Maternal Antibiotic Exposure and the Risk of Developing Antenatal or Postpartum Depressive Symptoms: The Maternal Experience Study Protocol
Abstract
:1. Introduction
Aims
2. Methods and Design
2.1. Study Design and Setting
2.2. Inclusion and Exclusion Criteria
2.3. Sample Size Calculation
2.4. Recruitment
3. Procedure
3.1. Data Collection
3.2. Ethics Consideration
3.3. Data Management
3.4. Data Analysis and Plan
- The antenatal period (from ~0 weeks gestation to mid-late third trimester);
- The perinatal period (from mid-late third trimester to 6 weeks postpartum);
- The postpartum period (from 6 weeks to 6 months postpartum and from 6 months to 12 months postpartum).
4. Discussion
Strengths and Limitations of This Study
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Depression and Other Common Mental Disorders Global Health Estimates. Available online: https://apps.who.int/iris/bitstream/handle/10665/254610/WHO-MSD-MER-2017.2-eng.pdf (accessed on 16 April 2020).
- Australian Bureau of Statistics. Mental Health. Available online: https://www.abs.gov.au/statistics/health/mental-health/mental-health/latest-release (accessed on 29 September 2023).
- Barandouzi, Z.A.; Starkweather, A.R.; Henderson, W.A.; Gyamfi, A.; Cong, X.S. Altered Composition of Gut Microbiota in Depression: A Systematic Review. Front. Psychiatry 2020, 11, 541. [Google Scholar] [CrossRef] [PubMed]
- Limbana, T.; Khan, F.; Eskander, N. Gut Microbiome and Depression: How Microbes Affect the Way We Think. Cureus 2020, 12, e9966. [Google Scholar] [CrossRef] [PubMed]
- Lurie, I.; Yang, Y.X.; Haynes, K.; Mamtani, R.; Boursi, B. Antibiotic exposure and the risk for depression, anxiety, or psychosis: A nested case-control study. J. Clin. Psychiatry 2015, 76, 1522–1528. [Google Scholar] [CrossRef] [PubMed]
- Hu, K.; Smedby, K.E.; Sjölander, A.; Montgomery, S.; Valdimarsdóttir, U.; Engstrand, L.; Fang, F.; Fall, K. Use of Antibiotics and Risk of Psychiatric Disorders in Newly Diagnosed Cancer Patients: A Population-Based Cohort Study in Sweden. Cancer Epidemiol. Biomark. Prev. 2022, 31, 528–535. [Google Scholar] [CrossRef]
- Pouranayatihosseinabad, M.; Bezabih, Y.; Hawrelak, J.; Peterson, G.M.; Veal, F.; Mirkazemi, C. Antibiotic use and the development of depression: A systematic review. J. Psychosom. Res. 2022, 164, 111113. [Google Scholar] [CrossRef]
- McCloskey, K.; Vuillermin, P.; Carlin, J.B.; Cheung, M.; Skilton, M.R.; Tang, M.L.; Allen, K.; Gilbert, G.L.; Ranganathan, S.; Collier, F.; et al. Perinatal microbial exposure may influence aortic intima-media thickness in early infancy. Int. J. Epidemiol. 2017, 46, 209–218. [Google Scholar] [CrossRef]
- Baraka, M.A.; AlLehaibi, L.H.; AlSuwaidan, H.N.; Alsulaiman, D.; Islam, M.A.; Alotaibi, B.S.; Alboghdadly, A.; Homoud, A.H.; Al-Ghamdi, F.H.; Al Ghamdi, M.S.; et al. Patterns of infections and antimicrobial drugs’ prescribing among pregnant women in Saudi Arabia: A cross sectional study. J. Pharm. Policy Pract. 2021, 14, 9. [Google Scholar] [CrossRef]
- Ahnfeldt-Mollerup, P.; Petersen, L.K.; Kragstrup, J.; Christensen, R.D.; Sørensen, B. Postpartum infections: Occurrence, healthcare contacts and association with breastfeeding. Acta Obstet. Gynecol. Scand. 2012, 91, 1440–1444. [Google Scholar] [CrossRef]
- Intra-Amniotic Infection (Chorioamnionitis). In Therapeutic Guidelines; Therapeutic Guidelines Limited: Melbourne; Available online: https://www.tg.org.au/ (accessed on 29 September 2023).
- Prophylaxis for Preterm Prelabour Rupture of Membranes. In Therapeutic Guidelines; Therapeutic Guidelines Limited: Melbourne; Available online: https://www.tg.org.au/ (accessed on 29 September 2023).
- Prevention of Neonatal Streptococcus Agalactiae (Group B Streptococcus) Disease. In Therapeutic Guidelines; Therapeutic Guidelines Limited: Melbourne; Available online: https://www.tg.org.au/ (accessed on 29 September 2023).
- Khanlari, S.; Eastwood, J.; Barnett, B.; Naz, S.; Ogbo, F.A. Psychosocial and obstetric determinants of women signalling distress during Edinburgh Postnatal Depression Scale (EPDS) screening in Sydney, Australia. BMC Pregnancy Childbirth 2019, 19, 407. [Google Scholar] [CrossRef]
- Milgrom, J.; Gemmill, A.W.; Bilszta, J.L.; Hayes, B.; Barnett, B.; Brooks, J.; Ericksen, J.; Ellwood, D.; Buist, A. Antenatal risk factors for postnatal depression: A large prospective study. J. Affect. Disord. 2008, 108, 147–157. [Google Scholar] [CrossRef]
- Woolhouse, H.; Gartland, D.; Mensah, F.; Brown, S.J. Maternal depression from early pregnancy to 4 years postpartum in a prospective pregnancy cohort study: Implications for primary health care. BJOG Int. J. Obstet. Gynaecol. 2015, 122, 312–321. [Google Scholar] [CrossRef] [PubMed]
- Robertson, E.; Celasun, N.; Stewart, D.E. Risk Factors for Postpartum Depression. Available online: https://madriella.org/wp-content/uploads/2019/11/WHO-PPD.pdf (accessed on 5 June 2020).
