Capturing Interactive Occupation and Social Engagement in a Residential Dementia and Mental Health Setting Using Quantitative and Narrative Data
Abstract
:1. Introduction
1.1. Theoretical Framework
1.2. Social Justice and Occupational Justice
2. Method
3. Results
3.1. Demographical Information
3.2. ATOSE Quantitative Observational Data Results
3.3. Qualitative (Narrative) Observational Data Results
3.3.1. Social Environment
3.3.2. Physical Environment
3.3.3. Fixed Routines
3.3.4. Sensory Environment
3.3.5. Interactive and Occupational Environment
4. Discussion
4.1. Staff Training
4.2. Sensory Environments
4.3. Recommendations for Change
4.3.1. Environments Supporting Engagement
4.3.2. Provision of Specialized Staff to Provide Occupational Interaction and Social Engagement
4.3.3. Physical Design
4.3.4. Social Policies
4.3.5. Operational Policies
4.4. Limitations
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Havighurst, R.J. Successful aging. Gerontologist 1961, 1, 8–13. [Google Scholar] [CrossRef]
- Atchley, R. A continuity theory of normal aging. Gerontologist 1989, 2, 183–190. [Google Scholar] [CrossRef]
- Wadensten, B. An analysis of psychosocial theories of ageing and their relevance to practical gerontological nursing in Sweden. Scand. J. Caring Sci. 2006, 20, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Nimrod, G. Expanding, reducing, concentration and diffusing: Post retirement leisure behavior and life satisfaction. Leis Sci. 2007, 29, 91–111. [Google Scholar] [CrossRef]
- Eakman, A.; Carlson, M.; Clark, F. The Meaningful Activity Participation Assessment: A measure of engagement in personally valued activities. Int. J. Aging Hum. Dev. 2010, 70, 299–317. [Google Scholar] [CrossRef] [PubMed]
- Causey-Upton, R. A model for quality of life: Occupational justice and leisure continuity for nursing home residents. Phys. Occup. Ther. Geriatr. 2015, 33, 175–188. [Google Scholar] [CrossRef]
- Townsend, E. Critical occupational literacy: Thinking about occupational justice, ecological sustainability, and aging in everyday life. J. Occup. Sci. 2015, 22, 389–402. [Google Scholar] [CrossRef]
- Nilsson, I.; Townsend, E. Occupational justice—bridging theory and practice. Scan. J. Occup. Ther. 2010, 17, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Jakobsen, K. If work doesn’t work: How to enable occupational justice. J. Occup. Sci. 2004, 11, 125–134. [Google Scholar] [CrossRef]
- Moyle, W.; Fetherstonhaugh, D.; Greben, M.; Beattie, E.; AusQoL Group. Influencers on quality of life as reported by people living with dementia in long-term care: a descriptive exploratory approach. BMC Geriatr. 2015, 15, 50. [Google Scholar] [CrossRef] [PubMed]
- Heggestad, A.; Nortvedt, P.; Slettebo, A. ‘Like a prison without bars’: Dementia and experiences of dignity. Nurs. Ethics. 2013, 20, 881–892. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kane, R.A.; Lum, T.Y.; Cutler, L.J.; Degenholtz, H.B.; Yu, T.-C. Resident outcomes in small-house nursing homes: A longitudinal evaluation of the initial Green House program. J. Am. Geriatr. Soc. 2007, 55, 832–839. [Google Scholar] [CrossRef] [PubMed]
- Chang, S. Lived experiences of nursing home residents in Korea. Asian Nurs. Res. 2013, 7, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Whall, A.; Kolanowski, A. The need-driven dementia-compromised behavior model—a framework for understanding the behavioral symptoms of dementia. Aging Ment. Health 2004, 8, 106–108. [Google Scholar] [CrossRef] [PubMed]
