A New Murine Highly Localized High-Dose Muscle Radiation Model as a Tool to Develop Innovative Countermeasures to Treat Radio-Induced Muscular Lesions †
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics, Animals, and Irradiation
2.2. Monitoring of Mice Post-Irradiation Status
2.3. Samples Collection and Analysis
2.4. Statistical Analysis
3. Results and Discussion
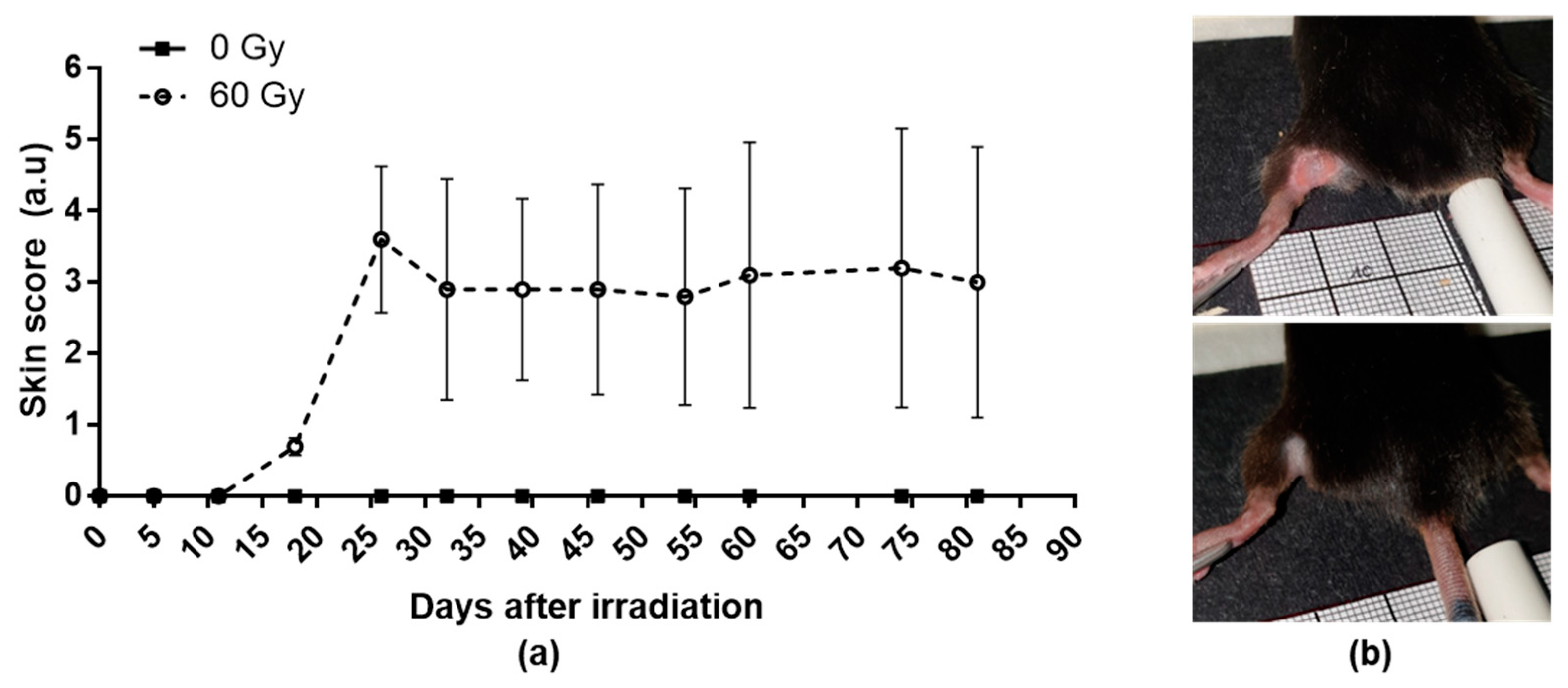
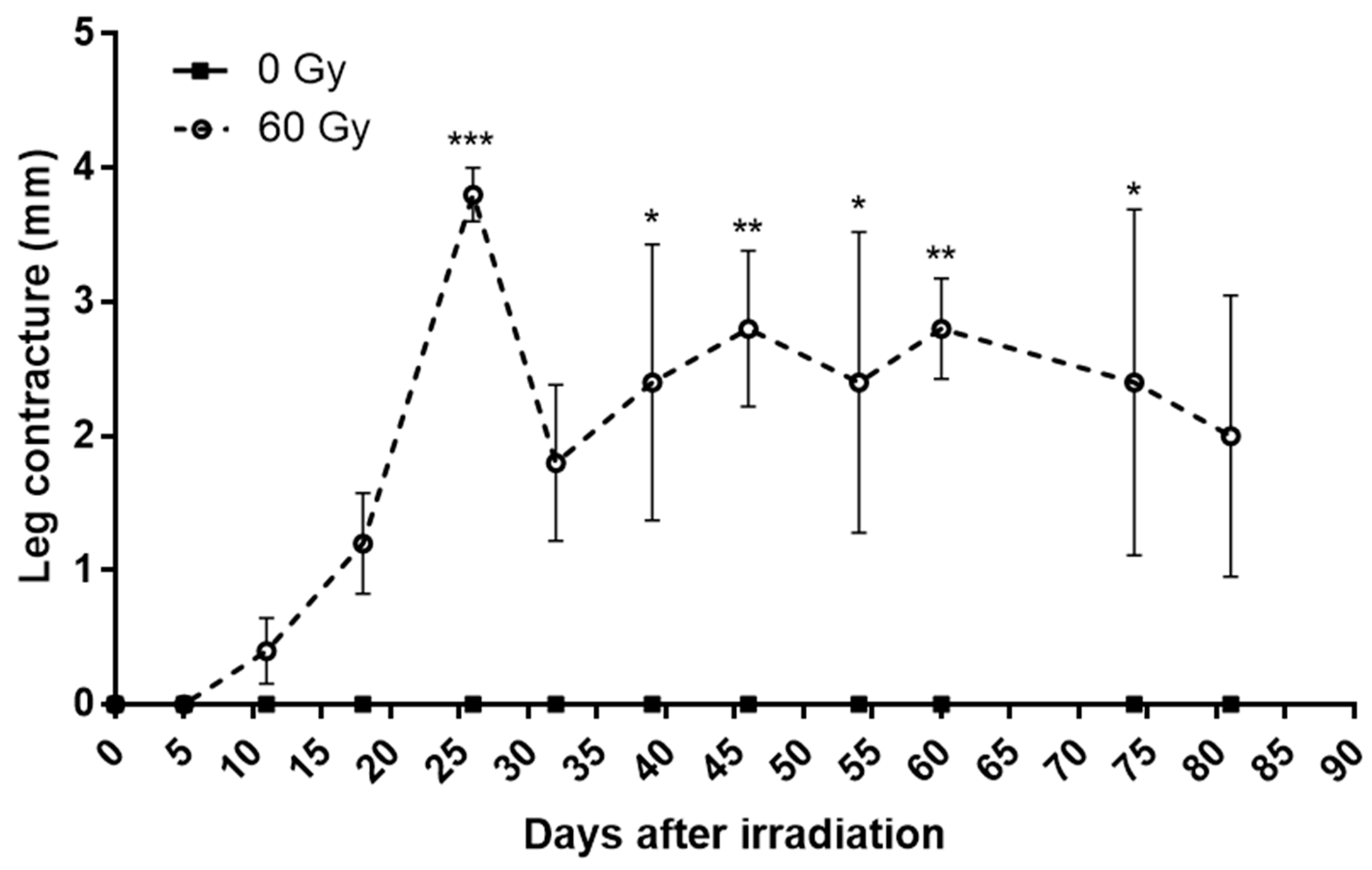
3.1. Radiation-Induced Skin Lesions and Leg Contracture
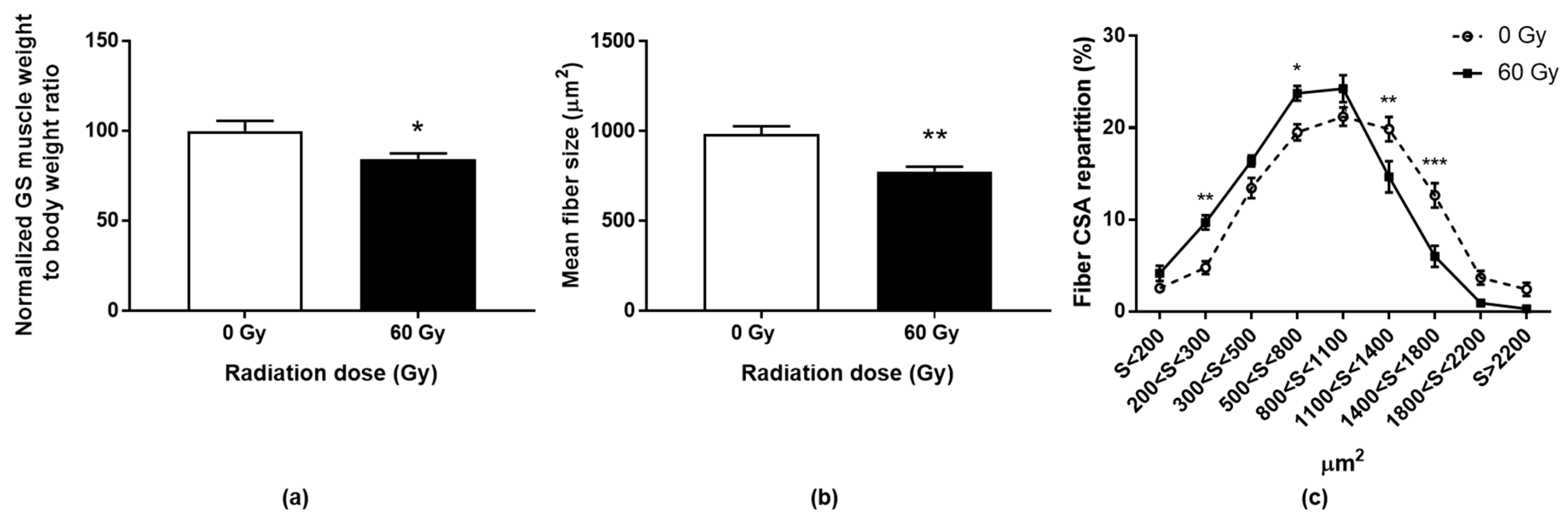
3.2. Muscle Weight and Size of Myofibers
3.3. Expression of Specific Genes after Radiation Exposure
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lefaix, J.L.; Delanian, S. Menace Terroriste Nucléaire: Approche Médicale; John Libbey Eurotext Plc: Arcueil, France, 2005; pp. 87–95. (In French) [Google Scholar]
- Hopewell, J.W. The Skin: Its Structure and Response to Ionizing Radiation. Int. J. Radiat. Biol. 1990, 57, 751–773. [Google Scholar] [CrossRef] [PubMed]
- Lataillade, J.; Doucet, C.; Bey, E.; Carsin, H.; Huet, C.; Clairand, I.; Bottollier-Depois, J.; Chapel, A.; Ernou, I.; Gourven, M.; et al. New approach to radiation burn treatment by dosimetry-guided surgery combined with autologous mesenchymal stem cell therapy. Regen. Med. 2007, 2, 785–794. [Google Scholar] [CrossRef] [PubMed]
- Bey, E.; Prat, M.; Duhamel, P.; Benderitter, M.; Brachet, M.; Trompier, F.; Battaglini, P.; Ernou, I.; Boutin, L.; Gourven, M.; et al. Emerging therapy for improving wound repair of severe radiation burns using local bone marrow-derived stem cell administrations. Wound Repair Regen. 2010, 18, 50–58. [Google Scholar] [CrossRef] [PubMed]
