: Samples of the compounds are available from the authors.
© 2013 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Jastrzębska-Stojko, Ż.; Stojko, R.; Rzepecka-Stojko, A.; Kabała-Dzik, A.; Stojko, J. Biological Activity of Propolis-Honey Balm in the Treatment of Experimentally-Evoked Burn Wounds. Molecules 2013, 18, 14397-14413. https://doi.org/10.3390/molecules181114397
Jastrzębska-Stojko Ż, Stojko R, Rzepecka-Stojko A, Kabała-Dzik A, Stojko J. Biological Activity of Propolis-Honey Balm in the Treatment of Experimentally-Evoked Burn Wounds. Molecules. 2013; 18(11):14397-14413. https://doi.org/10.3390/molecules181114397
Chicago/Turabian StyleJastrzębska-Stojko, Żaneta, Rafał Stojko, Anna Rzepecka-Stojko, Agata Kabała-Dzik, and Jerzy Stojko. 2013. "Biological Activity of Propolis-Honey Balm in the Treatment of Experimentally-Evoked Burn Wounds" Molecules 18, no. 11: 14397-14413. https://doi.org/10.3390/molecules181114397
APA StyleJastrzębska-Stojko, Ż., Stojko, R., Rzepecka-Stojko, A., Kabała-Dzik, A., & Stojko, J. (2013). Biological Activity of Propolis-Honey Balm in the Treatment of Experimentally-Evoked Burn Wounds. Molecules, 18(11), 14397-14413. https://doi.org/10.3390/molecules181114397







