Determining Reference Ranges for Total T4 in Dried Blood Samples for Newborn Screening
Abstract
:1. Introduction
2. Materials and Methods
2.1. tT4 Stability in Dried Blood Samples
2.2. Determination of tT4 Ranges
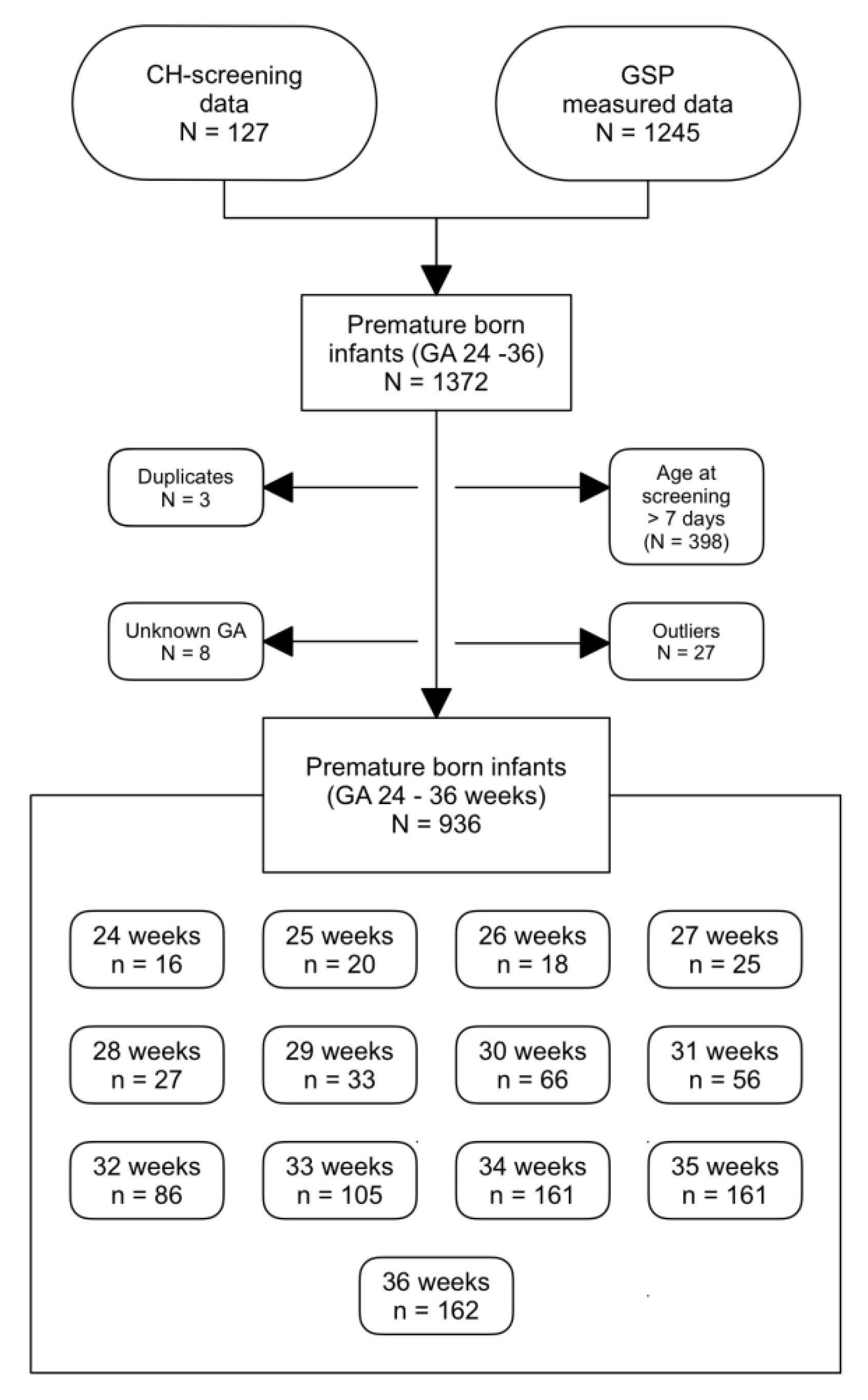
2.2.1. tT4 Values of Preterm-Born Infants
2.2.2. tT4 Concentrations of Term-Born Infants
3. Results
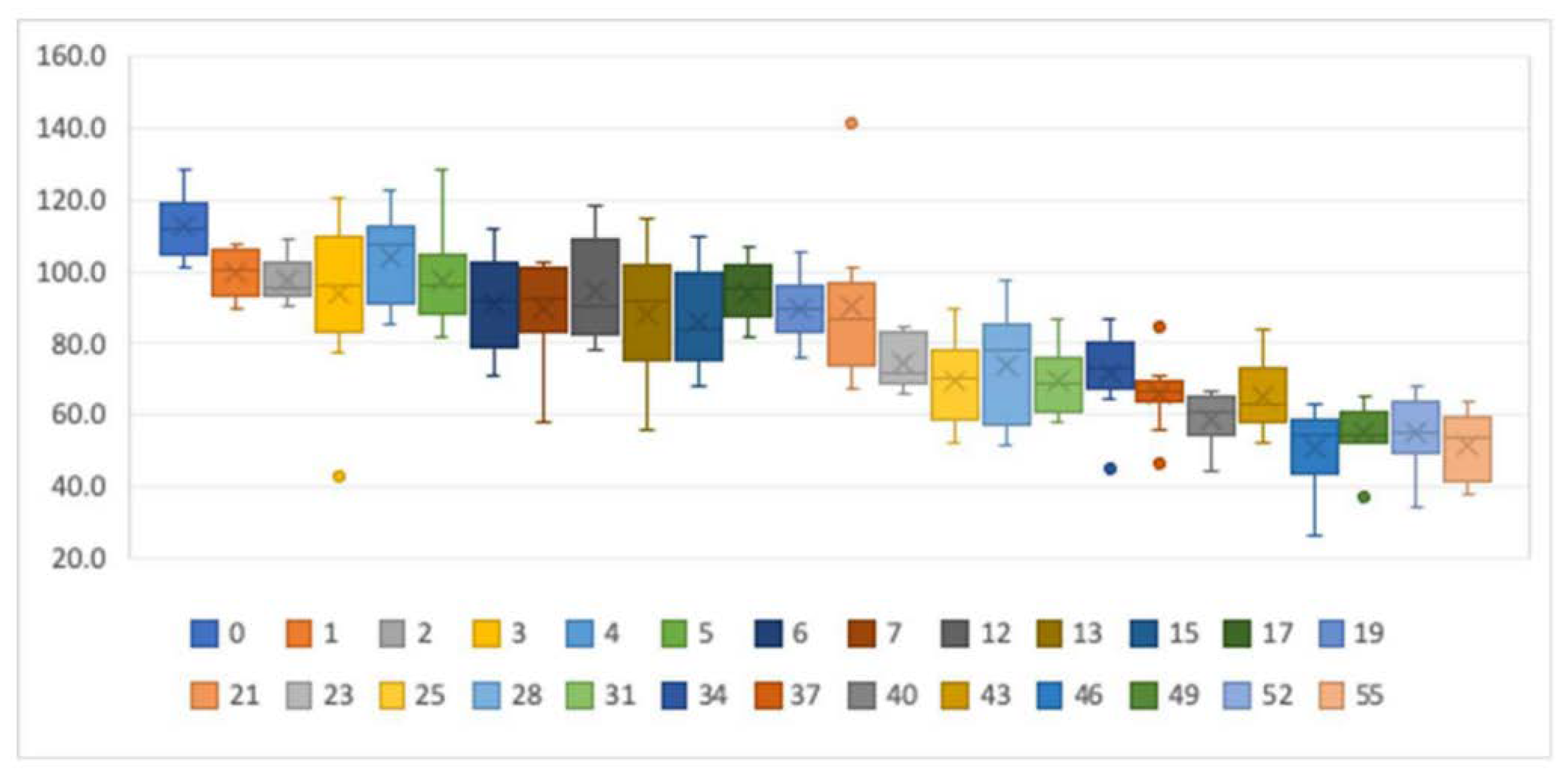
3.1. Stability of tT4 in Dried Blood Samples
3.2. Determination of the tT4 Ranges
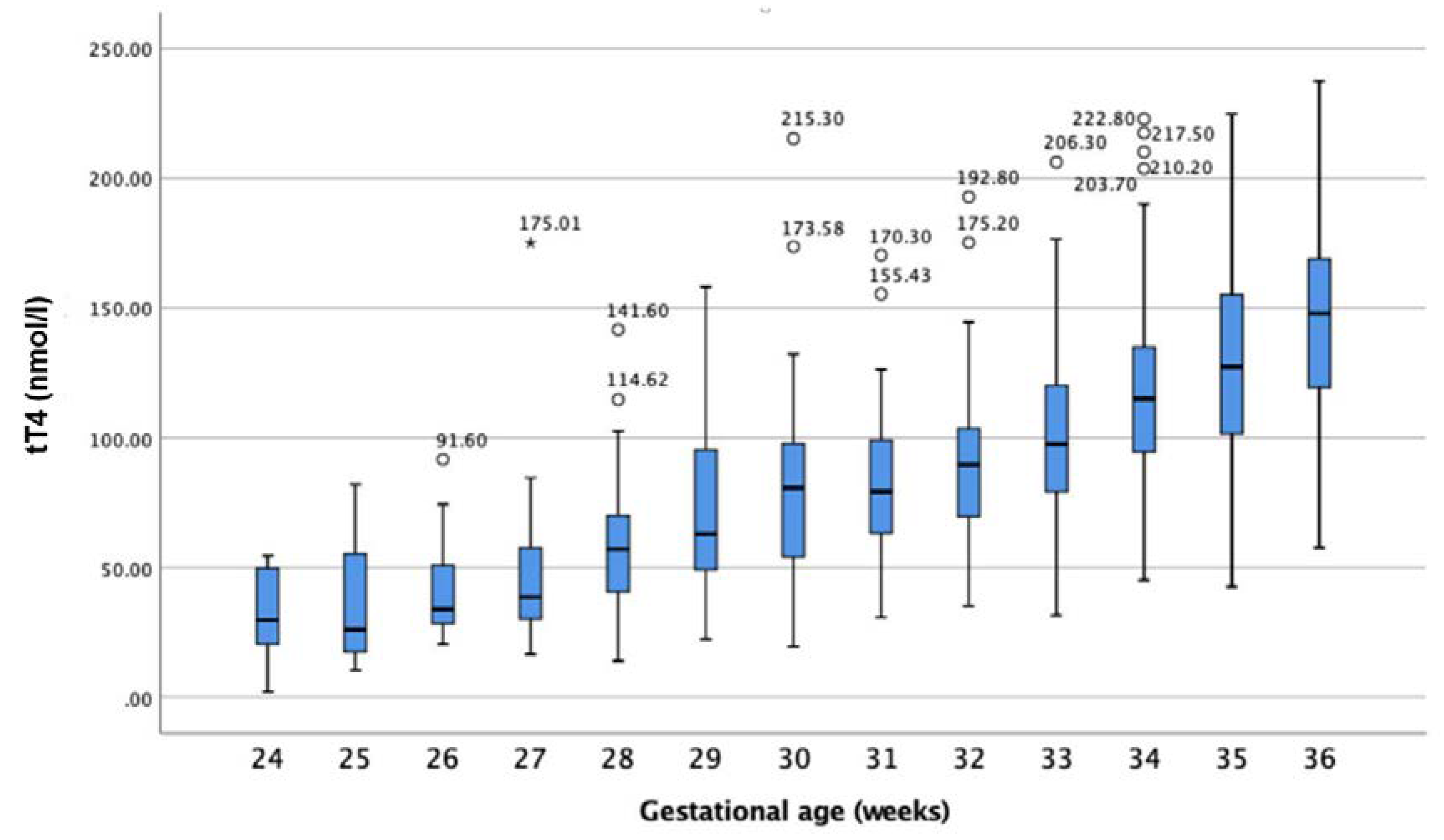
3.2.1. tT4 Values of Preterm-Born Infants
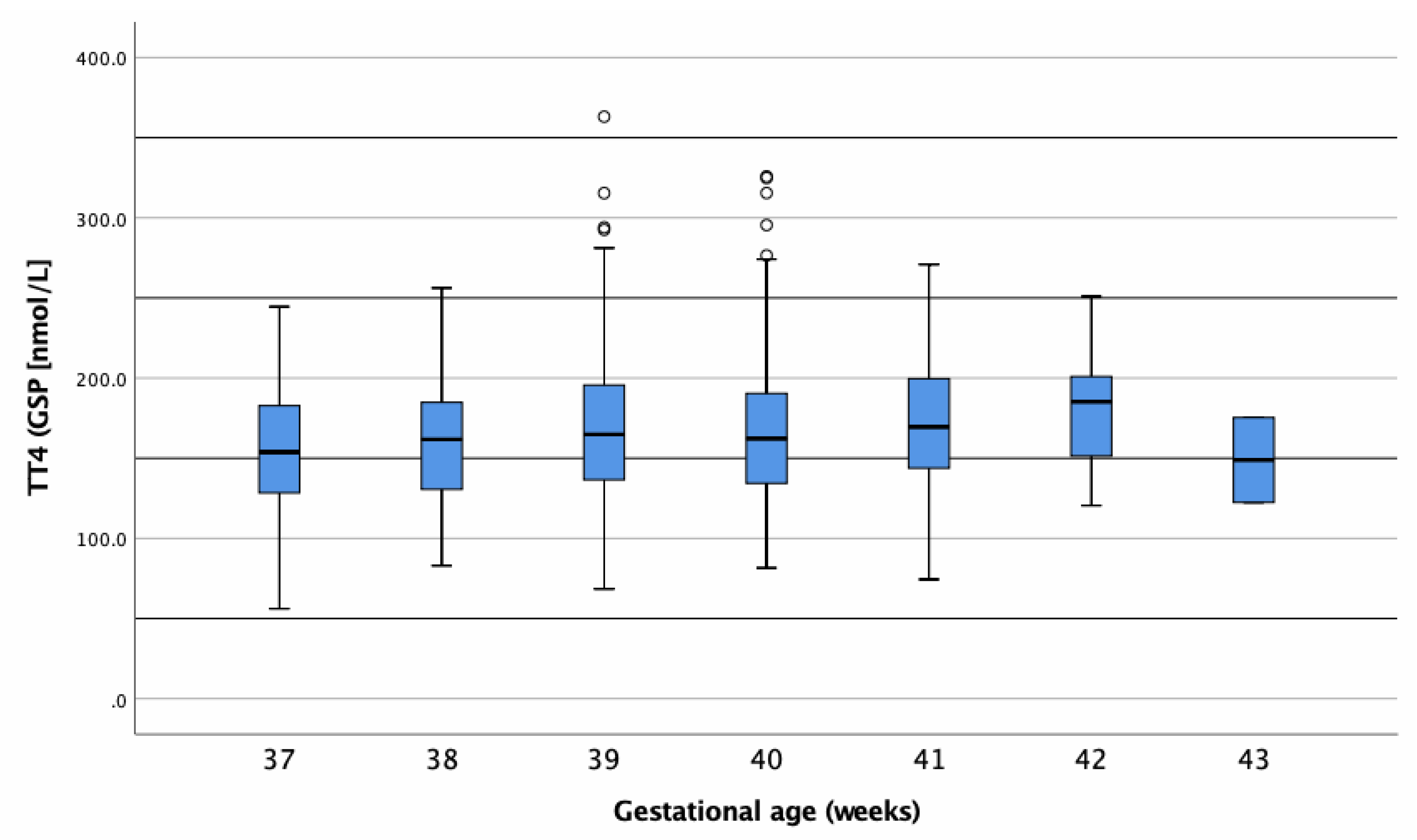
3.2.2. tT4 Concentrations of Term-Born Infants
3.2.3. tT4 Differences between Genders
3.3. Ethics
4. Discussion
4.1. Thyroxine Stability Testing
4.2. Reference Intervals for Newborn and Premature-Born Infants
4.3. Premature-Born Infants (24–36 Weeks)
