Endocarditis with Streptococcus pseudoporcinus Associated with Mastocytosis and Spondylodiscitis—A Coincidental Association? A Case Report
Abstract
:1. Introduction
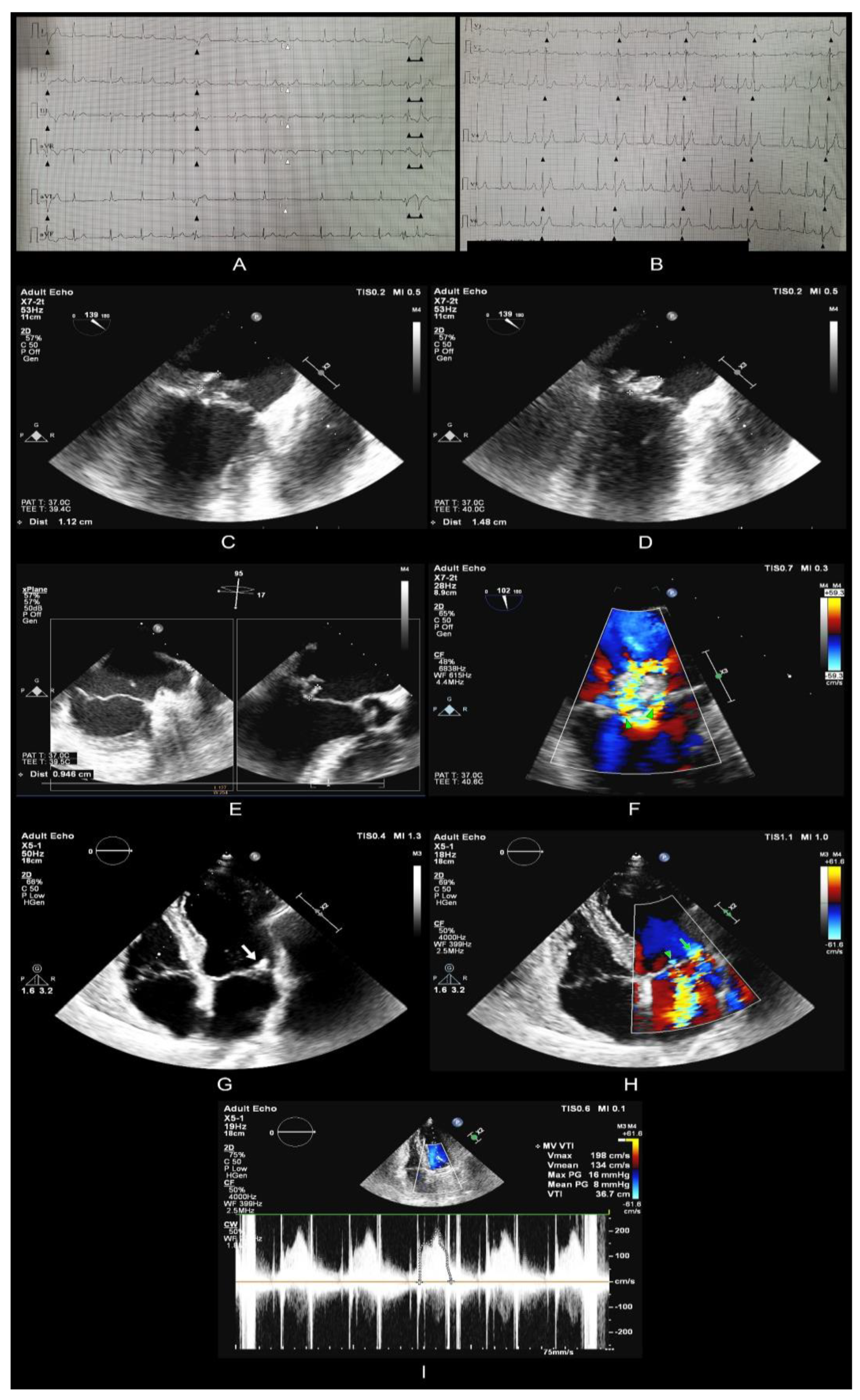
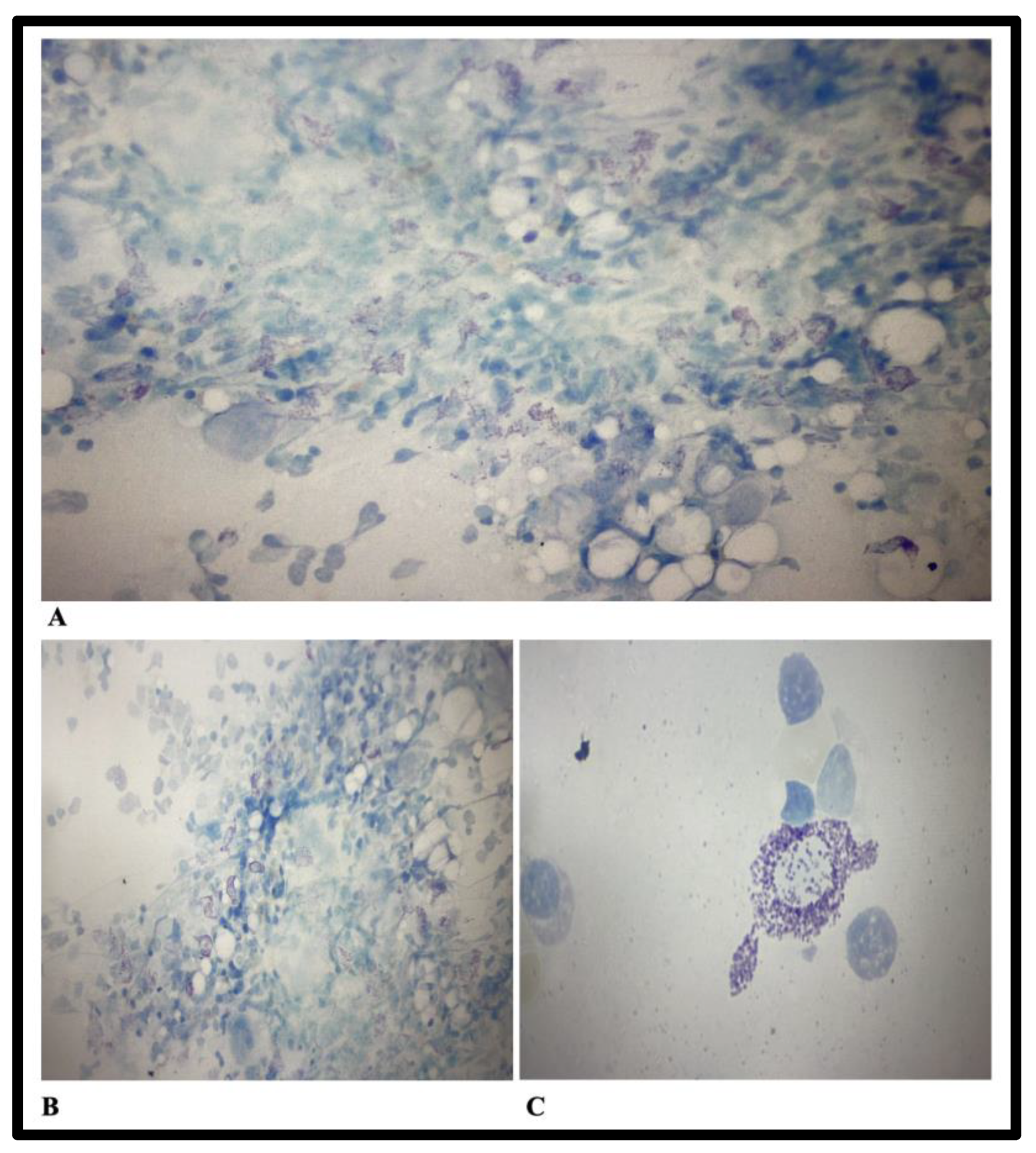
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mahlen, S.D.; Clarridge, J.E. III Thumb infection caused by Streptococcus pseudoporcinus. J. Clin. Microbiol. 2009, 47, 3041–3042. [Google Scholar] [CrossRef]
- Sawamura, S.; Niimori, D.; Ihn, H. A case of leg cellulitis caused by multidrug-resistant Streptococcus pseudoporcinus. Intractable Rare Dis. Res. 2018, 7, 280–282. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.; Wong, T.T.; Prasad, N.; Lee, B.; Urban, C.; Segal-Maurer, S.; Turett, G. Streptococcus pseudoporcinus: Case Reports and Review of the Literature. Case Rep. Infect. Dis. 2020, 2020, 4135246. [Google Scholar] [CrossRef] [PubMed]
- Hai, P.D.; Dung, N.M.; Son, P.N.; Phuong, L.L.; Thuyet, B.T.; Hoa, L.V. First report of infective endocarditis caused by Streptococcus pseudoporcinus in Vietnam. New Microbes New Infect. 2020, 34, 100643. [Google Scholar] [CrossRef] [PubMed]
- Gupta, K.; Mohanty, M.; Rath, S. Bacteremia because of Streptococcus pseudoporcinus in a Syphilis-HIV co-infected patient: A case report. J. Fam. Med. Prim. Care 2020, 9, 2119–2120. [Google Scholar] [CrossRef]
- Vergadi, E.; Goniotakis, I.; Maraki, S.; Galanakis, E. Extensive Cellulitis and Bacteremia Due to Streptococcus Pseudoporcinus in a Child With Klippel-Trenaunay Syndrome. Pediatr. Infect. Dis. J. 2021, 40, e316–e318. [Google Scholar] [CrossRef]
- Liatsos, G.D.; Tsiriga, A.; Dourakis, S.P. Fatal Streptococcus pseudoporcinus disseminated infection in decompensated liver cirrhosis: A case report. J. Med. Case Rep. 2021, 15, 240. [Google Scholar] [CrossRef]
- Dong, Y.; Tian, M. Case Report: Corneal perforation secondary to orbital cellulitis caused by Streptococcus pseudoporcinus infection. Eur. J. Ophthalmol. 2022, 4, 11206721221085210. [Google Scholar] [CrossRef]
