The Application of Porous Scaffolds for Cardiovascular Tissues
Abstract
:1. Introduction
2. Porous Scaffolds
3. Methods to Create Porous Scaffolds
4. Materials for Porous Scaffolds
4.1. Synthetic Polymer
4.2. Natural Polymer
4.3. Silk, Fibroin, Chitosan
4.4. Composite Material
5. Tissue-Engineered Vascular Graft
5.1. Tissue-Engineered Arterial Graft (TEAG)
5.2. Tissue-Engineered Venous Graft (TEVeG)
6. Tissue-Engineered Heart Valve (TEHV)
7. Cardiac Patch
| Material | Animal Species | Number | Surgery or Intervention | Findings | Reference |
|---|---|---|---|---|---|
| PGA/PLCL with hiPS-CMs | Rat | 6 | RVOT reconstruction, with the cardiomyocyte seeded scaffold. | Seeded cells were not present in the patch after 4 weeks. The seeded cell might affect the host cardiac regeneration at 16 weeks. | [119] |
| PGA/PLCL with hiPS-CPCs | Rat | 3 | LV free wall reconstruction with CPC seeded scaffold. | Seeded cells disappeared at an early stage, no contribution to LV function, possibility of affecting angiogenesis at 9 months. | [120] |
| collagen+G-CSF | Rat AMI model | 5 for each group | engrafting the collagen patch onto the injured myocardium | Effectively grafted, further increase in neovascularization with G-CSF | [122] |
| collagen with BMC+VEGF | Rat | 3-4/group | RV free wall reconstruction with collagen patch. | Promoted cell proliferation within the graft, increased blood vessel density and reduced construct thinning. | [123] |
| Chitosan-hyaluronan/slik fibroin | Rat AMI model | 11 | epicardial placement on the injured area | Improved LV function, reduced LV dilation, also improved angiogenesis. | [124] |
8. Future Prospective
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Truby, L.K.; Rogers, J.G. Advanced heart failure: Epidemiology, diagnosis, and therapeutic approaches. JACC Heart Fail. 2020, 8, 523–536. [Google Scholar] [CrossRef]
- Spears, J.; Al-Saiegh, Y.; Goldberg, D.; Manthey, S.; Goldberg, S. TAVR: A review of current practices and considerations in low-risk patients. J. Interv. Cardiol. 2020, 2020, 2582938. [Google Scholar] [CrossRef]
- Mack, M.; Carroll, J.D.; Thourani, V.; Vemulapalli, S.; Squiers, J.; Manandhar, P.; Deeb, G.M.; Batchelor, W.; Herrmann, H.C.; Cohen, D.J.; et al. Transcatheter Mitral valve therapy in the United States: A report from the STS-ACC TVT Registry. J. Am. Coll. Cardiol. 2021, 78, 2316–2353. [Google Scholar] [CrossRef]
- Head, S.J.; Milojevic, M.; Daeman, J.; Ahn, J.M.; Boersma, E.; Christiansen, E.H.; Domanski, M.J.; Farkouh, M.E.; Flather, M.; Fuster, V.; et al. Mortality after coronary artery bypass versus percutaneous coronary intervention with stenting for coronary artery disease: A pooled analysis of individual patient data. Lancet 2018, 391, 939–948. [Google Scholar] [CrossRef] [PubMed]
- Criqui, M.H.; Matsushita, K.; Aboyans, V.; Hess, C.N.; Hicks, C.W.; Kwan, T.W.; McDermott, M.M.; Misra, S.; Ujueta, F. Lower extremity peripheral artery disease: Contemporary epidemiology, management gaps, and future directions: A scientific statement from the American Heart Association. Circulation 2021, 144, e171–e191. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, T.; Ishida, N.; Takaoka, M.; Tsujimoto, K.; Kondo, K.; Isoda, R.; Yukawa, T.; Tokunaga, N.; Ishida, A.; Fukazawa, T.; et al. Bioelectrical impedance analysis for perioperative water management in adult cardiovascular valve disease surgery. Surg. Today 2021, 51, 1061–1067. [Google Scholar] [CrossRef] [PubMed]
- Ochiai, Y.; Watanabe, T.; Ohashi, I.; Katayama, H.; Ishida, N.; Hayashi, M.; Takaoka, M.; Kuinose, M.; Sugimoto, K.; Toda, Y.; et al. Analysis of water balance for perioperative management in coronary artery bypass grafting. Kawasaki Med. J. 2021, 47, 55–62. [Google Scholar]
