Cancers 2023, 15(6), 1631; https://doi.org/10.3390/cancers15061631 - 7 Mar 2023
Cited by 23 | Viewed by 3036
Abstract
The gastrin-releasing peptide receptor (GRPR) is overexpressed in prostate cancer (PCa) and in hormone-driven breast cancer (BCa). The aim of this phase I clinical trial was to evaluate safety, biodistribution, and dosimetry after the administration of the recently developed GRPR-targeting antagonistic bombesin analogue
[...] Read more.
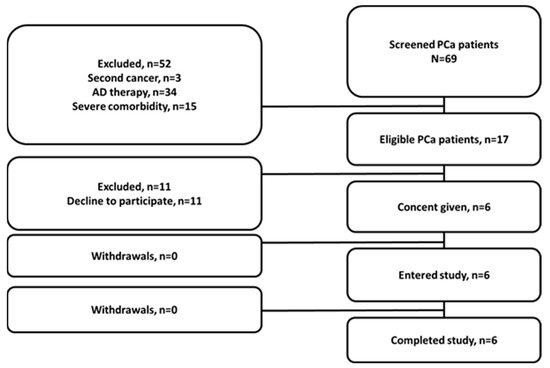
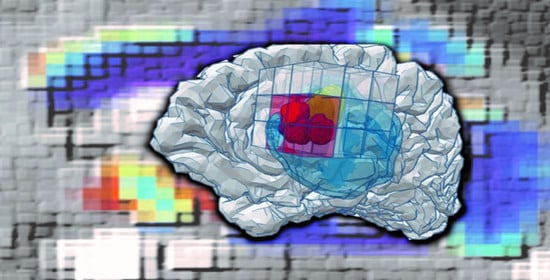
The gastrin-releasing peptide receptor (GRPR) is overexpressed in prostate cancer (PCa) and in hormone-driven breast cancer (BCa). The aim of this phase I clinical trial was to evaluate safety, biodistribution, and dosimetry after the administration of the recently developed GRPR-targeting antagonistic bombesin analogue [99mTc]Tc-maSSS-PEG2-RM26 in PCa and BCa patients. Planar and whole-body SPECT/CT imaging was performed in six PCa patients and seven BCa patients 2, 4, 6, and 24 h post the intravenous administration of 40 µg of [99mTc]Tc-maSSS-PEG2-RM26 (600–700 MBq). No adverse events or pathological changes were observed. The rapid blood clearance of [99mTc]Tc-maSSS-PEG2-RM26 was observed with predominantly hepatobiliary excretion. The effective doses were 0.0053 ± 0.0007 for male patients and 0.008 ± 0.003 mSv/MBq for female patients. The accumulation of [99mTc]Tc-maSSS-PEG2-RM26 in tumors was observed in four out of six PCa and in seven out of seven BCa patients. In four BCa patients, a high uptake of the agent into the axillary lymph nodes was detected. Immunohistochemistry revealed positive GRPR expression in 60% of primary PCa, 71.4% of BCa tumors, and 50% of examined BCa lymph nodes. In conclusion, a single administration of [99mTc]Tc-maSSS-PEG2-RM26 was safe and well tolerated. [99mTc]Tc-maSSS-PEG2-RM26 SPECT may be useful for tumor detection in PCa and BCa patients, pending further studies.
Full article
(This article belongs to the Special Issue Diagnostic and Treatment for Three Urological Cancers: Bladder Cancer, Kidney Cancer and Prostate Cancer)
►
Show Figures