- Reyes, E.H.; Baciu, F.; Benderitter, M.; Lataillade, J.J.; Bey, E.; Trompier, F.; Tamarat, R. Medical Response to Radiological Accidents in Latin America and International Assistance. Radiat. Res. 2016, 185, 359–365. [Google Scholar] [CrossRef] [PubMed]
- Mauro, A. Satellite cell of skeletal muscle fibers. J. Cell Biol. 1961, 9, 493–495. [Google Scholar] [CrossRef] [PubMed]
- Zammit, P.S.; Partridge, T.A.; Yablonka-Reuveni, Z. The Skeletal Muscle Satellite Cell: The Stem Cell That Came in From the Cold. J. Histochem. Cytochem. 2006, 54, 1177–1191. [Google Scholar] [CrossRef] [PubMed]
- Hawke, T.J.; Garry, D.J. Myogenic satellite cells: Physiology to molecular biology. J. Appl. Physiol. 2001, 91, 534–551. [Google Scholar] [CrossRef] [PubMed]
- Linard, C.; Brachet, M.; L’Homme, B.; Strup-Perrot, C.; Busson, E.; Bonneau, M.; Lataillade, J.-J.; Bey, E.; Benderitter, M. Long-term effectiveness of local BM-MSCs for skeletal muscle regeneration: A proof of concept obtained on a pig model of severe radiation burn. Stem Cell Res. Ther. 2018, 9, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Riccobono, D.; Agay, D.; François, S.; Scherthan, H.; Drouet, M.; Forcheron, F. Contribution of INTRAMUSCULAR autologous adipose tissue-derived stem cell injections to treat cutaneous radiation syndrome: Preliminary results. Health Phys. 2016, 111, 117–126. [Google Scholar] [CrossRef]
- Hardee, J.P.; Puppa, M.J.; Fix, D.K.; Gao, S.; Hetzler, K.L.; Bateman, T.A.; Carson, J.A. The effect of radiation dose on mouse skeletal muscle remodeling. Radiol. Oncol. 2014, 48, 247–256. [Google Scholar] [CrossRef]
- Viana, W.; Lambertz, D.; Borges, E.; Melo, J.; Lambertz, K.; Amaral, A. Late Effects of Radiation on Skeletal Muscle: An Open Field of Research. J. Biomed. Sci. Eng. 2015, 08, 555–570. [Google Scholar] [CrossRef]