- Benjamin, E.J.; Blaha, M.J.; Chiuve, S.E.; Cushman, M.; Das, S.R.; Deo, R.; de Ferranti, S.D.; Floyd, J.; Fornage, M.; Gillespie, C.; et al. Heart disease and stroke statistics—2017 update: A report from the American Heart Association. Circulation 2017, 135, e146–e603. [Google Scholar] [CrossRef] [PubMed]
- Alraies, M.C.; Eckman, P. Adult heart transplant: Indications and outcomes. J. Thorac. Dis. 2014, 6, 1120–1128. [Google Scholar]
- Messer, S.; Large, S. Resuscitating heart transplantation: The donation after circulatory determined death donor. Eur. J. Cardiothorac. Surg. 2016, 49, 1–4. [Google Scholar] [CrossRef]
- Inamdar, A.; Inamdar, C. Heart failure: Diagnosis, management, and utilization. J. Clin. Med. 2016, 5, 62. [Google Scholar] [CrossRef] [PubMed]
- Hobbs, R. Clinical burden and health service challenges of chronic heart failure. Br. J. Gen. Pract. 2010, 60, 611–615. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cowie, M.; Anker, S.D.; Cleland, J.G.F.; Felker, J.G.M.; Filippatos, G.; Jaarsma, T.; Jourdain, P.; Knight, E.; Massie, B.; Ponikowski, P.; et al. Improving care for patients with acute heart failure: Before, during and after hospitalization. ESC Heart Fail. 2014, 1, 110–145. [Google Scholar] [CrossRef] [PubMed]
- Voigt, J.; Sasha, J.M.; Taylor, A.; Krucoff, M.; Reynolds, M.R.; Gibson, M. A reevaluation of the costs of heart failure and its implications for the allocation of health resources in the United States. Clin. Cardiol. 2014, 37, 312–321. [Google Scholar] [CrossRef] [PubMed]
- Khatibzadeh, S.; Farzadfar, F.; Oliver, J.; Ezzati, M.; Moran, A. Worldwide risk factors for heart failure: A systematic review and pooled analysis. Int. J. Cardiol. 2013, 168, 1186–1194. [Google Scholar] [CrossRef]
- Mamode, N.; Scott, R.N. Graft type for femoro-popliteal bypass surgery. Cochrane Database Syst. Rev. 2000, 2, CD001487. [Google Scholar]
- Pugsley, M.K.; Tabrizchi, R. The vascular system. An overview of structure and function. J. Pharmacol. Toxicol. Methods 2000, 44, 333–340. [Google Scholar] [CrossRef]
- Diener, H.; Hellwinklel, O.; Carpenter, S.; Avellaneda, A.L.; Debus, E.S. Homografts and extra-anatomical reconstructions for infected vascular grafts. J. Cardiovasc. Surg. 2014, 55, 217–223. [Google Scholar]
- Kurobe, H.; Maxfield, M.W.; Breuer, C.K.; Shinoka, T. Concise review: Tissue-engineered. Vascular grafts for cardiac surgery: Past, present, and future. Stem Cells Transl. Med. 2012, 1, 566–571. [Google Scholar] [CrossRef]
- O’Donnell, A.; Yutzey, K.E. Mechanisms of heart valve development and diseases. Development 2020, 147, dev183020. [Google Scholar] [CrossRef]
- Salaun, E.; Clavel, M.A.; Rodes-Cabau, J.; Pibarot, P. Bioprosthetic aortic valve durability in the era of transcatheter aortic valve implantation. Heart 2018, 104, 1323–1332. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.; Basu, A.; Di Scenza, G.; Bartlett, J.; Fan, K.S.; Oo, S.; Harky, A. Understanding aortic valve repair through Ozaki procedure: A review of literature evidence. J. Card. Surg. 2022, 37, 5202–5206. [Google Scholar] [CrossRef]
- Westaby, S. Coronary revascularization in ischemic cardiomyopathy. Surg. Clin. N. Am. 2004, 84, 179–199. [Google Scholar] [CrossRef] [PubMed]
- Sayers, J.R.; Riley, P.R. Heart regeneration: Beyond new muscle and vessels. Cardiovasc. Res. 2021, 117, 727–742. [Google Scholar] [CrossRef] [PubMed]
- Muller, P.; Lemcke, H.; David, R. Stem cell therapy in heart diseases—Cell types, mechanisms, and improvement strategies. Cell. Physiol. Biochem. 2018, 48, 2607–2655. [Google Scholar] [CrossRef] [PubMed]
- Shafiee, A.; Atala, A. Tissue Engineering: Toward a New Era of Medicine. Annu. Rev. Med. 2017, 68, 29–40. [Google Scholar] [CrossRef]