- Peduzzi, P.; Concato, J.; Kemper, E.; Holford, T.R.; Feinstein, A.R. A simulation study of the number of events per variable in logistic regression analysis. J. Clin. Epidemiol. 1996, 49, 1373–1379. [Google Scholar] [CrossRef] [PubMed]
- Brown, S.J.; Lumley, J.M.; McDonald, E.A.; Krastev, A.H. Maternal health study: A prospective cohort study of nulliparous women recruited in early pregnancy. BMC Pregnancy Childbirth 2006, 6, 12. [Google Scholar] [CrossRef] [PubMed]
- Durankuş, F.; Aksu, E. Effects of the COVID-19 pandemic on anxiety and depressive symptoms in pregnant women: A preliminary study. J. Matern. Fetal Neonatal Med. 2020, 35, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Holmes, T.H.; Rahe, R.H. The Social Readjustment Rating Scale. J. Psychosom. Res. 1967, 11, 213–218. [Google Scholar] [CrossRef]
- Bower, C.; Elliott, E.J. Australian Guide to Diagnosis of Fetal Alcohol Spectrum Disorder (FASD). Available online: https://www.fasdhub.org.au/siteassets/pdfs/australian-guide-to-diagnosis-of-fasd_all-appendices.pdf (accessed on 1 September 2020).
- Brockington, I.F.; Oates, J.; George, S.; Turner, D.; Vostanis, P.; Sullivan, M.; Loh, C.; Murdoch, C. A Screening Questionnaire for mother-infant bonding disorders. Arch. Women’s Ment. Health 2001, 3, 133–140. [Google Scholar] [CrossRef]
- Hegarty, K.; Fracgp; Bush, R.; Sheehan, M. The composite abuse scale: Further development and assessment of reliability and validity of a multidimensional partner abuse measure in clinical settings. Violence Vict. 2005, 20, 529–547. [Google Scholar] [CrossRef]
- Woolhouse, H.; Gartland, D.; Hegarty, K.; Donath, S.; Brown, S.J. Depressive symptoms and intimate partner violence in the 12 months after childbirth: A prospective pregnancy cohort study. BJOG Int. J. Obstet. Gynaecol. 2012, 119, 315–323. [Google Scholar] [CrossRef]
- Snyder, E.; Cai, B.; DeMuro, C.; Morrison, M.F.; Ball, W. A New Single-Item Sleep Quality Scale: Results of Psychometric Evaluation in Patients With Chronic Primary Insomnia and Depression. J. Clin. Sleep. Med. 2018, 14, 1849–1857. [Google Scholar] [CrossRef]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 1987, 150, 782–786. [Google Scholar] [CrossRef]
- Norhayati, M.N.; Hazlina, N.H.; Asrenee, A.R.; Emilin, W.M. Magnitude and risk factors for postpartum symptoms: A literature review. J. Affect. Disord. 2015, 175, 34–52. [Google Scholar] [CrossRef] [PubMed]
- The Royal Australian and New Zealand College of Obstetricians and Gynaecologists. Mental Health Care in the Perinatal Period. Available online: https://ranzcog.edu.au/RANZCOG_SITE/media/RANZCOG-MEDIA/Women%27s%20Health/Statement%20and%20guidelines/Clinical-Obstetrics/Mental-health-care-in-the-perinatal-period-(C-Obs-48).pdf?ext=.pdf (accessed on 19 June 2020).