4.3.1. Reference Individuals
4.3.2. Differences in Thyroid Hormone Regulation Post-Partum between Premature- and Term-Born Infants
4.3.3. Reasons for Hypothyroxinaemia in Premature Infants
4.3.4. Consequences of Hypothyroxinaemia in Premature-Born Infants
4.3.5. Thyroxine Reference Ranges for Premature Infants
4.4. Term-Born Infants (37–43 Weeks)
4.4.1. Reference Ranges for Term-Born Infants
4.4.2. Central Congenital Hypothyroidism
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| DBS | Dried blood sample |
| GA | Gestational age |
| T3 | Triiodothyronine |
| T4 | Thyroxine |
| tT4 | Total thyroxine |
| fT4 | Free thyroxine |
| TSH | Thyroid stimulating hormone |
| THOP | Transitory hypothyroxinaemia of prematurity |
| LBW | Low birthweight |
| VLBW | Very low birthweight |
References
- Shanholtz, H.J. Congenital Hypothyroidism. J. Pediatric. Nurs. 2013, 28, 200–202. [Google Scholar] [CrossRef] [PubMed]
- Ford, G.; Lafranchi, S.H. Screening for congenital hypothyroidism: A worldwide view of strategies. Best Pract. Res. 2014, 28, 175–187. [Google Scholar] [CrossRef] [PubMed]
- Fisher, D.A.; Klein, A.H. Thyroid Development and Disorders of Thyroid Function in the Newborn. N. Engl. J. Med. 1981, 304, 702–712. [Google Scholar] [CrossRef] [PubMed]
- Carrascosa, A.; Ruiz-Cuevas, P.; Potau, N.; Almar, J.; Salcedo, S.; Clemente, M.; Yeste, D. Thyroid Function in Seventy-Five Healthy Preterm Infants Thirty to Thirty-Five Weeks of Gestational Age: A Prospective and Longitudinal Study During the First Year of Life. Thyroid 2004, 14, 435–442. [Google Scholar] [CrossRef] [PubMed]
- McGrath, N.; Hawkes, C.P.; McDonnell, C.M.; Cody, D.; O’Connell, S.M.; Mayne, P.D.; Murphy, N.P. Incidence of Congenital Hypothyroidism Over 37 Years in Ireland. Pediatrics 2018, 142, e20181199. [Google Scholar] [CrossRef] [Green Version]
- Persani, L. Central Hypothyroidism: Pathogenic, Diagnostic, and Therapeutic Challenges. J. Clin. Endocrinol. Metab. 2012, 97, 3068–3078. [Google Scholar] [CrossRef] [Green Version]
- Zwaveling-Soonawala, N.; van Trotsenburg, A.S.P.; Verkerk, P.H. TSH and FT4 Concentrations in Congenital Central Hypothyroidism and Mild Congenital Thyroidal Hypothyroidism. J. Clin. Endocrinol. Metab. 2018, 103, 1342–1348. [Google Scholar] [CrossRef]
- LaFranchi, S.H. Newborn screening strategies for congenital hypothyroidism: An update. J. Inherit. Metab. Dis. 2010, 33, 225–233. [Google Scholar] [CrossRef]
- Available online: https://www.bfs.admin.ch/bfs/de/home/statistiken/gesundheit/gesundheitszustand/gesundheit-neugeborenen.html (accessed on 1 March 2020).