- Fukuno, Y.; Usui, M.; Underwood, R.A.; Isenhath, S.; Marshall, A.J.; Hauch, K.D.; Ratner, B.D.; Olerud, J.E.; Fleckman, P. Epidermal and dermal integration into sphere-templated porous poly(2-hydroxyethyl methacrylate) implants in mice. J. Biomed. Mater. Res. A 2010, 94, 1172–1186. [Google Scholar] [CrossRef]
- Annabi, N.; Nichol, J.W.; Zhong, X.; Ji, C.; Koshy, C.; Khademhosseini, A. Controlling the porosity and microarchitecture of hydrogels for tissue engineering. Tissue Eng. Part B Rev. 2010, 16, 371–383. [Google Scholar] [CrossRef]
- Sharkaway, A.A.; Klitzmann, B.; Truskey, G.A.; Reichert, W.M. Engineering the tissue which encapsulates subcutaneous implants. I. Diffusion properties. J. Biomed. Mater. Res. 1997, 37, 401–412. [Google Scholar] [CrossRef]
- Galperin, A.; Long, T.J.; Ratner, B.D. Degradable, thermo-sensitive poly(N-isopropyl acrylamide)-based scaffolds with controlled porosity for tissue engineering applications. Biomacromolecules 2010, 11, 2583–2592. [Google Scholar] [CrossRef]
- Sharkawy, A.A.; Klitzman, B.; Truskey, G.A.; Reichart, W.M. Engineering the tissue which encapsulates subcutaneous implants. II. Plasma-tissue exchange properties. J. Biomed. Mater. Res. 1998, 40, 586–597. [Google Scholar] [CrossRef]
- Sussman, E.M.; Halpin, M.C.; Muster, J.; Moon, R.T.; Ratner, B.D. Porous implants modulate healing and induce shifts in local macrophage polarization in the foreign body reaction. Ann. Biomed. Eng. 2014, 42, 1508–1516. [Google Scholar] [CrossRef] [PubMed]
- Karp, R.D.; Johnson, K.H.; Buoen, L.C.; Ghobrial, H.K.; Brand, I.; Brand, K.G. Tumorigenesis by Millipore filters in mice: Histology and ultrastructure of tissue reactions as related to pore size. Natl. Cancer Inst. 1973, 51, 1275–1285. [Google Scholar] [CrossRef] [PubMed]
- Brauker, J.H.; CarroBrendel, V.E.; Martinson, L.A.; Crudele, J.; Johnston, W.D.; Johnson, R.C. Neovascularization of synthetic membranes directed by membrane microarchitecture. J. Biomed. Mater. Res. 1995, 29, 1517–1524. [Google Scholar] [CrossRef]
- Sayed, E.; Haj-Ahmad, R.; Ruparelia, K.; Arshad, M.S.; Chang, M.; Ahmad, Z. Porous inorganic drug delivery systems—A review. AAPS PharmSciTech 2017, 18, 1507–1525. [Google Scholar] [CrossRef]
- He, F.; Li, D.; He, J.; Liu, Y.; Ahmad, F.; Liu, Y.; Deng, X.; Ye, Y.; Yin, D. A novel layer-structures scaffold with large pore sizes suitable for 3D cell culture prepared by near field electrospinning. Mater. Sci. Eng. C 2018, 86, 18–27. [Google Scholar] [CrossRef]
- Tylek, T.; Blum, C.; Hrynevich, A.; Schlegelmilch, K.; Schilling, T.; Dalton, P.D.; Groll, J. Precisely defined fiber scaffolds with 40um porosity induce elongation driven M2-like polarization of human macrophages. Biofabrication 2020, 12, 025007. [Google Scholar] [CrossRef]
- Li, S.; Deng, B.; Grinthal, A.; Schneider-Yamamura, A.; Kang, J.; Martens, R.S.; Zhang, C.T.; Li, J.; Yu, S.; Bertoldi, K.; et al. Liquid-induced topological transformations of cellular microstructures. Nature 2021, 592, 386–391. [Google Scholar] [CrossRef]
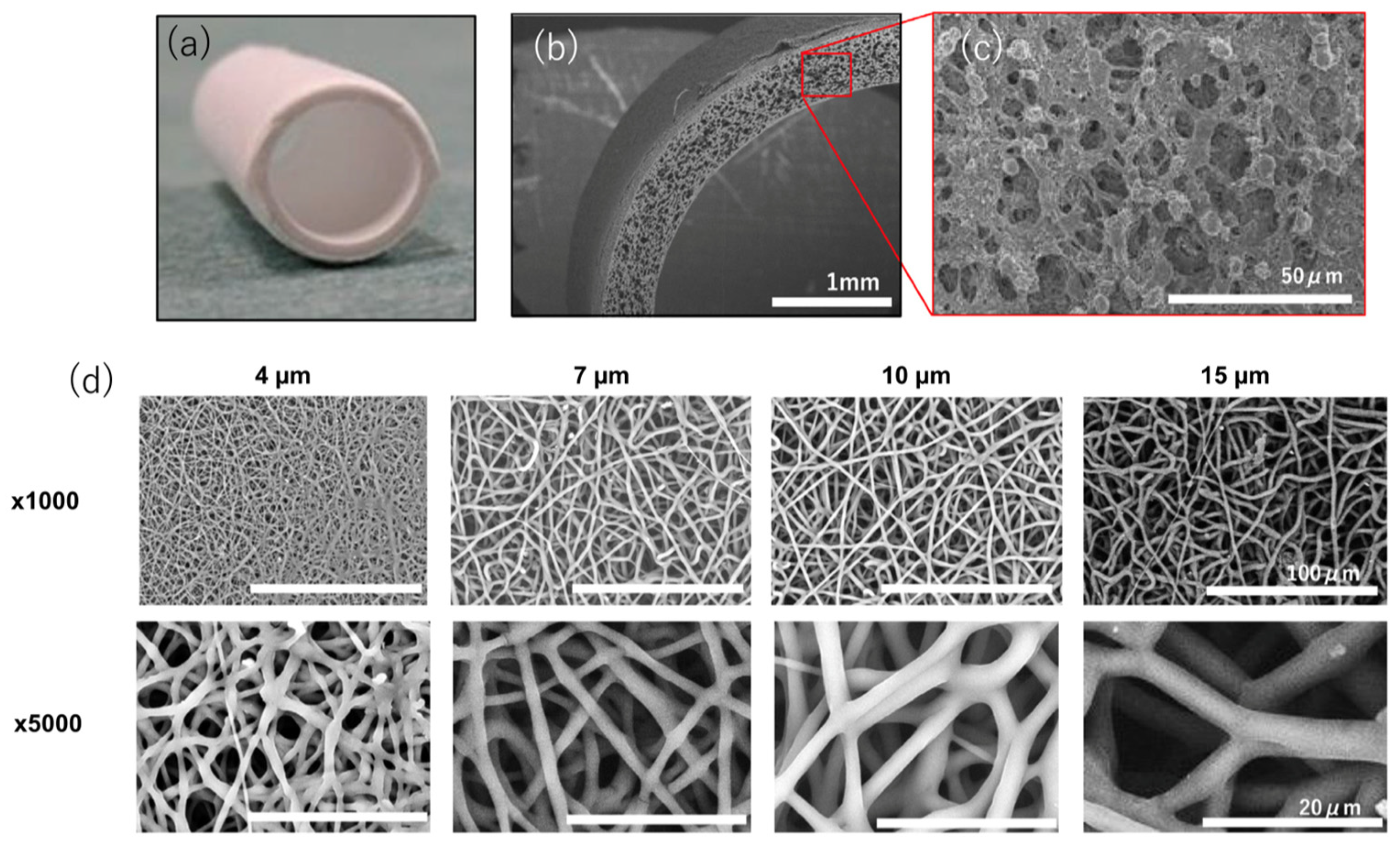
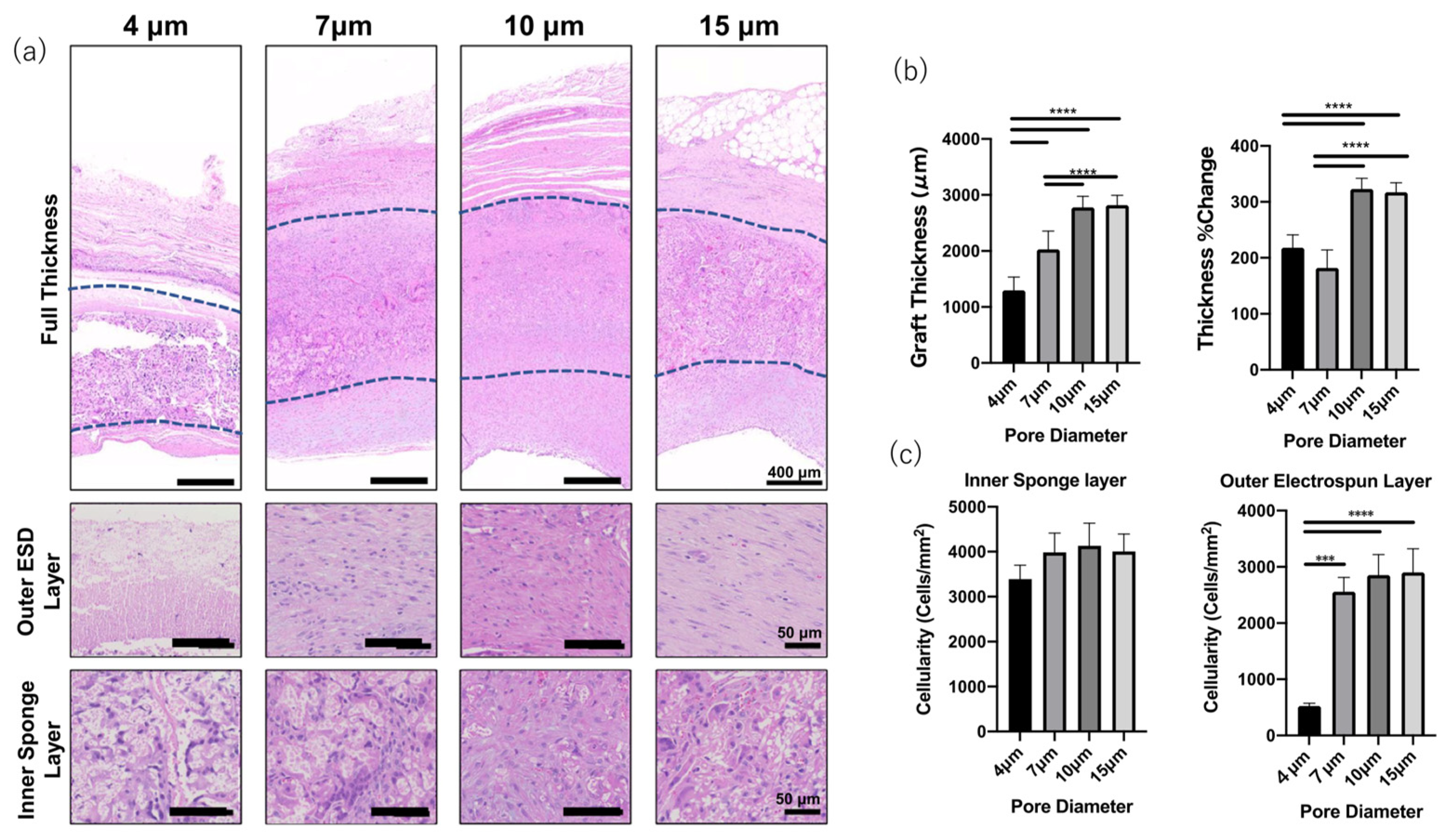
- Matsuzaki, Y.; Iwaki, R.; Reinhardt, J.W.; Chang, J.C.; Miyamoto, S.; Kelly, J.; Zbinden, J.; Blum, K.; Mirhaidari, G.; Ulziibayer, A.; et al. The effect of pore diameter on neo-tissue formation in electrospun biodegradable tissue-engineered arterial grafts in a large animal model. Acta Biomater. 2020, 115, 176–184. [Google Scholar] [CrossRef]
- Garg, T.; Goyal, A.K. Biomaterial-based scaffolds—Current status and future directions. Expert Opin. Drug Deliv. 2014, 11, 767–789. [Google Scholar] [CrossRef]