- Facklam, R.; Elliott, J.; Pigott, N.; Franklin, A.R. Identification of Streptococcus porcinus from human sources. J. Clin. Microbiol. 1995, 33, 385–388. [Google Scholar] [CrossRef]
- Bekal, S.; Gaudreau, C.; Laurence, R.A.; Simoneau, E.; Raynal, L. Streptococcus pseudoporcinus sp. nov., a novel species isolated from the genitourinary tract of women. J. Clin. Microbiol. 2006, 44, 2584–2586. [Google Scholar] [CrossRef]
- Gaudreau, C.; Simoneau, E.; Labrecque, O.; Laurence, R.A.; Laferrière, C.; Miller, M.; Raynal, L.; Rallu, F. Epidemiological, biochemical and antimicrobial susceptibility characteristics of Streptococcus pseudoporcinus isolated in Quebec, Canada, from 1997 to 2006. J. Med. Microbiol. 2007, 56 Pt 12, 1620–1624. [Google Scholar] [CrossRef]
- Martin, C.; Fermeaux, V.; Eyraud, J.L.; Aubard, Y. Streptococcus porcinus as a cause of spontaneous preterm human stillbirth. J. Clin. Microbiol. 2004, 42, 4396–4398. [Google Scholar] [CrossRef] [PubMed]
- Stoner, K.A.; Rabe, L.K.; Austin, M.N.; Meyn, L.A.; Hillier, S.L. Incidence and epidemiology of Streptococcus pseudoporcinus in the genital tract. J. Clin. Microbiol. 2011, 49, 883–886. [Google Scholar] [CrossRef] [PubMed]
- Grundy, M.; Suwantarat, N.; Rubin, M.; Harris, R.; Hanlon, A.; Tekle, T.; Ellis, B.; Carroll, K.; Witter, F. Differentiating Streptococcus pseudoporcinus from GBS: Could this have implications in pregnancy? Am. J. Obstet. Gynecol. 2019, 220, 490.e1–490.e7. [Google Scholar] [CrossRef]
- Akagi, M.; Iwanaga, N.; Torisu, Y.; Fujita, H.; Kawahara, C.; Horai, Y.; Izumi, Y.; Kawakami, A. IgA Vasculitis Triggered by Infective Endocarditis of Pulmonary Artery with Congenitally Corrected Transposition of the Great Arteries. Int. Heart J. 2020, 61, 404–408. [Google Scholar] [CrossRef] [PubMed]