- Bunevicius, A.; Kusminskas, L.; Pop, V.J.; Pedersen, C.A.; Bunevicius, R. Screening for antenatal depression with the Edinburgh Depression Scale. BJOG Int. J. Obstet. Gynaecol. 2009, 30, 238–243. [Google Scholar] [CrossRef] [PubMed]
- Lovibond, P.F.; Lovibond, S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- Lovibond, S.H.; Lovibond, P.F. Manual for the Depression Anxiety Stress Scales, 2nd ed.; Psychology Foundation of Australia: Sydney, NSW, Australia, 1995. [Google Scholar]
- Kocalevent, R.D.; Berg, L.; Beutel, M.E.; Hinz, A.; Zenger, M.; Härter, M.; Nater, U.; Brähler, E. Social support in the general population: Standardization of the Oslo social support scale (OSSS-3). BMC Psychol. 2018, 6, 31. [Google Scholar] [CrossRef]
- Aasheim, V.; Waldenström, U.; Hjelmstedt, A.; Rasmussen, S.; Pettersson, H.; Schytt, E. Associations between BJOG Int. J. Obstet. Gynaecol. maternal age and psychological distress in primiparous women, from early pregnancy to 18 months postpartum. BJOG 2012, 119, 1108–1116. [Google Scholar] [CrossRef]
- Katon, W.; Russo, J.; Gavin, A. Predictors of Postpartum Depression. J. Womens Health 2014, 23, 753–759. [Google Scholar] [CrossRef] [PubMed]
- Luciano, M.; Di Vincenzo, M.; Brandi, C.; Tretola, L.; Toricco, R.; Perris, F.; Volpicelli, A.; Torella, M.; La Verde, M.; Fiorillo, A.; et al. Does antenatal depression predict post-partum depression and obstetric complications? Results from a longitudinal, long-term, real-world study. Front. Psychiatry 2022, 13, 1082762. [Google Scholar] [CrossRef] [PubMed]
- Molyneaux, E.; Pasupathy, D.; Kenny, L.C.; McCowan, L.M.E.; North, R.A.; Dekker, G.A.; Walker, J.J.; Baker, P.N.; Poston, L.; Howard, L.M. Socio-economic status influences the relationship between obesity and antenatal depression: Data from a prospective cohort study. J. Affect. Disord. 2016, 202, 124–127. [Google Scholar] [CrossRef]
- Molyneaux, E.; Poston, L.; Khondoker, M.; Howard, L.M. Obesity, antenatal depression, diet and gestational weight gain in a population cohort study. Arch. Women’s Mental Health 2016, 19, 899–907. [Google Scholar] [CrossRef]
- Silverman, M.E.; Smith, L.; Lichtenstein, P.; Reichenberg, A.; Sandin, S. The association between body mass index and postpartum depression: A population-based study. J. Affect. Disord. 2018, 240, 193–198. [Google Scholar] [CrossRef]
- Ngocho, J.S.; Minja, L.M.; Mwamba, R.N.; Knettel, B.A.; Kisigo, G.A.; Mmbaga, B.T.; Watt, M.H. Prevalence and predictors of depression among women attending antenatal care in Moshi, Tanzania: A cross-sectional study. BMC Pregnancy Childbirth 2022, 22, 594. [Google Scholar] [CrossRef] [PubMed]
- Beck, C.T. Predictors of postpartum depression: An update. Nurs. Res. 2001, 50, 275–285. [Google Scholar] [CrossRef]
- Silva, R.; Jansen, K.; Souza, L.; Quevedo, L.; Barbosa, L.; Moraes, I.; Horta, B.; Pinheiro, R. Sociodemographic risk factors of perinatal depression: A cohort study in the public health care system. Braz. J. Psychiatry 2012, 34, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Ogbo, F.A.; Eastwood, J.; Hendry, A.; Jalaludin, B.; Agho, K.E.; Barnett, B.; Page, A. Determinants of antenatal depression and postnatal depression in Australia. BMC Psychiatry 2018, 18, 49. [Google Scholar] [CrossRef] [PubMed]
- Kornfeind, K.R.; Sipsma, H.L. Exploring the Link between Maternity Leave and Postpartum Depression. Womens Health Issues 2018, 28, 321–326. [Google Scholar] [CrossRef]
- Van Niel, M.S.; Bhatia, R.; Riano, N.S.; de Faria, L.; Catapano-Friedman, L.; Ravven, S.; Weissman, B.; Nzodom, C.; Alexander, A.; Budde, K.; et al. The Impact of Paid Maternity Leave on the Mental and Physical Health of Mothers and Children: A Review of the Literature and Policy Implications. Harv. Rev. Psychiatry 2020, 28, 113–126. [Google Scholar] [CrossRef] [PubMed]
- Yoo, H.; Ahn, S.; Park, S.; Kim, J.; Oh, J.; Koh, M. Factors influencing prenatal and postpartum depression in Korea: A prospective cohort study. Korean J. Women Health Nurs. 2021, 27, 326–336. [Google Scholar] [CrossRef] [PubMed]
- Maila, B.; Paul, R.; Mayimbo, S.; Kabwita, K. Prevalence and correlates of antenatal depression at Chelstone First Level Hospital in Lusaka, Zambia: A cross-sectional study. Afr. Health Sci. 2022, 22, 334–347. [Google Scholar] [CrossRef]