- Braunecker, J.; Baba, M.; Milroy, G.E.; Cameron, R.E. The effects of molecular weight and porosity on the degradation and drug release from polyglycolide. Int. J. Pharm. 2004, 282, 19–34. [Google Scholar] [CrossRef] [PubMed]
- Recum, A.F.; Shannon, C.E.; Cannon, C.E.; Long, K.J.; Kooten, T.G.; Meyle, J. Surface roughness, porosity, and texture as modifiers of cellular adhesion. Tissue Eng. 1996, 2, 241–253. [Google Scholar] [CrossRef] [PubMed]
- Ozpinar, E.W.; Frey, A.L.; Cruse, G.; Freytes, D.O. Mast cell-biomaterial interactions and tissue repair. Tissue Eng. Part B Rev. 2021, 27, 590–603. [Google Scholar] [CrossRef] [PubMed]
- Doloff, J.C.; Veiseh, O.; Mezerville, R.; Sforza, M.; Perry, T.A.; Haupt, J.; Jamiel, M.; Chambers, C.; Nash, A.; Fotovat, A.S.; et al. The surface topography of silicone breast implants mediates the foreign body response in mice, rabbits, and humans. Nat. Biomed. Eng. 2021, 5, 1115–1130. [Google Scholar] [CrossRef]
- Khorshidi, S.; Solouk, A.; Mirzadeh, H.; Mazinani, S.; Lagaron, J.M.; Sharifi, S.; Ramakrishna, S. A review of critical challenges of electrospun scaffolds for tissue-engineering applications. J. Tissue Eng. Regen. Med. 2016, 10, 715–738. [Google Scholar] [CrossRef]
- Hernandez, J.L.; Woodrow, K.A. Medical applications of porous biomaterials: Features of porosity and tissue-specific implications for biocompatibility. Adv. Health Mater. 2022, 11, e2102087. [Google Scholar] [CrossRef]
- Koch, L.; Drenckchan, W.; Stubenrauch, C. Porous polymers via emulsion templating: Pore deformation during solidification cannot be explained by an osmotic transport! Colloid Polym. Sci. 2021, 299, 233–242. [Google Scholar] [CrossRef]
- Zhao, P.; Wang, J.; Li, Y.; Wang, X.; Chen, C.; Liu, G. Microfluidic technology for the production of well-ordered porous polymer scaffolds. Polymers 2020, 12, 1863. [Google Scholar] [CrossRef]
- Ngo, T.D.; Kashani, A.; Imbalzano, G.; Nguyen, K.T.Q.; Hui, D. Additive manufacturing (3D printing): A review of materials, methods, applications, and challenges. Compos. Part B 2018, 143, 172–196. [Google Scholar] [CrossRef]
- Chou, S.F.; Cardon, D.; Woodrow, K.A. Current strategies for sustaining drug release from electrospun nanofibers. J. Control. Release 2015, 220, 584–591. [Google Scholar] [CrossRef]
- Stock, U.A.; Mayer, J.E., Jr. Tissue engineering of cardiac valves on the basis of PGA/PLA Copolymers. J. Long Term Eff. Med. Implants. 2001, 11, 249–260. [Google Scholar] [CrossRef] [PubMed]
- Asiri, A.M.; Marwani, H.M.; Khan, S.B.; Webster, T.J. Greater cardiomyocyte density on aligned compared with random carbon nanofibers in polymer composites. Int. J. Nanomed. 2014, 9, 5533–5539. [Google Scholar]
- Hibino, N.; Imai, Y.; Shin-Oka, T.; Aoki, M.; Watanabe, M.; Kosaka, Y.; Matsumura, G.; Konuma, T.; Toyama, S.; Murata, A.; et al. First successful clinical application of tissue engineered blood vessel. Kyobu Geka 2002, 55, 368–373. [Google Scholar] [PubMed]
- Naito, Y.; Shinoka, T.; Duncan, D.; Hibino, N.; Solomon, D.; Cleary, M.; Rathore, A.; Fein, C.; Church, S.; Breuer, C. Vascular Tissue Engineering: Towards the next Generation Vascular Grafts. Adv. Drug Deliv. Rev. 2011, 63, 312–323. [Google Scholar] [CrossRef]
- Leal, B.B.J.; Wakabayashi, N.; Oyama, K.; Kamiya, H.; Braghirolli, D.I.; Pranke, P. Vascular Tissue Engineering: Polymers and Methodologies for Small Caliber Vascular Grafts. Front. Cardiovasc. Med. 2021, 7, 592361. [Google Scholar] [CrossRef]
- Ong, C.S.; Fukunishi, T.; Liu, R.H.; Nelson, K.; Zhang, H.; Wieczorek, E.; Palmieri, M.; Ueyama, Y.; Ferris, E.; Geist, G.E.; et al. Bilateral Arteriovenous Shunts as a Method for Evaluating Tissue-Engineered Vascular Grafts in Large Animal Models. Tissue Eng. Part C Methods 2017, 23, 728–735. [Google Scholar] [CrossRef]