- Pierce, S.L.; Shibib, D.R.; Robison, D.; Edwards, R.K. A case of maternal sepsis and fetal demise associated with Streptococcus pseudoporcinus. Case Rep. Obstet. Gynecol. 2019, 2019, 4309191. [Google Scholar] [CrossRef] [PubMed]
- Wolff, K.; Komar, M.; Petzelbauer, P. Clinical and histopathological aspects of cutaneous mastocytosis. Leuk. Res. 2001, 25, 519–528. [Google Scholar] [CrossRef]
- Kounis, N.G.; Zavras, G.M. Histamine-induced coronary artery spasm: The concept of allergic angina. Br. J. Clin. Pract. 1991, 45, 121–128. [Google Scholar]
- Abdelghany, M.; Subedi, R.; Shah, S.; Kozman, H. Kounis syndrome: A review article on epidemiology, diagnostic findings, management and complications of allergic acute coronary syndrome. Int. J. Cardiol. 2017, 232, 1–4. [Google Scholar] [CrossRef]
- Broesby-Olsen, S.; Farkas, D.K.; Vestergaard, H.; Hermann, A.P.; Møller, M.B.; Mortz, C.G.; Kristensen, T.K.; Bindslev-Jensen, C.; Sørensen, H.T.; Frederiksen, H. Risk of solid cancer, cardiovascular disease, anaphylaxis, osteoporosis and fractures in patients with systemic mastocytosis: A nationwide population-based study. Am. J. Hematol. 2016, 91, 1069–1075. [Google Scholar] [CrossRef]
- Paratz, E.D.; Khav, N.; Burns, A.T. Systemic Mastocytosis, Kounis Syndrome and Coronary Intervention: Case Report and Systematic Review. Heart Lung Circ. 2017, 26, 772–778. [Google Scholar] [CrossRef] [PubMed]
- Kokkonen, J.O.; Kovanen, P.T. Stimulation of mast cells leads to cholesterol accumulation in macrophages in vitro by a mast cell granule-mediated uptake of low density lipoprotein. Proc. Natl. Acad. Sci. USA 1987, 84, 2287–2291. [Google Scholar] [CrossRef] [PubMed]
- Kovanen, P.T. Mast Cell Granule-Mediated Uptake of Low Density Lipoproteins by Macrophages: A Novel Carrier Mechanism Leading to the Formation of Foam Cells. Ann. Med. 1991, 23, 551–559. [Google Scholar] [CrossRef] [PubMed]