- Cohen-Mansfield, J.; Marx, M.S.; Thein, K.; Dakheel-Ali, M. The impact of past and present preferences on stimulus engagement in nursing home residents with dementia. Aging Ment. Health 2010, 14, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Cohen-Mansfield, J.; Marx, M.S.; Thein, K.; Dakheel-Ali, M. The impact of stimuli on affect in persons with dementia. J. Clin. Psychiatry 2011, 72, 480–486. [Google Scholar] [CrossRef] [PubMed]
- Cohen-Mansfield, J.; Thein, K.; Dakheel-Ali, M.; Regier, N.G.; Marx, M.S. The value of social attributes of stimuli for promoting engagement in persons with dementia. J. Nerv. Ment. Dis. 2010, 198, 586–592. [Google Scholar] [CrossRef] [PubMed]
- Cohen-Mansfield, J.; Dakheel-Ali, M.; Thein, K.; Marx, M. The impact of stimulus attributes on engagement of nursing home residents with dementia. Arch. Gerontol. Geriatr. 2009, 49, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Avorn, J.; Langer, E. Induced disability in nursing home patients: A controlled trial. J. Am. Geriatr. Soc. 1982, 30, 397–400. [Google Scholar] [CrossRef] [PubMed]
- Engelman, K.K.; Mathews, R.M.; Altus, D.E. Restoring dressing independence in persons with Alzheimer’s disease: A pilot study. Am. J. Alzheimer’s Dis. Other Demen. 2002, 17, 37–43. [Google Scholar] [CrossRef]
- Holthe, T.; Thorsen, K.; Josephsson, S. Occupational patterns of people with dementia in residential care: An ethnographic study. Scan. J. Occup. Ther. 2007, 14, 96–107. [Google Scholar] [CrossRef] [PubMed]
- Sprangers, S.; Dijkstra, K.; Romijn-Luijten, A. Communication skills training in a nursing home: Effects of a brief intervention on residents and nursing aides. Clin. Interv. Aging. 2015, 10, 311–319. [Google Scholar] [PubMed]
- Phinney, A.; Chaudhury, H.; O’Connor, D.L. Doing as much as I can do: The meaning of activity for people with dementia. Aging Ment. Health 2007, 11, 384–393. [Google Scholar] [CrossRef] [PubMed]
- Menec, V. The relation between everyday activities and successful aging: A 6-year longitudinal study. J. Gerontol. B Psychol. Sci. Soc. Sci. 2003, 58, S74–S82. [Google Scholar] [CrossRef] [PubMed]
- Dahlan, A.; Ibrahim, S.; Maciver, D.; Nicol, M. The idiographic experience of the Lively Later Life Programme (3LP) for older people in institutional settings in Malaysia. EIJST 2014, 3, 3–24. [Google Scholar]
- Ibrahim, S.; Dahlan, A. Engagement in occupational activities and purpose in life amongst older people in the community and institutions. Procedia Soc. Behav. Sci. 2015, 202, 263–272. [Google Scholar] [CrossRef]
- Russell, S. Human developmental science for social justice. Res. Hum. Dev. 2015, 12, 274–279. [Google Scholar] [CrossRef]
- Townsend, E.; Wilcock, A. Occupational justice and client-centred practice: A dialogue in progress. Can. J. Occup. Ther. 2004, 71, 75–87. [Google Scholar] [CrossRef] [PubMed]
- Townsend, E.; Marval, R. Can professionals actually enable occupational justice? Cad. Ter. Ocup. 2013, 21, 215–228. [Google Scholar] [CrossRef]
- Richards, K.; D’Cruz, R.; Harman, S.; Stagnitti, K. Comparison of a traditional and non-traditional residential care facility for persons living with dementia and the impact of the environment on occupational engagement. Aust. Occup. Ther. J. 2015, 62, 438–448. [Google Scholar] [CrossRef] [PubMed]