- Hu, Y.T.; Pan, X.D.; Zheng, J.; Ma, W.G.; Sun, L.Z. In Vitro and in Vivo Evaluation of a Small-Caliber Coaxial Electrospun Vascular Graft Loaded with Heparin and VEGF. Int. J. Surg. 2017, 44, 244–249. [Google Scholar] [CrossRef]
- Mahara, A.; Somekawa, S.; Kobayashi, N.; Hirano, Y.; Kimura, Y.; Fujisato, T.; Yamaoka, T. Tissue-Engineered Acellular Small Diameter Long-Bypass Grafts With neointima-Inducing Activity. Biomaterials 2015, 58, 54–62. [Google Scholar] [CrossRef]
- Bouchet, M.; Gauthier, M.; Maire, M.; Ajji, A.; Lerouge, S. Towards Compliant Small-Diameter Vascular Grafts: Predictive Analytical Model and Experiments. Mater. Sci. Eng. C 2019, 100, 715–723. [Google Scholar] [CrossRef]
- Fang, Z.; Xiao, Y.; Geng, X.; Jia, L.; Xing, Y.; Ye, L.; Gu, Y.; Zhang, A.-Y.; Feng, Z.-G. Fabrication of Heparinized Small Diameter TPU/PCL Bi-Layered Artificial Blood Vessels and in Vivo Assessment in a Rabbit Carotid Artery Replacement Model. Mater. Sci. Eng. C 2022, 133, 112628. [Google Scholar] [CrossRef]
- Lee, C.H.; Singla, A.; Lee, Y. Biomedical Applications of Collagen. Int. J. Pharm. 2001, 221, 1–22. [Google Scholar] [CrossRef]
- Jakab, K. Tissue engineering by self-assembly of cells printed into topologically defined structures. Tissue Eng. Part A 2008, 14, 413–421. [Google Scholar] [CrossRef] [PubMed]
- Laurent, S.; Boutouyrie, P.; Lacolley, P. Structural and Genetic Bases of Arterial Stiffness. Hypertension 2005, 45, 1050–1055. [Google Scholar] [CrossRef] [PubMed]
- Daamen, W.F.; Veerkamp, J.H.; van Hest, J.C.M.; van Kuppevelt, T.H. Elastin as a Biomaterial for Tissue Engineering. Biomaterials 2007, 28, 4378–4398. [Google Scholar] [CrossRef]
- Chan, A.H.P.; Filipe, E.C.; Tan, R.P.; Santos, M.; Yang, N.; Hung, J.; Feng, J.; Nazir, S.; Benn, A.J.; Ng, M.K.C.; et al. Altered Processing Enhances the Efficacy of Small-Diameter Silk Fibroin Vascular Grafts. Sci. Rep. 2019, 9, 17461. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nitta, S.K.; Numata, K. Biopolymer-Based Nanoparticles for Drug/Gene Delivery and Tissue Engineering. Int. J. Mol. Sci. 2013, 14, 1629–1654. [Google Scholar] [CrossRef] [PubMed]
- Altman, G.H.; Diaz, F.; Jakuba, C.; Calabro, T.; Horan, R.L.; Chen, J.; Lu, H.; Richmond, J.; Kaplan, D. L Silk-Based Biomaterials. Biomaterials 2003, 24, 401–416. [Google Scholar] [CrossRef]
- Aytemiz, D.; Sakiyama, W.; Suzuki, Y.; Nakaizumi, N.; Tanaka, R.; Ogawa, Y.; Takagi, Y.; Nakazawa, Y.; Asakura, T. Small-Diameter Silk Vascular Grafts (3 Mm Diameter) with a Double-Raschel Knitted Silk Tube Coated with Silk Fibroin Sponge. Adv. Healthc. Mater. 2013, 2, 361–368. [Google Scholar] [CrossRef]
- Croisier, F.; Jérôme, C. Chitosan-Based Biomaterials for Tissue Engineering. Eur. Polym. J. 2013, 49, 780–792. [Google Scholar] [CrossRef]
- VandeVord, P.J.; Matthew, H.W.T.; DeSilva, S.P.; Mayton, L.; Wu, B.; Wooley, P.H. Evaluation of the Biocompatibility of a Chitosan Scaffold in Mice. J. Biomed. Mater. Res. 2002, 59, 585–590. [Google Scholar] [CrossRef]
- Zhang, H.; Neau, S.H. In vitro degradation of chitosan by a commercial enzyme preparation: Effect of molecular weight and degree of deacetylation. Biomaterials 2001, 22, 1653–1658. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.M.; Hu, W.; Wang, X.D.; Gu, X.S. The controlling biodegradation of chitosan fibers by N-acetylation in vitro and in vivo. J. Mater. Sci. Mater. Med. 2007, 18, 2117–2121. [Google Scholar] [CrossRef] [PubMed]
- Fukunishi, T.; Best, C.A.; Sugiura, T.; Shoji, T.; Yi, T.; Udelsman, B.; Ohst, D.; Ong, C.S.; Zhang, H.; Shinoka, T.; et al. Tissue-engineered small diameter arterial vascular grafts from cell-free nanofiber PCL/Chitosan scaffoldsin a sheep model. PLoS ONE 2016, 11, e015855. [Google Scholar]