- Valent, P.; Akin, C.; Hartmann, K.; Alvarez-Twose, I.; Brockow, K.; Hermine, O.; Niedoszytko, M.; Schwaab, J.; Lyons, J.J.; Carter, M.C.; et al. Updated Diagnostic Criteria and Classification of Mast Cell Disorders: A Consensus Proposal. Hemasphere 2021, 5, e646. [Google Scholar] [CrossRef] [PubMed]
- Peir-Yu, F.; Gandhi, S.A. Streptococcus pseudoporcinus subacute mitral valve endocarditis: A case report. Int. J. Case Rep. Images 2017, 8, 105–107. [Google Scholar]
- Cancan Gursul, N.; Ozdemir, E. Streptococcus porcinus Endocarditis: The First Reported Case In Humans. Eskisehir Med. J. 2022, 3, 1–4. [Google Scholar] [CrossRef]

| Date | Parameter | Values | Reference Value |
|---|---|---|---|
| On admission | C-Reactive Protein | 114.81 mg/L | 0–5 mg/L |
| Fibrinogen | 514 mg/dL | 170–420 mg/dL | |
| WBCs | 14.70 × 103/µL | 4.2–7.5 × 103/µL | |
| Differential blood count: | |||
| Neutrophils | 11.77 × 103/µL | 10 × 103/µL | |
| Lymphocytes | 1.91 × 103/µL | 1.5–4 × 03/µL | |
| Monocytes | 0.95 × 103/µL | 0.2–1 × 103/µL | |
| Basophils | 0.02 × 103/µL | 0–0.2 × 103/µL | |
| Eosinophils | 0.05 × 103/µL | 0–0.7 × 103/µL | |
| Red Blood Cells | 3.35 × 106/µL | 4.5–5.8 × 106/ µL | |
| Haemoglobin | 10.3 g/dL | 13–17 g/dL | |
| Hematocrit | 30.6% | 40–50% | |
| Thrombocytes | 170 × 103/uL | 150–400 × 103/uL | |
| Coagulation tests | Prothrombin time (PT): | ||
| 13.9 | 9.9–12.3 s | ||
| Activated partial thromboplastin time (aPTT): | |||
| 30.9 | 25.1–37.7 s | ||
| International normalized ratio (INR): | |||
| 1.10 | 0.86–1.1 | ||
| Serum protein electrophoresis: | |||
| Albumin | 50.1% | 54.3–65.5% | |
| Alpha-1 globulins | 4.1% | 1.2–3.3% | |
| Alpha-2 globulins | 9.1% | 8.3–15% | |
| Beta- globulins | 13.7% | 8.6–14.8% | |
| Gamma- globulins | 23% | 7.1–19.5% | |
| IgA | 432 mg/dL | 70–400 mg/dL | |
| IgG | 1661 mg/dL | 700–1600 mg/dL | |
| IgM | 133 mg/dL | 40–230 mg/dL | |
| ESR* | 74 mm/h | 0–15 mm/h | |
| Urea | 34 mg/dL | 18–55 mg/dL | |
| Creatinine | 0.95 mg/dL | 0.72–1.25 mg/dL | |