- Lando, V.S.; Batista, M.C.; Nakamura, I.T.; Mazi, C.R.; Mendonca, B.B.; Brito, V.N. Effects of long-term storage of filter paper blood samples on neonatal thyroid stimulating hormone, thyroxin and 17-alpha-hydroxyprogesterone measurements. J. Med. Screen. 2008, 15, 109–111. [Google Scholar] [CrossRef]
- Waite, K.V.; Maberly, G.F.; Eastman, C.J. Storage conditions and stability of thyrotropin and thyroid hormones on filter paper. Clin. Chem. 1987, 33, 853. [Google Scholar] [CrossRef]
- Davis, G.; Poholek, R. Stability of dried blood spots on paper, as used in screening neonates for hypothyroidism. Clin. Chem. 1979, 25, 24–25. [Google Scholar] [CrossRef] [PubMed]
- Adeli, K. Clinical laboratory reference intervals in pediatrics: Current gaps and recent advance. Clin. Biochem. 2011, 44, S7–S8. [Google Scholar] [CrossRef]
- Ishaku, A.A.; Shabbal, D.M.; Isichei, C. Reference Interval of Thyroxine and Thyrotropin of Healthy Term Nigerian Newborns in Jos University of Teaching Hospital. Jos J. Med. 2017, 11, 26–30. [Google Scholar]
- Jacobsen, B.B.; Andersen, H.J.; Peitersen, B.; Dige-Petersen, H.; Hummer, L. Serum Levels of Thyrotropin, Thyroxine and Triiodothyronine in Fullterm, Small-for-gestational Age and Preterm Newborn Babies. Acta Paediatr. 1977, 66, 681–687. [Google Scholar] [CrossRef]
- Larson, C.; Hermos, R.; Delaney, A.; Daley, D.; Mitchell, M. Risk factors associated with delayed thyrotropin elevations in congenital hypothyroidism. J. Pediatr. 2003, 143, 587–591. [Google Scholar] [CrossRef]
- Smith, L. Updated AAP guidelines on newborn screening and therapy for congenital hypothyroidism. Am. Fam. Physician 2007, 76, 439. [Google Scholar] [CrossRef] [Green Version]
- Mandel, S.J.; Hermos, R.J.; Larson, C.A.; Prigozhin, A.B.; Rojas, D.A.; Mitchell, M.L. Atypical Hypothyroidism and the Very Low Birthweight Infant. Thyroid 2000, 10, 693–695. [Google Scholar] [CrossRef]
- Hunter, M.K.; Mandel, S.H.; Sesser, D.E.; Miyabira, R.S.; Rien, L.; Skeels, M.R.; LaFranchi, S.H. Follow-up of newborns with low thyroxine and nonelevated thyroid-stimulating hormone–screening concentrations: Results of the 20-year experience in the Northwest Regional Newborn Screening Program. J. Pediatrics 1998, 132, 70–74. [Google Scholar] [CrossRef]
- Ozarda, Y. Reference intervals: Current status, recent developments and future considerations. Biochem. Med. 2016, 26, 5–16. [Google Scholar] [CrossRef] [Green Version]
- Williams, F.L.R.; Simpson, J.; Delahunty, C.; Ogston, S.A.; Bongers-Schokking, J.J.; Murphy, N.; van Toor, H.; Wu, S.-Y.; Visser, T.J.; Hume, R. Developmental Trends in Cord and Postpartum Serum Thyroid Hormones in Preterm Infants. J. Clin. Endocrinol. Metab. 2004, 89, 5314–5320. [Google Scholar] [CrossRef] [Green Version]