- Wu, Y.; Qin, Y.; Wang, Z.; Wang, J.; Zhang, C.; Li, C.; Kong, D. The Regeneration of Macro-Porous Electrospun Poly(ε-Caprolactone) Vascular Graft during Long-Term in Situ Implantation. J. Biomed. Mater. Res. Part B Appl. Biomater. 2018, 106, 1618–1627. [Google Scholar] [CrossRef] [PubMed]
- Weinberg, C.B.; Bell, E. A Blood Vessel Model Constructed from Collagen and Cultured Vascular Cells. Science 1986, 231, 397–400. [Google Scholar] [CrossRef]
- L’Heureux, N.; Pâquet, S.; Labbé, R.; Germain, L.; Auger, F.A. A Completely Biological Tissue-engineered Human Blood Vessel. FASEB J. 1998, 12, 47–56. [Google Scholar]
- Zhang, W.J.; Liu, W.; Cui, L.; Cao, Y. Tissue Engineering of Blood Vessel. J. Cell. Mol. Med. 2007, 11, 945–957. [Google Scholar] [CrossRef] [PubMed]
- Benrashid, E.; Mccoy, C.C.; Youngwirth, L.M.; Kim, J.; Manson, R.J.; Otto, J.C.; Lawson, J.H. Tissue Engineered Vascular Grafts: Origins, Development, and Current Strategies for Clinical Application. Methods 2016, 99, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Ben-shaul, S.; Landau, S.; Merdler, U.; Levenberg, S. Mature Vessel Networks in Engineered Tissue Promote Graft–HostAnastomosis and Prevent Graft Thrombosis. Proc. Natl. Acad. Sci. USA 2019, 116, 2955–2960. [Google Scholar] [CrossRef]
- Neufurth, M.; Wang, X.; Tolba, E.; Dorweiler, B.; Schröder, H.; Link, T.; Diehl-Seifert, B.; Müller, W. Modular Small DiameterVascular Grafts with Bioactive Functionalities. PLoS ONE 2015, 10, e0133632. [Google Scholar]
- DeValence, S.; Tille, J.C.; Mugnai, D.; Mrowczynski, W.; Gurny, R.; Moller, M.; Walpoth, B.H. Long term performance of polycaprolactone vascular graft in a rat aorta replacement model. Biomaterials 2012, 33, 38–47. [Google Scholar] [CrossRef] [PubMed]
- Shinoka, T.; Imai, Y.; Ikeda, Y. Transplantation of a tissue engineered pulmonary artery. N. Engl. J. Med. 2001, 344, 532–533. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Lei, D.; Zou, H.; Huang, S.; Yang, Q.; Li, S.; Qing, F.L.; Ye, X.; You, Z.; Zhao, Q. Hybrid electrospun rapamycin-loaded small-diameter decellularized vascular grafts effectively inhibit intimal hyperplasia. Acta Biomater. 2019, 97, 321–332. [Google Scholar] [CrossRef] [PubMed]
- Morton, H.F. Variability of arterial wall shear stress, its dependence on vessel diameter, and implications for Murray’s law. Atherosclerosis 2009, 203, 47–48. [Google Scholar]
- Innocente, F.; Mandracchia, D.; Pektok, E.; Nottelet, B.; Tille, J.C.; de Valence, S.; Faggin, G.; Mazzucco, A.; Kalangos, A.; Gurny, R.; et al. Paclitaxel eluting biodegradable synthetic vascular prostheses: A step to wards reduction of neointima formation? Circulation 2009, 120, S37–S45. [Google Scholar] [CrossRef]
- Zheng, W.; Wang, Z.; Song, L.; Zhao, Q.; Zhang, J.; Li, D.; Wang, S.; Han, J.; Zheng, X.L.; Yang, Z.; et al. Endothelialization and patency of RGD-functionalized vascular grafts in a rabbit carotid artery model. Biomaterials 2012, 33, 2880–2891. [Google Scholar] [CrossRef]
- Khairy, P.; Poirier, N. Is the Extracardiac Conduit the Preferred Fontan Approach for Patients With Univentricular Hearts? Circulation 2012, 126, 2516–2525. [Google Scholar] [CrossRef]
- Bezuska, L.; Lebetkevicius, V.; Sudikiene, R.; Liekiene, D.; Tarutis, V. 30-year experience of Fontan surgery: Single-centre’s data. J. Cardiothorac. Surg. 2017, 12, 67. [Google Scholar] [CrossRef]
- Hibino, N.; McGillicuddy, E.; Matsumura, G.; Ichihara, Y.; Naito, Y.; Breuer, C.; Shinoka, T. Late-term results of tissue-engineeredvascular grafts in humans. J. Thorac. Cardiovasc. Surg. 2010, 139, 431–436.e2. [Google Scholar] [CrossRef] [Green Version]