- Morgan-Brown, M. Changes in Interactive Occupation and Social Engagement for People with Dementia: Comparing Household to Traditional Nursing Home Environments in Ireland. Ph.D. Thesis, University of Salford, Manchester, UK, 1 January 2013. Available online: http://usir.salford.ac.uk/id/eprint/30253 (accessed on 27 June 2016). [Google Scholar]
- Hutchinson, A.; Milke, D.; Maisey, S.; Johnson, C.; Squires, J.; Teare, B.; Estabrooks, C. The Resident Assessment Instrument-Minimum Dataset 2.0 quality indicators: A systematic review. BMC Health Serv. Res. 2010, 10, 166. [Google Scholar] [CrossRef] [PubMed]
- Wood, W.; Harris, S.; Snider, M.; Patchel, S.A. Activity situations on an Alzheimer’s disease special care unit and resident environmental interactions, time use, and affect. Am. J. Alzheimers Dis. Other Demen. 2005, 20, 105–117. [Google Scholar] [CrossRef] [PubMed]
- Brooker, D.; Surr, C. Dementia Care Mapping (DCM): Initial validation of DCM 8 in UK field trials. Int. J. Geriatr. Psychiatry 2006, 21, 1018–1025. [Google Scholar] [CrossRef] [PubMed]
- Van Haitsma, K.; Lawton, M.; Kleban, M.K.J.; Corn, J. Methodological aspects of the study of streams of behavior in elders with dementing illness. Alzheimer Dis. Assoc. Disord. 1997, 11, 228–238. [Google Scholar]
- Robson, C. Real World Research: A Resource for Social Scientists and Practitioner-Researchers, 2nd ed.; Blackwell Publishers Ltd.: Oxford, UK, 2002. [Google Scholar]
- Cantley, C.; Woodhouse, J.; Smith, M. Listen to Us: Involving People with Dementia in Planning and Developing Services; Dementia North, Northumbria University: Newcastle, NE, USA, 2005. [Google Scholar]
- Dewing, J. From ritual to relationship: A person-centred approach to consent in qualitative research with older people who have dementia. Dementia 2002, 1, 157–171. [Google Scholar] [CrossRef]
- Sandelowski, M. Telling stories: Narrative approaches in qualitative research. J. Nurs. Scholarsh. 1991, 23, 161–166. [Google Scholar] [CrossRef]
- Morgan-Brown, M.; Newton, R.; Ormerod, M. Engaging life in two Irish nursing home units for people with dementia: Quantitative comparisons before and after implementing household environments. Aging Ment. Health 2013, 17, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Morgan-Brown, M.; Ormerod, M.; Newton, R.; Manley, D. An exploration of occupation in nursing home residents with dementia. Br. J. Occup. Ther. 2011, 74, 217–225. [Google Scholar] [CrossRef]
- Gustafsdottir, M. Is watching television a realistic leisure option for people with dementia? Dement. Geriatr. Cogn. Disord. 2015, 5, 116–122. [Google Scholar] [CrossRef] [PubMed]
- Settersten, R. Relationships in time and the life course: the significance of linked lives. Res. Hum. Dev. 2015, 12, 217–223. [Google Scholar] [CrossRef]
- Kolanowski, A.; Litaker, M.; Buettner, L.; Moeller, J.; Costa, P. A randomized clinical trial of theory-based activities for the behavioral symptoms of dementia in nursing home residents. J. Am. Geriatr. Soc. 2011, 59, 1032–1041. [Google Scholar] [CrossRef] [PubMed]
- Schreiner, A.; Yamamoto, E.; Shiotani, H. Positive affect among nursing home residents with Alzheimer’s dementia: The effect of recreational activity. Aging Ment. Health 2005, 9, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Kong, E.; Evans, L.; Guevara, J. Nonpharmacological intervention for agitation in dementia: A systematic review and meta-analysis. Aging Ment. Health 2009, 13, 512–520. [Google Scholar] [CrossRef] [PubMed]