- Chung, H.R.; Shin, C.H.; Yang, S.W.; Choi, C.W.; Kim, B.I.; Kim, E.K.; Kim, H.S.; Choi, J.H. High incidence of thyroid dysfunction in preterm infants. J. Korean. Med. Sci. 2009, 24, 627–631. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Büyükgebiz, A. Newborn screening for congenital hypothyroidism. J. Clin. Res. Pediatr. Endocrinol. 2013, 5, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Reuss, M.L.; Paneth, N.; Pinto-Martin, J.A.; Lorenz, J.M.; Susser, M. The Relation of Transient Hypothyroxinemia in Preterm Infants to Neurologic Development at Two Years of Age. N. Engl. J. Med. 1996, 334, 821–827. [Google Scholar] [CrossRef] [PubMed]
- Meijer, W.J.; Verloove-Vanhorick, S.P.; Brand, R.; van den Brande, J.L. Transient hypothyroxinaemia associated with developmental delay in very preterm infants. Arch. Dis. Child. 1992, 67, 944–947. [Google Scholar] [CrossRef] [PubMed]
- Murphy, N.; Hume, R.; van Toor, H.; Matthews, T.G.; Ogston, S.A.; Wu, S.-Y.; Visser, T.J.; Williams, F.L.R. The Hypothalamic-Pituitary-Thyroid Axis in Preterm Infants; Changes in the First 24 Hours of Postnatal Life. J. Clin. Endocrinol. Metab. 2004, 89, 2824–2831. [Google Scholar] [CrossRef]
- Clark, S.J.; Deming, D.D.; Emery, J.R.; Adams, L.M.; Carlton, E.I.; Nelson, J.C. Reference Ranges for Thyroid Function Tests in Premature Infants Beyond the First Week of Life. J. Perinatol. 2001, 21, 531–536. [Google Scholar] [CrossRef] [Green Version]
- Hollanders, J.J.; Israëls, J.; van der Pal, S.M.; Verkerk, P.H.; Rotteveel, J.; Finken, M.J.J.; Dutch, P.-C.S.G. No Association between Transient Hypothyroxinemia of Prematurity and Neurodevelopmental Outcome in Young Adulthood. J. Clin. Endocrinol. Metab. 2015, 100, 4648–4653. [Google Scholar] [CrossRef] [Green Version]
- La Gamma, E.F.; Korzeniewski, S.J.; Ballabh, P.; Paneth, N. Transient Hypothyroxinemia of Prematurity. NeoReviews 2016, 17, e394–e402. [Google Scholar] [CrossRef]
- Van Wassenaer, A.G.; Kok, J.H.; de Vijlder, J.J.M.; Briët, J.M.; Smit, B.J.; Tamminga, P.; van Baar, A.; Dekker, F.W.; Vulsma, T. Effects of Thyroxine Supplementation on Neurologic Development in Infants Born at Less Than 30 Weeks’ Gestation. N. Engl. J. Med. 1997, 336, 21–26. [Google Scholar] [CrossRef] [Green Version]
- Adams, L.M.; Emery, J.R.; Clark, S.J.; Carlton, E.I.; Nelson, J.C. Reference ranges for newer thyroid function tests in premature infants. J. Pediatr. 1995, 126, 122–127. [Google Scholar] [CrossRef]
- Braslavsky, D.; Méndez, M.V.; Prieto, L.; Keselman, A.; Enacan, R.; Gruñeiro-Papendieck, L.; Jullien, N.; Savenau, A.; Reynaud, R.; Brue, T.; et al. Pilot Neonatal Screening Program for Central Congenital Hypothyroidism: Evidence of Significant Detection. Horm. Res. Paediatr. 2017, 88, 274–280. [Google Scholar] [CrossRef] [PubMed]
- Zwaveling-Soonawala, N.; van Trotsenburg, A.S.P.; Verkerk, P.H. The Severity of Congenital Hypothyroidism of Central Origin Should Not Be Underestimated. J. Clin. Endocrinol. Metab. 2015, 100, E297–E300. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lanting, C.I.; van Tijn, D.A.; Loeber, J.G.; Vulsma, T.; de Vijlder, J.J.M.; Verkerk, P.H. Clinical Effectiveness and Cost-Effectiveness of the Use of the Thyroxine/Thyroxine-Binding Globulin Ratio to Detect Congenital Hypothyroidism of Thyroidal and Central Origin in a Neonatal Screening Program. Pediatrics 2005, 116, 168. [Google Scholar] [CrossRef] [PubMed]