- Sugiura, T.; Matsumura, G.; Miyamoto, S.; Miyachi, H.; Breuer, C.K.; Shinoka, T. Tissue-engineered Vascular Grafts in Children with Congenital Heart Disease: Intermediate Term Follow-up. Semin. Thorac. Cardiovasc. Surg. 2018, 30, 175–179. [Google Scholar] [CrossRef]
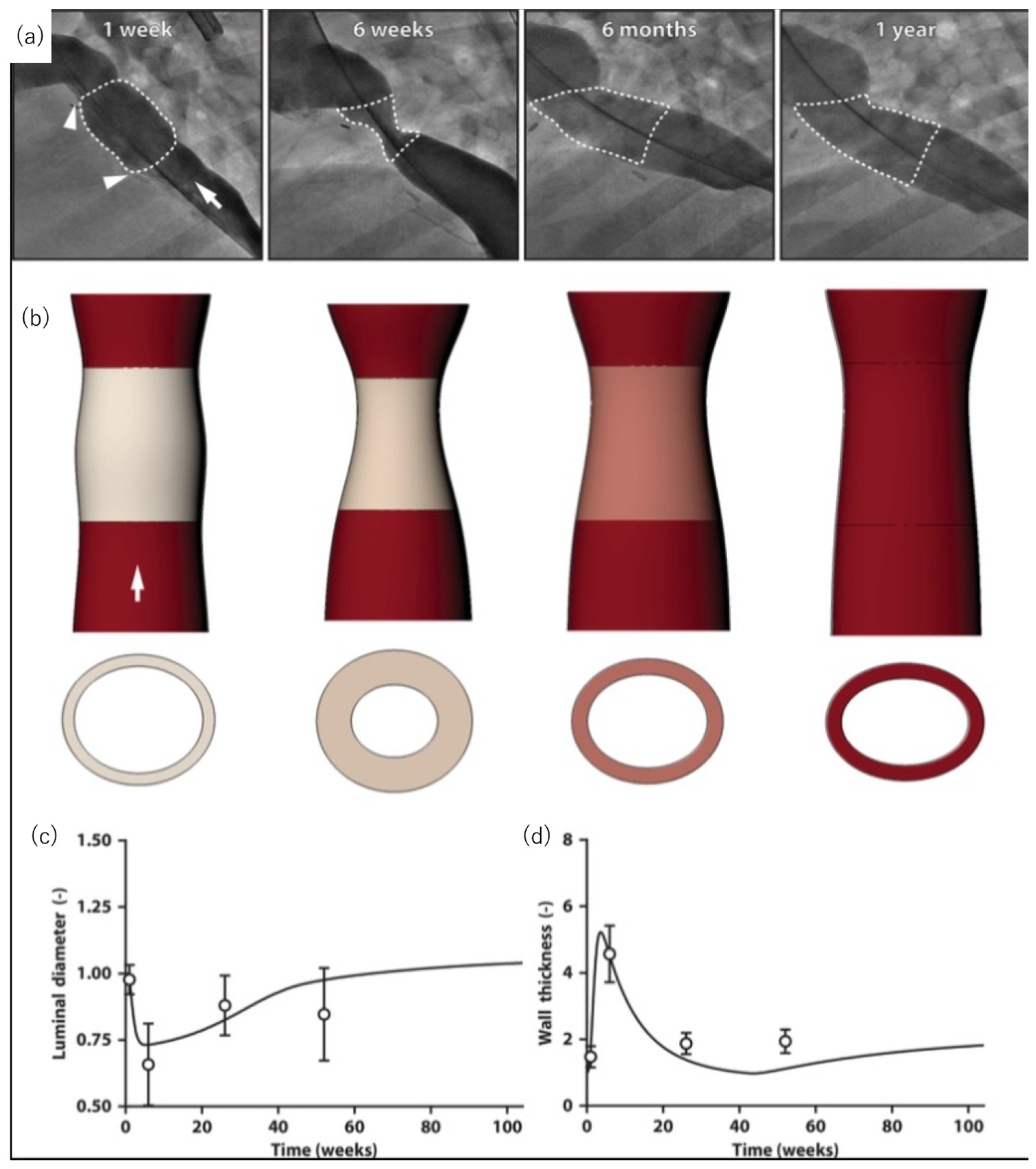
- Szafron, J.M.; Khosravi, R.; Reinhardt, J.; Best, C.A.; Bersi, M.R.; Yi, T.; Breuer, C.K.; Humphrey, J.D. Immuno-driven and Mechano-mediated Neotissue Formation in Tissue Engineered Vascular Grafts. Ann. Biomed. Eng. 2018, 46, 1938–1950. [Google Scholar] [CrossRef]
- Drews, J.D.; Pepper, V.K.; Best, C.A.; Szafron, J.M.; Cheatham, J.P.; Yates, A.R.; Hor, K.N.; Zbinden, J.C.; Chang, Y.-C.; Mirhaidari, G.J.M.; et al. Spontaneous reversal of stenosis in tissue-engineered vascular grafts. Sci. Transl. Med. 2020, 12, eaax6919. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://clinicaltrials.gov/ (accessed on 28 January 2023).
- Dijkman, P.E.; Fioretta, E.S.; Frese, L.; Pasqualini, F.S.; Hoerstrup, S.P. Heart valve replacements with regenerative capacity. Transfus. Med. Hemother. 2016, 43, 282–290. [Google Scholar] [CrossRef] [PubMed]
- Jana, S.; Tefft, B.J.; Spoon, D.B.; Simari, R.D. Scaffolds for tissue engineering of cardiac valves. Acta Biomater. 2014, 10, 2877–2893. [Google Scholar] [CrossRef] [PubMed]
- Kluin, J.; Talacua, H.; Smits, A.; Emmert, M.Y.; Brugmans, M.C.P.; Fioretta, E.S.; Dijkman, P.E.; Sontjens, S.H.M.; Duijvelshoff, R.; Dekker, S.; et al. In situ heart valve tissue engineering using a bioresorbable elastomeric implant—From material design to 12 months follow-up in sheep. Biomaterials 2017, 125, 101–117. [Google Scholar] [CrossRef]
- Soliman, O.I.; Miyazaki, Y.; Abdelghani, M.; Brugmans, M.; Witsenburg, M.; Onuma, Y.; Cox, M.; Serruys, P.W. Midterm performance of a novel restorative pulmonary valved conduit: Preclinical results. EuroIntervention 2017, 13, e1418–e1427. [Google Scholar] [CrossRef]
- Capulli, A.K.; Emmert, M.Y.; Pasqualini, F.S.; Kehl, D.; Caliskan, E.; Lind, J.U.; Sheehy, S.P.; Park, S.J.; Ahn, S.; Weber, B.; et al. JetValve: Rapid manufacturing of biohybrid scaffolds for biomimetic heart valve replacement. Biomaterials 2017, 133, 229–241. [Google Scholar] [CrossRef]
- Miyazaki, Y.; Soliman, O.I.I.; Abdelghani, M.; Katsikis, A.; Naz, C.; Lopes, S.; Warnack, B.; Cox, M.; Onuma, Y.; Serruys, P.W. Acute performance of a novel restorative transcatheter aortic valve: Preclinical results. EuroIntervention 2017, 13, e1410–e1417. [Google Scholar] [CrossRef]
- Bennink, G.; Trii, S.; Brugmans, M.; Cox, M.; Svanidze, O.; Ladich, E.; Carrel, T.; Virmani, R. A novel restorative pulmonary valved conduit in a chronic sheep model: Mid-term hemodynamic function and histologic assessment. J. Thorac. Cardiovasc. Surg. 2018, 155, 2591–2601e3. [Google Scholar] [CrossRef]
- Coyan, G.N.; D’Amore, A.; Matsumura, Y.; Pedersen, D.D.; Luketich, S.K.; Shanov, V.; Katz, W.E.; David, T.E.; Wagner, W.R.; Badhwar, V. In vivo functional assessment of a novel degradable metal and elastomeric scaffold-based tissue engineered heart valve. J. Thorac. Cardiovasc. Surg. 2019, 157, 1809–1816. [Google Scholar] [CrossRef]
- Weber, B.; Scherman, J.; Emmert, M.Y.; Gruenenfelder, J.; Verbeek, R.; Bracher, M.; Black, M.; Kortsmit, J.; Franz, T.; Schoenauer, R.; et al. Injectable living marrow stromal cell-based autologous tissue engineered heart valves: First experiences with a one-step intervention in primates. Eur. Heart J. 2011, 32, 2830–2840. [Google Scholar] [CrossRef] [PubMed]