- Phulpin, B.; Dolivet, G.; Marie, P.-Y.; Poussier, S.; Gallet, P.; Leroux, A.; Graff, P.; Groubach, F.; Bravetti, P.; Merlin, J.-L.; et al. Re-assessment of chronic radio-induced tissue damage in a rat hindlimb model. Exp. Ther. Med. 2010, 1, 553–560. [Google Scholar] [CrossRef]
- E Wright, L.; Buijs, J.T.; Kim, H.-S.; E Coats, L.; Scheidler, A.M.; John, S.K.; She, Y.; Murthy, S.; Ma, N.; Chin-Sinex, H.J.; et al. Single-Limb Irradiation Induces Local and Systemic Bone Loss in a Murine Model. J. Bone Miner. Res. 2015, 30, 1268–1279. [Google Scholar] [CrossRef] [PubMed]
- Stone, H.B. Leg contracture in mice: An assay of normal tissue response. Int. J. Radiat. Oncol. 1984, 10, 1053–1061. [Google Scholar] [CrossRef]
- Riccobono, D.; Nikovics, K.; François, S.; Favier, A.-L.; Jullien, N.; Schrock, G.; Scherthan, H.; Drouet, M. First Insights Into the M2 Inflammatory Response After Adi-pose-Tissue-Derived Stem Cell Injections in Radiation-Injured Muscles. Health Phys. 2018, 115, 37–48. [Google Scholar] [CrossRef]
- Keller, A.; Demeurie, J.; Merkulova, T.; Gérard, G.; Charlotte, C.-G.; Marguerite, L.; François-Patrick, C. Fibre-type distribution and subcellular localisation of alpha and beta enolase in mouse striated muscle. Biol. Cell. 2000, 92, 527–535. [Google Scholar] [CrossRef]

| Score | |||||||
|---|---|---|---|---|---|---|---|
| 0 | 0.5 | 1 | 2 | 3 | 4 | 5 | |
| Depilation | None | slight | pronounced | ||||
| Erythema | None | slight redness | redness | pronounced redness | intense redness | burgundy to purple redness | |
| Edema | None | minor bulge | slight swelling | pronounced swelling | major swelling | phlyctena | |