- Oboro, O.F.; Ebulue, V.; Oboro, V.O.; Ohenhen, V.; Oyewole, A.; Akindele, R.; Ala, O.; Oyeniran, O.; Isawumi, A.; Afolabi, B. The magnitude and determinants of depressive symptoms amongst women in early pregnancy in Southern Nigeria: A cross-sectional study. S. Afr. J. Psychiatr. 2022, 28, 1691. [Google Scholar] [CrossRef]
- Nakamura, A.; van der Waerden, J.; Melchior, M.; Bolze, C.; El-Khoury, F.; Pryor, L. Physical activity during pregnancy and postpartum depression: Systematic review and meta-analysis. J. Affect. Disord. 2019, 246, 29–41. [Google Scholar] [CrossRef]
- Vargas-Terrones, M.; Barakat, R.; Santacruz, B.; Fernandez-Buhigas, I.; Mottola, M.F. Physical exercise programme during pregnancy decreases perinatal depression risk: A randomised controlled trial. Br. J. Sports Med. 2019, 53, 348–353. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Guo, N.; Li, T.; Zhuang, W.; Jiang, H. Prevalence and Associated Factors of Postpartum Anxiety and Depression Symptoms Among Women in Shanghai, China. J. Affect. Disord. 2020, 274, 848–856. [Google Scholar] [CrossRef] [PubMed]
- Ross, L.E.; Dennis, C.L. The prevalence of postpartum depression among women with substance use, an abuse history, or chronic illness: A systematic review. J. Womens Health 2009, 18, 475–486. [Google Scholar] [CrossRef]
- Hutchens, B.F.; Kearney, J. Risk Factors for Postpartum Depression: An Umbrella Review. J. Midwifery Womens Health 2020, 65, 96–108. [Google Scholar] [CrossRef] [PubMed]
- Gaillard, A.; Le Strat, Y.; Mandelbrot, L.; Keïta, H.; Dubertret, C. Predictors of postpartum depression: Prospective study of 264 women followed during pregnancy and postpartum. Psychiatry Res. 2014, 215, 341–346. [Google Scholar] [CrossRef]
- Beck, C.T. A meta-analysis of predictors of postpartum depression. Nurs. Res. 1996, 45, 297–303. [Google Scholar] [CrossRef]
- Urbanová, E.; Škodová, Z.; Bašková, M. The Association between Birth Satisfaction and the Risk of Postpartum Depression. Int. J. Environ. Res. Public Health 2021, 18, 10458. [Google Scholar] [CrossRef]
- Vikström, J.; Sydsjö, G.; Hammar, M.; Bladh, M.; Josefsson, A. Risk of postnatal depression or suicide after in vitro fertilisation treatment: A nationwide case-control study. BJOG Int. J. Obstet. Gynaecol. 2017, 124, 435–442. [Google Scholar] [CrossRef]
- Muchanga, S.M.J.; Eitoku, M.; Mbelambela, E.P.; Ninomiya, H.; Iiyama, T.; Komori, K.; Yasumitsu-Lovell, K.; Mitsuda, N.; Tozin, R.R.; Maeda, N.; et al. Association between nausea and vomiting of pregnancy and postpartum depression: The Japan Environment and Children’s Study. J. Psychosom. Obstet. Gynaecol. 2020, 43, 2–10. [Google Scholar] [CrossRef]
- Blom, E.A.; Jansen, P.W.; Verhulst, F.C.; Hofman, A.; Raat, H.; Jaddoe, V.W.; Coolman, M.; Steegers, E.A.; Tiemeier, H. Perinatal complications increase the risk of postpartum depression. The Generation R Study. BJOG Int. J. Obstet. Gynaecol. 2010, 117, 1390–1398. [Google Scholar] [CrossRef]
- Lara, M.A.; Navarrete, L.; Nieto, L. Prenatal predictors of postpartum depression and postpartum depressive symptoms in Mexican mothers: A longitudinal study. Arch. Women’s Mental Health 2016, 19, 825–834. [Google Scholar] [CrossRef] [PubMed]
- Qiu, X.; Zhang, S.; Sun, X.; Li, H.; Wang, D. Unintended pregnancy and postpartum depression: A meta-analysis of cohort and case-control studies. J. Psychosom. Res. 2020, 138, 110259. [Google Scholar] [CrossRef] [PubMed]
- Abebe, A.; Tesfaw, G.; Mulat, H.; Hibdye, G.; Yohannes, K. Postpartum depression and associated factors among mothers in Bahir Dar Town, Northwest Ethiopia. Ann. Gen. Psychiatry 2019, 18, 19. [Google Scholar] [CrossRef] [PubMed]
- Kızılırmak, A.; Calpbinici, P.; Tabakan, G.; Kartal, B. Correlation between postpartum depression and spousal support and factors affecting postpartum depression. Health Care Women Int. 2021, 42, 1325–1339. [Google Scholar] [CrossRef]
- Chalise, A.; Shrestha, G.; Paudel, S.; Poudyal, A.K. Antenatal depression and its associated factors among women of Godawari Municipality, Lalitpur, Nepal: A cross-sectional study. BMJ Open 2022, 12, e063513. [Google Scholar] [CrossRef]