| Storage Time | n | tT4 (nmol/L) | p-Value | |||
|---|---|---|---|---|---|---|
| Baseline | Post Storage | |||||
| Mean | 95% CI | Mean | 95% CI | |||
| 0 weeks | 10 | 116.0 | 88.15–143.98 | 128.6 | 102.2–155.06 | 0.000 |
| 1 week | 10 | 108.4 | 87.25–129.63 | 106.9 | 89.88–123.90 | 0.572 |
| 2 weeks | 10 | 128.1 | 109.35–146.85 | 124.2 | 107.08–141.36 | 0.136 |
| 3 weeks | 10 | 114.4 | 90.52–138.36 | 106.9 | 81.64–132.08 | 0.345 |
| 4 weeks | 10 | 109.5 | 94.31–124.71 | 113.8 | 95.74–131.88 | 0.346 |
| 5 weeks | 9 | 110.6 | 84.02–137.23 | 104.0 | 79.66–128.34 | 0.075 |
| 6 weeks | 10 | 113.8 | 89.94–137.56 | 100.5 | 87.74–113.22 | 0.059 |
| 7 weeks | 11 | 111.2 | 87.47–134.93 | 98.4 | 74.66–122.20 | 0.020 |
| 12 weeks | 10 | 105.1 | 92.24–117.90 | 99.4 | 84.53–114.21 | 0.287 |
| 13 weeks | 10 | 103.4 | 86.76–119.96 | 90.2 | 72.90–107.40 | 0.068 |
| 15 weeks | 10 | 112.0 | 95.03–128.87 | 95.9 | 81.13–110.61 | 0.025 |
| 17 weeks | 10 | 108.9 | 95.30–122.56 | 103.0 | 86.46–119.58 | 0.084 |
| 19 weeks | 9 | 118.4 | 102.01–134.77 | 108.9 | 90.08–127.81 | 0.007 |
| 21 weeks | 9 | 106.5 | 86.17–126.90 | 91.3 | 67.76–114.80 | 0.003 |
| 23 weeks | 10 | 134.4 | 108.22–160.60 | 99.3 | 81.78–116.82 | 0.000 |
| 25 weeks | 11 | 118.1 | 96.31–139.91 | 82.4 | 61.34–103.50 | 0.000 |
| Storage Time | n | tT4 (nmol/L) | p-Value | |||
|---|---|---|---|---|---|---|
| Baseline | Post Storage and Post Correction | |||||
| Mean | 95% CI | Mean | 95% CI | |||
| 6 weeks | 10 | 113.8 | 89.94–137.56 | 110.53 | 96.51–124.54 | 0.594 |
| 7 weeks | 11 | 111.2 | 87.47–134.93 | 108.27 | 82.12–134.41 | 0.570 |
| 12 weeks | 10 | 105.1 | 92.24–117.90 | 109.31 | 92.98–125.63 | 0.455 |
| 13 weeks | 10 | 103.4 | 86.76–119.96 | 99.16 | 80.18–118.14 | 0.551 |
| 15 weeks | 10 | 112.0 | 95.03–128.87 | 105.46 | 89.25–121.67 | 0.324 |
| 17 weeks | 10 | 108.9 | 95.30–122.56 | 113.32 | 95.11–131.54 | 0.245 |
| 19 weeks | 9 | 118.4 | 102.01–134.77 | 119.84 | 103.49–143.31 | 0.660 |
| 21 weeks | 9 | 106.5 | 86.17–126.90 | 100.41 | 78.91–124.78 | 0.181 |
| 23 weeks | 10 | 134.4 | 108.22–160.60 | 109.23 | 89.96–128.50 | 0.000 |
| 25 weeks | 11 | 118.1 | 96.31–139.91 | 90.66 | 67.47–113.85 | 0.000 |
| GA at Birth (Weeks) | Number Studied (n) | Mean ± SD | Percentiles or (Min–Max) * | Unit | |
|---|---|---|---|---|---|
| 2.5 | 97.5 | ||||
| 24 | 16 | 32.52 ± 17.1 | (1.98–54.45) | nmol/L | |
| 2.5 ± 1.3 | (0.15–4.23) | µg/dL | |||
| 25 | 20 | 39.7 ± 25.8 | (10.50–87.30) | nmol/L | |
| 3.1 ± 2.0 | (0.81–6.78) | µg/dL | |||
| 26 | 18 | 36.7 ± 16.7 | (15.40–74.30 | nmol/L | |
| 2.8 ± 1.3 | (1.19–5.77) | µg/dL | |||
| 27 | 25 | 43.2 ± 17.1 | (16.60–84.48) | nmol/L | |