| Exudation | None | slightly moist wound | oozing | marked exudation | impregnated hair around the wound | superinfection | |
| Ulcer/Necrosis | None | shallow ulcer / small necrosis | deep ulcer / significant necrosis | ||||
| Tendancy to spread | same or smaller area than at previous examination | moderate extension (<50% of the area at previous examination) | significant extension (>50% of the area at previous examination) | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jullien, N.; Graziosi, E.R.; Gauthier, M.; Drouet, M.; Francois, S.; Riccobono, D. A New Murine Highly Localized High-Dose Muscle Radiation Model as a Tool to Develop Innovative Countermeasures to Treat Radio-Induced Muscular Lesions. Med. Sci. Forum 2023, 21, 49. https://doi.org/10.3390/ECB2023-14280
Jullien N, Graziosi ER, Gauthier M, Drouet M, Francois S, Riccobono D. A New Murine Highly Localized High-Dose Muscle Radiation Model as a Tool to Develop Innovative Countermeasures to Treat Radio-Induced Muscular Lesions. Medical Sciences Forum. 2023; 21(1):49. https://doi.org/10.3390/ECB2023-14280
Chicago/Turabian StyleJullien, Nicolas, Emmanuelle Rota Graziosi, Michel Gauthier, Michel Drouet, Sabine Francois, and Diane Riccobono. 2023. "A New Murine Highly Localized High-Dose Muscle Radiation Model as a Tool to Develop Innovative Countermeasures to Treat Radio-Induced Muscular Lesions" Medical Sciences Forum 21, no. 1: 49. https://doi.org/10.3390/ECB2023-14280
APA StyleJullien, N., Graziosi, E. R., Gauthier, M., Drouet, M., Francois, S., & Riccobono, D. (2023). A New Murine Highly Localized High-Dose Muscle Radiation Model as a Tool to Develop Innovative Countermeasures to Treat Radio-Induced Muscular Lesions. Medical Sciences Forum, 21(1), 49. https://doi.org/10.3390/ECB2023-14280