- Umuziga, M.P.; Gishoma, D.; Hynie, M.; Nyirazinyoye, L. Antenatal depressive symptoms in rwanda: Rates, risk factors, and social support. BMC Pregnancy Childbirth 2022, 22, 193. [Google Scholar] [CrossRef]
- Lee, S.H.; Liu, L.C.; Kuo, P.C.; Lee, M.S. Postpartum depression and correlated factors in women who received in vitro fertilization treatment. J. Midwifery Women’s Health 2011, 56, 347–352. [Google Scholar] [CrossRef]
- Martínez-Galiano, J.M.; Hernández-Martínez, A.; Rodríguez-Almagro, J.; Delgado-Rodríguez, M.; Gómez-Salgado, J. Relationship between parity and the problems that appear in the postpartum period. Sci. Rep. 2019, 9, 11763. [Google Scholar] [CrossRef]
- Wyatt, S.; Ostbye, T.; De Silva, V.; Lakmali, P.; Long, Q. Predictors and occurrence of antenatal depressive symptoms in Galle, Sri Lanka: A mixed-methods cross-sectional study. BMC Pregnancy Childbirth 2021, 21, 758. [Google Scholar] [CrossRef]
- Caropreso, L.; de Azevedo Cardoso, T.; Eltayebani, M.; Frey, B.N. Preeclampsia as a risk factor for postpartum depression and psychosis: A systematic review and meta-analysis. Arch. Women’s Mental Health 2019, 23, 493–505. [Google Scholar] [CrossRef]
- Chen, Y.; Ismail, F.; Xiong, Z.; Li, M.; Chen, I.; Wen, S.W.; Xie, R.H. Association between perceived birth trauma and postpartum depression: A prospective cohort study in China. Int. J. Gynaecol. Obstet. 2022, 157, 598–603. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Wang, S.; Li, X.Q. Association between mode of delivery and postpartum depression: A systematic review and network meta-analysis. Aust. N. Z. J. Psychiatry 2020, 55, 588–601. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Ding, Y.; Ma, Y.; Xin, X.; Zhang, D. Cesarean section and risk of postpartum depression: A meta-analysis. J. Psychosom. Res. 2017, 97, 118–126. [Google Scholar] [CrossRef] [PubMed]
- Doke, P.P.; Vaidya, V.M.; Narula, A.P.S.; Datar, M.C.; Patil, A.V.; Panchanadikar, T.M.; Wagh, G.N. Assessment of difference in postpartum depression among caesarean and vaginally delivered women at 6-week follow-up in hospitals in Pune District, India: An observational cohort study. BMJ Open 2021, 11, e052008. [Google Scholar] [CrossRef] [PubMed]
- Hickey, A.R.; Ellwood, D.; Boyce, P.M.; Morris-Yates, A.D. Early discharge and risk for postnatal depression. Med. J. Aust. 1997, 167, 244–247. [Google Scholar] [CrossRef]
- Sword, W.; Kurtz Landy, C.; Thabane, L.; Watt, S.; Krueger, P.; Farine, D.; Foster, G. Is mode of delivery associated with postpartum depression at 6° weeks: A prospective cohort study. BJOG Int. J. Obstet. Gynaecol. 2011, 118, 966–977. [Google Scholar] [CrossRef]
- Murphy, J.R.; Paul, S.; Dunlop, A.L.; Corwin, E.J. Maternal peripartum antibiotic exposure and the risk of postpartum depression. Res. Nurs. Health 2018, 41, 369–377. [Google Scholar] [CrossRef]
- Slykerman, R.F.; Hood, F.; Wickens, K.; Thompson, J.M.D.; Barthow, C.; Murphy, R.; Kang, J.; Rowden, J.; Stone, P.; Crane, J.; et al. Effect of Lactobacillus rhamnosus HN001 in Pregnancy on Postpartum Symptoms of Depression and Anxiety: A Randomised Double-blind Placebo-controlled Trial. eBioMedicine 2017, 24, 159–165. [Google Scholar] [CrossRef]
- Robakis, T.; Williams, K.E.; Nutkiewicz, L.; Rasgon, N.L. Hormonal Contraceptives and Mood: Review of the Literature and Implications for Future Research. Curr. Psychiatry Rep. 2019, 21, 57. [Google Scholar] [CrossRef]
- Böttcher, B.; Radenbach, K.; Wildt, L.; Hinney, B. Hormonal contraception and depression: A survey of the present state of knowledge. Arch. Gynecol. Obstet. 2012, 286, 231–236. [Google Scholar] [CrossRef]
- Skovlund, C.W.; Mørch, L.S.; Kessing, L.V.; Lidegaard, Ø. Association of Hormonal Contraception With Depression. JAMA Psychiatry 2016, 73, 1154–1162. [Google Scholar] [CrossRef]
- Wang, H.; Chen, M.; Xin, T.; Tang, K. Number of children and the prevalence of later-life major depression and insomnia in women and men: Findings from a cross-sectional study of 0.5 million Chinese adults. BMC Psychiatry 2020, 20, 267. [Google Scholar] [CrossRef]