- Cohen-Mansfield, J.; Marx, M.S.; Dakheel-Ali, M.; Regier, N.G.; Thein, K.; Freedman, L. Can agitated behavior of nursing home residents with dementia be prevented with the use of standardized stimuli? J. Am. Geriatr. Soc. 2010, 58, 1459–1464. [Google Scholar] [CrossRef] [PubMed]
- Telenius, E.; Engedal, K.; Bergland, A. Long-term effects of a 12 weeks high-intensity functional exercise program on physical function and mental health in nursing home residents with dementia: a single blinded randomized controlled trial. BMC Geriatr. 2015, 15, 158. [Google Scholar] [CrossRef] [PubMed]
- Telenius, E.; Engedal, K.; Bergland, A. Physical performance and quality of life of nursing-home residents with mild and moderate dementia. Int. J. Environ. Res. Publ. Health 2013, 10, 6672–6686. [Google Scholar] [CrossRef] [PubMed]
- Richards, K.; Beck, C.; O’Sullivan, P.; Shue, V. Effect of individualized social activity on sleep in nursing home residents with dementia. J. Am. Geriatr. Soc. 2005, 53, 1510–1517. [Google Scholar] [CrossRef] [PubMed]
- Filan, S.; Llewellyn-Jones, R. Animal-assisted therapy for dementia: A review of the literature. Int. Psychogeriatr. 2006, 18, 597–611. [Google Scholar] [CrossRef] [PubMed]
- Garre-Olmo, J.; Lopez-Pousa, S.; Turon-Estrada, A.; Juvinya, D.; Ballester, D.; Vilalta-Franch, J. Environmental determinants of quality of life in nursing home residents with severe dementia. J. Am. Geriatr. Soc. 2012, 60, 1230–1236. [Google Scholar] [CrossRef] [PubMed]
- Anderiesen, H.; Scherder, E.; Goossens, R.; Sonneveld, M. A systematic review—physical activity in dementia: The influence of the nursing home environment. Appl. Ergon. 2014, 45, 1678–1686. [Google Scholar] [CrossRef] [PubMed]
- Wood, W.; Womack, J.; Hooper, B. Dying of boredom: An exploratory case study of time use, apparent affect, and routine activity situations on two Alzheimer’s Special Care Units. Am. J. Occup. Ther. 2009, 63, 337–350. [Google Scholar] [CrossRef] [PubMed]
- Brooker, D. What makes life worth living? Aging Ment. Health 2008, 12, 525–527. [Google Scholar] [CrossRef] [PubMed]
- Mozley, D. Exploring connections between occupation and mental health in care homes for older people. J. Occup. Sci. 2001, 8, 14–19. [Google Scholar] [CrossRef]
- Kiely, D.; Flacker, J. The protective effect of social engagement on 1-year mortality in a long-stay nursing home population. J. Clin. Epidemiol. 2003, 56, 472–478. [Google Scholar] [CrossRef]
- Danes, S. Creating an environment for community. Alzheimer’s Care Q. 2002, 3, 61–66. [Google Scholar]
- Fritsch, T.; Kwak, J.; Grant, S.; Lang, J.; Montgomery, R.; Basting, A. Impact of TimeSlips, a creative expression intervention program, on nursing home residents with dementia and their caregivers. Gerontologist 2009, 49, 117–127. [Google Scholar] [CrossRef] [PubMed]
- Friedmann, E.; Galik, E.; Thomas, S.; Hall, P.; Chung, S.; McCune, S. Evaluation of a pet-assisted living intervention for improving functional status in assisted living residents with mild to moderate cognitive impairment: A pilot study. Alzheimer Dis. Assoc. Disord. 2015, 30, 276–289. [Google Scholar] [CrossRef] [PubMed]
- Rahman, A.; Schnelle, J. The nursing home culture-change movement: Recent past, present and future directions for research. Gerontologist 2008, 48, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Smit, D.; de Lange, J.; Willemse, B.; Pot, A. The relationship between small-scale care and activity involvement of residents with dementia. Int. Psychogeriatr. 2012, 24, 722–732. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- du Toit, S.; van der Merwe, R. Promoting person-centred care for people with advanced dementia through environmental adaptations. S. Afr. J. Occup. Ther. 2012, 43, 2–4. [Google Scholar]