| Blood glucose | 128 mg/dL | 80–115 mg/dL | |
| Urinalysis | Color —Yellow Clarity/turbidity—Clear pH—5.5 Specific gravity—1.015 Glucose—125 mg/d Ketones—None Nitrites—Negative Bilirubin—Negative Urobilirubin—Normal Blood—Negative Protein—100 mg/d RBCs—1–2 RBCs/hpf WBCs—2–3 WBCs/hpf Squamous epithelial cells—5–10 squamous epithelial cells/hpf | ||
| Urine Culture | E. coli >100,000 CFU/ML | ||
| HIV-1/HIV-2 Antibody Test | Negative | ||
| Rapid plasma reagin | Negative | ||
| 12 days after admission | C-Reactive Protein | 26.77 mg/L | |
| Fibrinogen | 364 mg/dL | ||
| WBCs | 18.69 × 103/µL | ||
| Haemoglobin | 11.4 g/dL | ||
| Hematocrit | 34.4 % | ||
| Thrombocytes | 155 × 103/µL | ||
| 19 days after admission | C-Reactive Protein | 26.45 mg/L | |
| Fibrinogen | 443.9 mg/dL | ||
| WBCs | 14.93 × 103/µL | ||
| Haemoglobin | 11.8 g/dL | ||
| Hematocrit | 35.8 % | ||
| Thrombocytes | 187 × 103/µL | ||
| ESR * | 16 mm/h |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Birlutiu, V.; Birlutiu, R.-M.; Teodoru, M.; Catana, A.C.; Stoica, C.I. Endocarditis with Streptococcus pseudoporcinus Associated with Mastocytosis and Spondylodiscitis—A Coincidental Association? A Case Report. Trop. Med. Infect. Dis. 2023, 8, 247. https://doi.org/10.3390/tropicalmed8050247
Birlutiu V, Birlutiu R-M, Teodoru M, Catana AC, Stoica CI. Endocarditis with Streptococcus pseudoporcinus Associated with Mastocytosis and Spondylodiscitis—A Coincidental Association? A Case Report. Tropical Medicine and Infectious Disease. 2023; 8(5):247. https://doi.org/10.3390/tropicalmed8050247
Chicago/Turabian StyleBirlutiu, Victoria, Rares-Mircea Birlutiu, Minodora Teodoru, Alina Camelia Catana, and Cristian Ioan Stoica. 2023. "Endocarditis with Streptococcus pseudoporcinus Associated with Mastocytosis and Spondylodiscitis—A Coincidental Association? A Case Report" Tropical Medicine and Infectious Disease 8, no. 5: 247. https://doi.org/10.3390/tropicalmed8050247