- Nisarga, V.; Anupama, M.; Madhu, K.N. Social and obstetric risk factors of antenatal depression: A cross-sectional study from South-India. Asian J. Psychiatr. 2022, 72, 103063. [Google Scholar] [CrossRef] [PubMed]
- Zanardo, V.; Manghina, V.; Giliberti, L.; Vettore, M.; Severino, L.; Straface, G. Psychological impact of COVID-19 quarantine measures in northeastern Italy on mothers in the immediate postpartum period. Int. J. Gynaecol. Obstet. 2020, 150, 184–188. [Google Scholar] [CrossRef]
- Pietikäinen, J.T.; Polo-Kantola, P.; Pölkki, P.; Saarenpää-Heikkilä, O.; Paunio, T.; Paavonen, E.J. Sleeping problems during pregnancy-a risk factor for postnatal depressiveness. Arch. Women’s Mental Health volume 2019, 22, 327–337. [Google Scholar] [CrossRef] [PubMed]
- Øygarden, A.U.; Småstuen, M.C.; Abudayya, A.; Glavin, K.; Saether, K.M.; Solberg, B.L.; Brekke, M.; Strøm, B.S. Prevalence and predictive factors of depressive symptoms among primiparae in antenatal care: A cross-sectional study in the new families programme. J. Clin. Nurs. 2023, 32, 4894–4903. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, S.; Hudson, C.C.; Harkness, K. Social Media and Depression Symptoms: A Meta-Analysis. Res. Child Adolesc. Psychopathol. 2021, 49, 241–253. [Google Scholar] [CrossRef] [PubMed]
- Aalbers, G.; McNally, R.J.; Heeren, A.; de Wit, S.; Fried, E.I. Social media and depression symptoms: A network perspective. J. Exp. Psychol. Gen. 2019, 148, 1454–1462. [Google Scholar] [CrossRef]
- Da Silva Tanganhito, D.; Bick, D.; Chang, Y.S. Breastfeeding experiences and perspectives among women with postnatal depression: A qualitative evidence synthesis. Women Birth 2020, 33, 231–239. [Google Scholar] [CrossRef]
- Pope, C.J.; Mazmanian, D. Breastfeeding and Postpartum Depression: An Overview and Methodological Recommendations for Future Research. Depress. Res. Treat. 2016, 2016, 4765310. [Google Scholar] [CrossRef]
- Roberts, T.A.; Hansen, S. Association of Hormonal Contraception with depression in the postpartum period. Contraception 2017, 96, 446–452. [Google Scholar] [CrossRef] [PubMed]
- Ti, A.; Curtis, K.M. Postpartum hormonal contraception use and incidence of postpartum depression: A systematic review. Eur. J. Contracept. Reprod. Health Care 2019, 24, 109–116. [Google Scholar] [CrossRef]
- Mbianda, J.; Mathew, B.; Levine, J.; Amico, J. Is progestin-only contraception associated with higher incidence of postpartum depression? Evid.-Based Pract. 2022, 25, 31–32. [Google Scholar] [CrossRef]
- Woolhouse, H.; Gartland, D.; Perlen, S.; Donath, S.; Brown, S.J. Physical health after childbirth and maternal depression in the first 12 months post partum: Results of an Australian nulliparous pregnancy cohort study. Midwifery 2014, 30, 378–384. [Google Scholar] [CrossRef]
- Austin, M.P.; Tully, L.; Parker, G. Examining the relationship between antenatal anxiety and postnatal depression. J. Affect. Disord. 2007, 101, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Brooks, J.; Nathan, E.; Speelman, C.; Swalm, D.; Jacques, A.; Doherty, D. Tailoring screening protocols for perinatal depression: Prevalence of high risk across obstetric services in Western Australia. Arch. Women’s Ment. Health 2009, 12, 105–112. [Google Scholar] [CrossRef]
- Willinck, L.A.; Cotton, S.M. Risk factors for postnatal depression. Aust. Midwifery 2004, 17, 10–15. [Google Scholar] [CrossRef]
- Aydin, N.; Inandi, T.; Karabulut, N. Depression and Associated Factors Among Women Within Their First Postnatal Year in Erzurum Province in Eastern Turkey. Women Health 2005, 41, 1–12. [Google Scholar] [CrossRef]
- Doering Runquist, J.J.; Morin, K.; Stetzer, F.C. Severe Fatigue and Depressive Symptoms in Lower-Income Urban Postpartum Women. West. J. Nurs. Res. 2009, 31, 599–612. [Google Scholar] [CrossRef]
- Rich-Edwards, J.W.; James-Todd, T.; Mohllajee, A.; Kleinman, K.; Burke, A.; Gillman, M.W.; Wright, R.J. Lifetime maternal experiences of abuse and risk of pre-natal depression in two demographically distinct populations in Boston. Int. J. Epidemiol. 2010, 40, 375–384. [Google Scholar] [CrossRef]