- Pulsford, D. Therapeutic activities for people with dementia—what, why .... and why not? J. Adv. Nurs. 1997, 26, 704–709. [Google Scholar] [CrossRef] [PubMed]
- Morgan-Brown, M.; Ormerod, M.; Newton, R.; Manley, D.; Fitzpatrick, M. Social and occupational engagement of staff in two Irish nursing homes for people with dementia. Ir. J. Occup. Ther. 2011, 39, 11–17. [Google Scholar]
- Kim, H. Effects of experience-based group therapy on cognitive and physical functions and psychological symptoms of elderly people with mild dementia. J. Phys. Ther. Sci. 2015, 27, 2069–2071. [Google Scholar] [CrossRef] [PubMed]
- Werezak, L.J.; Morgan, D.G. Creating a therapeutic psychosocial environment in dementia care. J. Gerontolog. Nurs. 2003, 29, 18–25. [Google Scholar] [CrossRef]
- Bradshaw, S.; Playford, E.; Riazi, A. Living well in care homes: A systematic review of qualitative studies. Age Ageing 2012, 41, 429–440. [Google Scholar] [CrossRef] [PubMed]
- Pulsford, D.; Rushforth, D.; Connor, I. Woodlands therapy: An ethnographic analysis of a small-group therapeutic activity for people with moderate or severe dementia. J. Adv. Nurs. 2000, 32, 650–657. [Google Scholar] [CrossRef] [PubMed]
- De Boer, B.; Hamers, J.; Beerens, H.; Zwakhalen, S.; Tan, F.; Verbeek, H. Living at the farm, innovative nursing home care for people with dementia - study protocol of an observational longitudinal study. BMC Geriatr. 2015, 15, 144. [Google Scholar] [CrossRef] [PubMed]
- De Bruin, S.; Stoop, A.; Molema, C.; Vaandrager, L.; Hop, P.; Baan, C. Green care farms: An innovative type of adult day service to stimulate social participation of people with dementia. Gerontol. Geriatr. Med. 2015, 1. [Google Scholar] [CrossRef]
- Whear, R.; Coon, J.; Bethel, A.; Abbott, R.; Stein, K.; Garside, R. What is the impact of using outdoor spaces such as gardens on the physical and mental well-being of those with dementia? A systematic review of quantitative and qualitative evidence. J. Am. Med. Dir. Assoc. 2014, 15, 697–705. [Google Scholar] [CrossRef] [PubMed]
- Altus, D.; Engelman, K.; Mathews, R. Finding a practical method to increase engagement of residents on a dementia care unit. Am. J. Alzheimers Dis. Other Demen. 2002, 17, 245–248. [Google Scholar] [CrossRef] [PubMed]
- Burgio, L.; Allen-Burge, R.; Roth, D.; Bourgeois, M.; Dijkstra, K.; Gerstle, J.; Jackson, E.; Bankester, L. Come talk with me: Improving communication between nursing assistants and nursing home residents during care routines. Gerontologist 2000, 41, 449–460. [Google Scholar] [CrossRef]
- Telenius, E.; Engedal, K.; Bergland, A. Physical performance and quality of life of nursing-home residents with mild and moderate dementia. Int. J. Environ. Res. Publ. Health 2013, 10, 6672–6686. [Google Scholar] [CrossRef] [PubMed]
- Yoon, J.; Lee, S.; Lim, H.; Kim, T.; Jeon, J.; Mun, M. The effects of cognitive activity combined with active extremity exercise on balance, walking activity, memory level and quality of life of an older adult sample with dementia. J. Physical. Therap. Sci. 2013, 25, 1601–1604. [Google Scholar] [CrossRef] [PubMed]