| 3.3 ± 1.3 | (1.29–6.56) | µg/dL | |||
| 28 | 27 | 57.9 ± 24.8 | (15.40–114.62) | nmol/L | |
| 4.4 ± 1.9 | (1.20–8.90) | µg/dL | |||
| 29 | 33 | 76.6 ± 37.6 | (22.33–158.18) | nmol/L | |
| 5.9 ± 2.9 | (1.73–12.29) | µg/dL | |||
| 30 | 66 | 77.6 ± 32.9 | 11.90 | 161.43 | nmol/L |
| 6.0 ± 2.5 | 0.92 | 12.51 | µg/dL | ||
| 31 | 56 | 82.0 ± 31.3 | 33.52 | 163.98 | nmol/L |
| 6.3 ± 2.4 | 2.60 | 12.71 | µg/dL | ||
| 32 | 86 | 86.1 ± 24.5 | 43.97 | 142.40 | nmol/L |
| 6.6 ± 1.9 | 3.41 | 11.04 | µg/dL | ||
| 33 | 105 | 102.4 ± 32.6 | 44.44 | 172.57 | nmol/L |
| 7.9 ± 2.5 | 3.44 | 13.38 | µg/dL | ||
| 34 | 161 | 115.5 ± 29.2 | 64.12 | 179.63 | nmol/L |
| 8.9 ± 2.5 | 4.97 | 13.92 | µg/dL | ||
| 35 | 161 | 129.9 ± 39.5 | 52.26 | 211.16 | nmol/L |
| 10.0 ± 3.0 | 4.05 | 16.37 | µg/dL | ||
| 36 | 162 | 144.4 ± 36.8 | 72.00 | 215.19 | nmol/L |
| 11.1 ± 2.8 | 5.58 | 16.68 | µg/dL | ||
| GA at Birth (Weeks) | Number Studied (n) | Mean ± SD | Percentiles or (Min–Max) * | Unit | |
|---|---|---|---|---|---|
| 2.5 | 97.5 | ||||
| 37 | 60 | 157.6 ± 39.9 | 81.09 | 232.95 | nmol/L |
| 12.1 ± 3.1 | 6.30 | 18.10 | µg/dL | ||
| 38 | 155 | 162.1 ± 36.5 | 101.94 | 237.86 | nmol/L |
| 12.5 ± 2.8 | 7.92 | 18.48 | µg/dL | ||
| 39 | 223 | 168.5 ± 44.2 | 95.80 | 269.42 | nmol/L |
| 13.0 ± 3.4 | 7.44 | 20.93 | µg/dL | ||
| 40 | 260 | 156.9 ± 44.1 | 95.32 | 266.66 | nmol/L |
| 12.8 ± 3.4 | 7.40 | 20.72 | µg/dL | ||
| 41 | 147 | 170.3 ± 39.3 | 94.94 | 242.85 | nmol/L |
| 13.1 ± 3.0 | 7.37 | 18.87 | µg/dL | ||
| 42 | 21 | 182.7 ± 37.6 | (120.50–250.90) | nmol/L | |
| 14.1 ± 2.9 | (9.36–19.49) | µg/dL | |||
| 43 | 2 | 148.9 ± 37.5 | (122.40–175.40) | nmol/L | |
| 11.5 ± 2.9 | (9.51–13.63) | µg/dL | |||
| All | 868 | 166.4 ± 41.7 | 95.91 | 256.00 | nmol/L |
| 12.8 ± 3.2 | 7.45 | 19.90 | µg/dL | ||
| Gender | Number Studied (n) | Mean | Standard Deviation |
|---|---|---|---|
| Male | 749 | 124.4 | 52.75 |
| Female | 619 | 123.7 | 55.10 |
| Unknown | 19 | 137.8 | 46.7 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hijman, A.-I.; Konrad, D.; Fingerhut, R. Determining Reference Ranges for Total T4 in Dried Blood Samples for Newborn Screening. Int. J. Neonatal Screen. 2020, 6, 17. https://doi.org/10.3390/ijns6010017
Hijman A-I, Konrad D, Fingerhut R. Determining Reference Ranges for Total T4 in Dried Blood Samples for Newborn Screening. International Journal of Neonatal Screening. 2020; 6(1):17. https://doi.org/10.3390/ijns6010017
Chicago/Turabian StyleHijman, Anna-Isabella, Daniel Konrad, and Ralph Fingerhut. 2020. "Determining Reference Ranges for Total T4 in Dried Blood Samples for Newborn Screening" International Journal of Neonatal Screening 6, no. 1: 17. https://doi.org/10.3390/ijns6010017
APA StyleHijman, A.-I., Konrad, D., & Fingerhut, R. (2020). Determining Reference Ranges for Total T4 in Dried Blood Samples for Newborn Screening. International Journal of Neonatal Screening, 6(1), 17. https://doi.org/10.3390/ijns6010017