- Sørbø, M.F.; Grimstad, H.; Bjørngaard, J.H.; Lukasse, M.; Schei, B. Adult physical, sexual, and emotional abuse and postpartum depression, a population based, prospective study of 53,065 women in the Norwegian Mother and Child Cohort Study. BMC Pregnancy Childbirth 2014, 14, 316. [Google Scholar] [CrossRef] [PubMed]
 indicates the points of time when the Edinburgh Postpartum Depression Scale (EPDS) is used for screening depressive symptoms.
indicates the points of time when the Edinburgh Postpartum Depression Scale (EPDS) is used for screening depressive symptoms.
 indicates the points of time when the Edinburgh Postpartum Depression Scale (EPDS) is used for screening depressive symptoms.
indicates the points of time when the Edinburgh Postpartum Depression Scale (EPDS) is used for screening depressive symptoms. 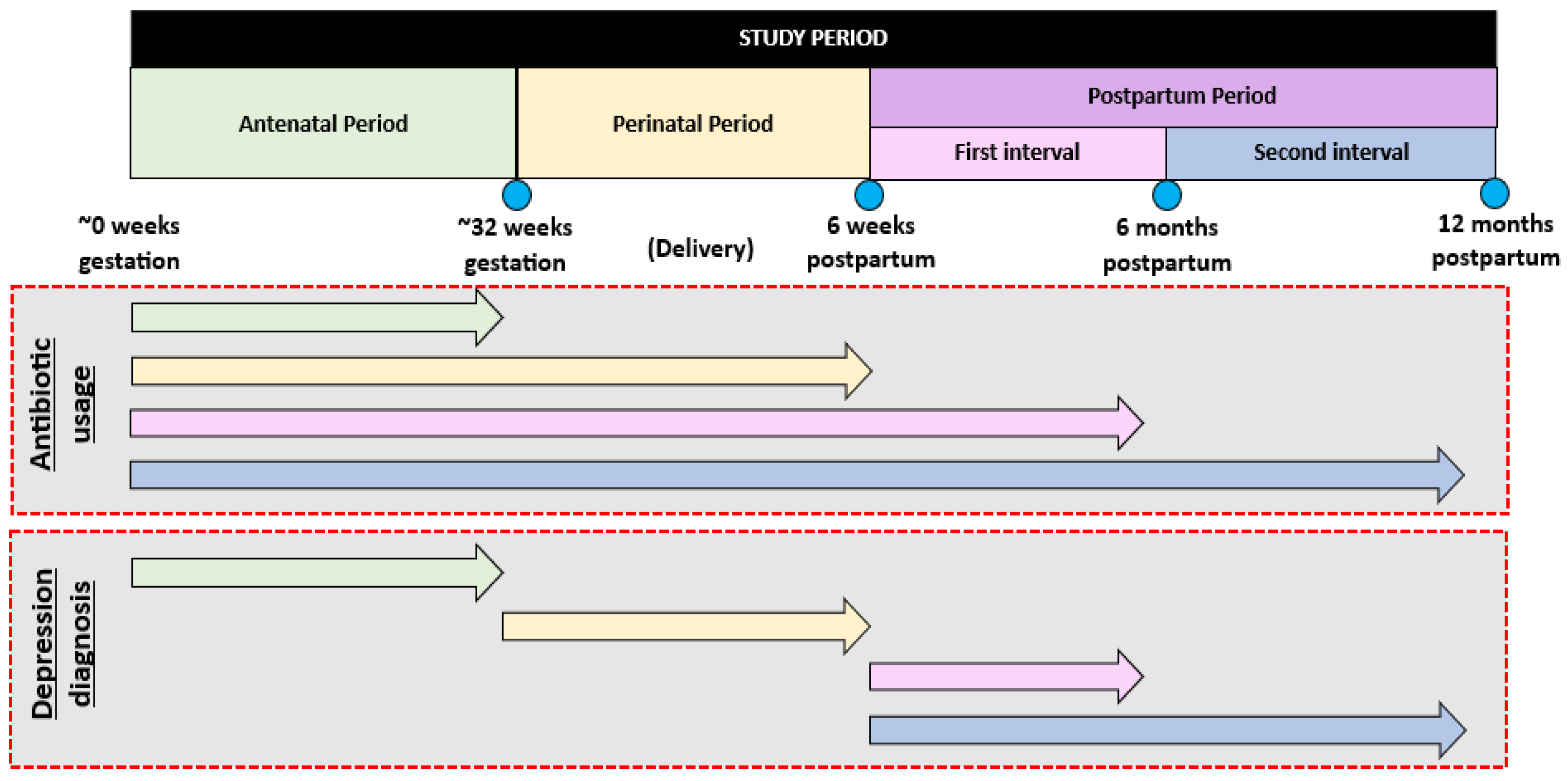
| Variable | Proposed Tool | Description of Tool | Pregnancy | Postpartum Period | ||
|---|---|---|---|---|---|---|
| Initial Survey | 6-Week Survey | 6-Month Survey | 12-Month Survey | |||
| Demographics and Socioeconomic (incl. participant +/− partner work) status | MPUQ | The Maternal Health Study conducted by Murdoch Children’s Research Institute [19]. | ✔ | ✔ | ✔ | ✔ |
| Current medical history and medication use *, including antibiotic and probiotic use | IDQ | N/A | ✔ | ✔ | ✔ | ✔ |
| Impact of COVID-19 pandemic on pregnancy experience | MPUQ | Modified questions from a study by Durankuş and Aksu [20]. | ✔ | ✔ | ✔ | ✔ |
| Antenatal class attendance | IDQ | N/A | ✔ | ✔ | – | – |
| Physical activity | IDQ | N/A | ✔ | ✔ | ✔ | ✔ |
| Social media usage (non-work related) | IDQ | N/A | ✔ | ✔ | ✔ | ✔ |
| Pregnancy and fertility history | MPUQ | The Maternal Health Study conducted by Murdoch Children’s Research Institute [19]. | ✔ | – | – | – |
| Pregnancy expectations and experience | MPUQ and IDQ | The Maternal Health Study conducted by Murdoch Children’s Research Institute [19]. | ✔ | – | – | – |
| Delivery intention, expectation, and actual experience | MPUQ and IDQ | The Maternal Health Study conducted by Murdoch Children’s Research Institute [19]. | ✔ | ✔ | – | – |
| Complications related to pregnancy/delivery | MPUQ | The Maternal Health Study conducted by Murdoch Children’s Research Institute [19]. | ✔ | ✔ | – | – |
| Prior infant feeding experience | MPUQ and IDQ | The Maternal Health Study conducted by Murdoch Children’s Research Institute [19]. | ✔ | – | – | – |
| Intended and actual infant feeding method(s) | MPUQ and IDQ | The Maternal Health Study conducted by Murdoch Children’s Research Institute [19]. | ✔ | ✔ | ✔ | ✔ |
| Previous contraception use intended postpartum contraception use, and factors affecting use (e.g., personal +/− partner religion/cultural beliefs) | IDQ | N/A | ✔ | – | – | – |
| Actual postpartum contraception use | IDQ | N/A | – | ✔ | ✔ | ✔ |
| Pregnancy within 12 months of index pregnancy | IDQ | N/A | – | – | ✔ | ✔ |
| Knowledge about the postpartum period | IDQ | N/A | ✔ | – | – | ✔ |
| Stressful life events | MPUQ | Modified questions from The Social Readjustment Rating Scale [21]. | – | – | – | ✔ |
| Prior and current substance use (incl. alcohol, smoking, and recreational drugs) | AUDIT-C, MPUQ and IDQ | AUDIT-C: Suggested by Australian Guide for the diagnosis of Fetal Alcohol Spectrum Disorder [22]. Provides a standardized method for the assessment of maternal alcohol use. Allows categorisation of the level of fatal risk associated with maternal drinking by derivation of the AUDIT-C score. The Maternal Health Study conducted by Murdoch Children’s Research Institute [19]. | ✔ | – | – | ✔ † |
| Mother-infant bonding | BPQ | Consists of a 25-item questionnaire [23]. Designed to detect disorders of the mother-infant relationship. | – | ✔ | ✔ | ✔ |
| Current intimate partner abuse | CAS-Short | Consists of 18 items for assessing emotional or physical abuse by a partner or ex-partner [24]. Explores history of abuse within the last 12 months. Developed and validated for use in general practices in Australia [24]. Used in previous studies conducted in Australia exploring factors affecting risk of developing depressive symptoms [16,25]. | ✔ | – | – | ✔ |
| Sleep quality | SQS | Consists of a single item to measure overall sleep quality over the prior 7 nights [26]. | ✔ | ✔ | ✔ | ✔ |