- Morgan-Brown, M.; Chard, G. Comparing communal environments using the Assessment Tool for Occupation and Social Engagement: Using interactive occupation and social engagement as outcome measures. Br. J. Occup. Ther. 2014, 77, 50–58. [Google Scholar] [CrossRef]
- Bone, C.; Cheung, G.; Wade, B. Evaluating person centred care and Dementia Care Mapping in a psychogeriatric hospital in New Zealand: A pilot study. N. Z. J. Occup. Ther. 2010, 57, 35–40. [Google Scholar]
| Age | n | Diagnosis | n | Communication Ability | n | ADL Dependency | n |
|---|---|---|---|---|---|---|---|
| 60–70 | 7 | Dementia | 4 | Able to initiate conversation | 9 | Eating | 4 |
| 70–80 | 8 | Bipolar | 4 | Will respond but not initiate | 6 | Dressing | 15 |
| 80–90 | 3 | Psychosis | 7 | Greatly reduced conversation | 1 | Hygiene | 19 |
| 90+ | 2 | Depression; anxiety | 2 | No real conversation | 4 | Toileting | 5 |
| Intellectual disability | 3 |
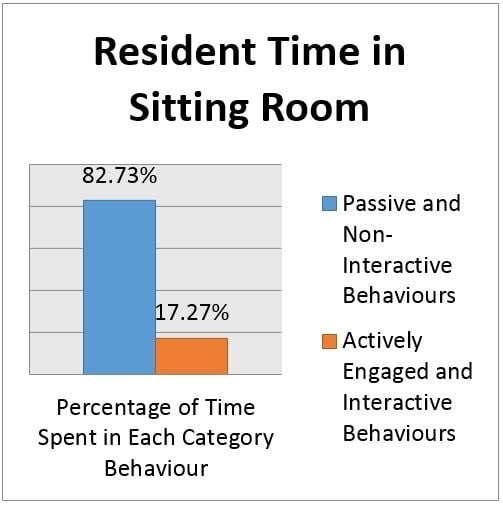
| Resident: Engagement and Interaction Levels | Examples of Behaviours | % age time spent |
|---|---|---|
| Social Engagement | Talking with another, non-verbal interaction (e.g., patting another on the hands) | 3.72 |
| Interactive Occupation | Active reading, participation in individual or group activity, walking, drinking, eating | 10.70 |
| Receiving Care | Medication, adjusting clothes, re-positioning | 2.85 |
| Subtotal: Engagement and Interactive Occupation | 17.27 | |
| No Interaction | Calm sitting, staring into space, disassociated from the environment | 36.61 |
| Eyes Closed | Dozing, sleeping, disconnected from the environment with closed eyes | 40.25 |
| Agitated | Forceful rocking, distressed verbal noises | 0.5 |
| Self-Stimulatory | Repetitive scratching, repetitive touching | 5.37 |
| Subtotal: Non-engaged and non-Interactive | 82.73 | |
| Total of all Categories | 100 % |
| Staff: Engagement and Interaction Levels | Examples of Behaviours | % age time spent |
|---|---|---|
| Social Engagement | Talking with other staff, residents, visitors | 22.04 |
| Interactive Occupation | Undertaking activity with residents such as games, crafts, magazine reading | 8.79 |
| Providing Care | Adjusting clothes, transfers, escorting to toilet | 15.78 |
| Subtotal: Interpersonal Engagement | 56.61 | |
| No Interaction | No active involvement | 1.16 |
| Catering Tasks | Setting tables, preparing food without involvement of residents | 10.44 |
| Domestic Tasks | Sweeping, cleaning without involvement of residents | 3.48 |
| Professional Tasks | Medication trolley, telephone, hand-over discussions | 28.31 |
| Subtotal: Interpersonal non-Engagement | 43.39 | |
| Total of all Categories | 100 % |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morgan-Brown, M.; Brangan, J. Capturing Interactive Occupation and Social Engagement in a Residential Dementia and Mental Health Setting Using Quantitative and Narrative Data. Geriatrics 2016, 1, 15. https://doi.org/10.3390/geriatrics1030015
Morgan-Brown M, Brangan J. Capturing Interactive Occupation and Social Engagement in a Residential Dementia and Mental Health Setting Using Quantitative and Narrative Data. Geriatrics. 2016; 1(3):15. https://doi.org/10.3390/geriatrics1030015
Chicago/Turabian StyleMorgan-Brown, Mark, and Joan Brangan. 2016. "Capturing Interactive Occupation and Social Engagement in a Residential Dementia and Mental Health Setting Using Quantitative and Narrative Data" Geriatrics 1, no. 3: 15. https://doi.org/10.3390/geriatrics1030015