| Depression | EPDS | Consists of a 10-item questionnaire [27]. Widely used nationally and internationally [16,25,28]. Recommended by RANZCOG for screening for depression during perinatal period [29]. It has been used and validated for assessment of depression during pregnancy [30] and postpartum [27]. | ✔ | ✔ | ✔ | ✔ |
| Depression, anxiety, and life stress | DASS-21 | Consists of a 21-item questionnaire (7 questions for measuring each variable of depression, stress, and life stress) [31,32]. It is validated for use in the general population, but not specifically for assessing depression during pregnancy and postpartum [31,32]. | ✔ | ✔ | ✔ | ✔ |
| Social support | OSSS-3 | Consists of a 3-item questionnaire [33]. Measures level of social support [33]. | ✔ | ✔ | ✔ | ✔ |
| Variables to Be Explored | Reference for Association with Depression in Prior Studies, Where Applicable | Variable Investigated during Mid-Late Third Trimester | Variable Investigated during Postpartum Time Points (6 Weeks, 6 Months, and 12 Months Postpartum) |
|---|---|---|---|
| Maternal age | [34,35,36] | ✔ | ✔ |
| Body Mass Index | [37,38,39] | ✔ | ✔ |
| Marital status | [40,41] | ✔ | |
| Socioeconomic status, maternal leave, partner maternal leave | [35,41,42,43,44,45,46,47,48] | ✔ | ✔ |
| Level of physical activity during pregnancy and postpartum | [49,50] | ✔ | ✔ |
| Smoking status, alcohol consumption, recreational drug use | [35,51,52] | ✔ | ✔ |
| Personal and family medical history (incl. depression, anxiety, other mental illness) | [36,41,43,46,53,54,55,56,57] and NVI | ✔ | ✔ |
| Nausea and vomiting during pregnancy | [58] | ✔ | N/A |
| Pre- and perinatal admission to hospital | [59] | ✔ | N/A |
| Whether the pregnancy was unplanned | [41,48,60,61,62,63,64,65] | ✔ | ✔ |
| Use of reproductive technologies | [57,66] | ✔ | ✔ |
| Gravidity and parity (incl. previous miscarriages/termination of pregnancy) | [48,60,64,65,67,68] | ✔ | ✔ |
| Whether they delivered in a private or public hospital | NVI | N/A | ✔ |
| Peri- and postpartum complications for mother and baby (e.g., painful caesarean section wound) | [54,59,62,69,70] | N/A | ✔ |
| Mode of delivery | [56,71,72,73] | N/A | ✔ |
| If the birth plan/preferences were able to be followed | NVI | N/A | ✔ |
| Length of stay in hospital postpartum | [74,75] | N/A | ✔ |
| Social support level | [43,46,48,60,63] | ✔ | ✔ |
| Medication use (e.g., antibiotic and probiotic, hormonal contraceptive use, antidepressant/anxiolytic use) | [76,77,78,79,80] | ✔ | ✔ |
| Number of other children to care for | [81] | ✔ | ✔ |
| Current partner abuse | [25,43,48,53,62,63,64,82] | ✔ | ✔ |
| Antenatal depression | [41,53] | - | ✔ |
| Symptoms of stress and anxiety | [43,55,56] | ✔ | ✔ |
| Stressful life events | [42,55,62] | - | ✔ |
| COVID-19 stress and psychological impact of pandemic | [20,83] | ✔ | ✔ |
| Sleep quality | [84,85] | ✔ | ✔ |
| Social media use | [86,87] | ✔ | ✔ |
| Feeding plans and outcome | [88,89] | ✔ | ✔ |
| Contraception | [80,90,91,92] | ✔ | ✔ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pouranayatihosseinabad, M.; Taylor, M.; Hawrelak, J.; Peterson, G.M.; Veal, F.; Ling, T.; Williams, M.; Whatley, M.; Ahdieh, K.; Mirkazemi, C. Maternal Antibiotic Exposure and the Risk of Developing Antenatal or Postpartum Depressive Symptoms: The Maternal Experience Study Protocol. Methods Protoc. 2023, 6, 98. https://doi.org/10.3390/mps6050098
Pouranayatihosseinabad M, Taylor M, Hawrelak J, Peterson GM, Veal F, Ling T, Williams M, Whatley M, Ahdieh K, Mirkazemi C. Maternal Antibiotic Exposure and the Risk of Developing Antenatal or Postpartum Depressive Symptoms: The Maternal Experience Study Protocol. Methods and Protocols. 2023; 6(5):98. https://doi.org/10.3390/mps6050098
Chicago/Turabian StylePouranayatihosseinabad, Mahsa, Maggie Taylor, Jason Hawrelak, Gregory M. Peterson, Felicity Veal, Tristan Ling, Mackenzie Williams, Megan Whatley, Kyan Ahdieh, and Corinne Mirkazemi. 2023. "Maternal Antibiotic Exposure and the Risk of Developing Antenatal or Postpartum Depressive Symptoms: The Maternal Experience Study Protocol" Methods and Protocols 6, no. 5: 98. https://doi.org/10.3390/mps6050098