- Emmert, M.Y.; Weber, B.; Behr, L.; Frauenfelder, T.; Brokopp, C.E.; Grunenfelder, J.; Falk, V.; Hoerstrup, S.P. Transapical aortic implantation of autologous marrow stromal cell-based tissue-engineered heart valves: First experiences in the systemic circulation. JACC Cardiovasc. Interv. 2011, 4, 822–823. [Google Scholar] [CrossRef] [PubMed]
- Emmert, M.Y.; Weber, B.; Wolint, P.; Behr, L.; Sammut, S.; Frauenfelder, T.; Frese, L.; Scherman, J.; Brokopp, C.E.; Templin, C.; et al. Stem cell-based transcatheter aortic valve implantation: First experiences in a preclinical model. JACC Cardiovasc. Interv. 2012, 5, 874–883. [Google Scholar] [CrossRef] [PubMed]
- Emmert, M.Y.; Weber, B.; Behr, L.; Sammut, S.; Frauenfelder, T.; Wolint, P.; Scherman, J.; Bettex, D.; Gruenfelder, J.; Falk, V.; et al. Transcatheter aortic valve implantation using anatomically oriented, marrow stromal cell-based, stented, tissue-engineered heart valves: Technical considerations and implications for translational cell-based heart valve concepts. Eur. J. Cardiothorac. Surg. 2014, 45, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Fioretta, E.S.; Lintas, V.; Mallone, A.; Motta, S.E.; von Boehmer, L.; Dijkman, P.E.; Cesarovic, N.; Caliskan, E.; Biefer, H.R.C.; Lipiski, M.; et al. Differential leaflet remodeling of bone marrow cell pre-seeded versus nonseeded bioresorbable transcatheter pulmonary valve replacements. JACC Basic Transl. Sci. 2019, 5, 15–31. [Google Scholar] [CrossRef] [PubMed]
- Fioretta, E.; Putti, M.; Fallahi, A.; Mes, T.; Bosman, A.; Caliskan, E.; Cesarovic, N.; Rodriguez, H.; Dnakers, P.; Bouten, C.; et al. A multidisciplinary study to develop a transcatheter aortic valve implantation system for in situ heart valve tissue engineering. Struct. Heart 2020, 4, 57. [Google Scholar] [CrossRef]
- US National Library of Medicine. ClinicalTrials.gov. 2016. Available online: https://clinicaltrials.gov/ct2/show/NCT02700100 (accessed on 28 January 2023).
- Morales, D.L.; Herrington, C.; Bacha, E.A.; Morell, V.O.; Prodan, Z.; Mroczek, T.; Sivalingam, S.; Cox, M.; Bennink, G.; Asch, F.M. A novel restorative pulmonary valve conduit: Early outcomes of two clinical trials. Front. Cardiovasc. Med. 2021, 4, 583360. [Google Scholar] [CrossRef]
- US National Library of Medicine. ClinicalTrials.gov. 2017. Available online: https://clinicaltrials.gov/ct2/show/NCT03022708 (accessed on 23 January 2023).
- Gaetani, R.; Zizzi, E.A.; Deriu, M.A.; Morbiducci, U.; Pesce, M.; Messina, E. When Stiffness Matters: Mechanosensing in Heart Development and Disease. Front. Cell Dev. Biol. 2020, 8, 334. [Google Scholar] [CrossRef]
- Chaudhuri, O.; Cooper-White, J.; Janmey, P.A.; Mooney, D.J.; Shenoy, V.B. Effects of extracellular matrix viscoelasticity on cellular behaviour. Nature 2020, 584, 535–546. [Google Scholar] [CrossRef]
- Darnell, M.; O’Neil, A.; Mao, A.; Gu, L.; Rubin, L.L.; Mooney, D.J. Material microenvironmental properties couple to induce distinct transcriptional programs in mammalian stem cells. Proc. Natl. Acad. Sci. USA 2018, 115, E8368–E8377. [Google Scholar] [CrossRef]
- Seo, B.R.; Chen, X.; Ling, L.; Song, Y.H.; Shimpi, A.A.; Choi, S.; Gonzalez, J.; Sapudom, J.; Wang, K.; Andresen Eguiluz, R.C.; et al. Collagen microarchitecture mechanically controls myofibroblast differentiation. Proc. Natl. Acad. Sci. USA 2020, 117, 11387–11398. [Google Scholar] [CrossRef] [PubMed]
- Carson, D.; Hnilova, M.; Yang, X.; Nemeth, C.L.; Tsui, J.H.; Smith, A.S.; Jiao, A.; Regnier, M.; Murry, C.E.; Tamerler, C.; et al. Nanotopography-Induced Structural Anisotropy and Sarcomere Development in Human Cardiomyocytes Derived from Induced Pluripotent Stem Cells. ACS Appl. Mater. Interfaces 2016, 8, 21923–21932. [Google Scholar] [CrossRef] [PubMed]
- Jang, Y.; Park, Y.; Kim, K. Engineering biomaterials to guide heart cells for matured cardiac tissue. Coatings 2020, 10, 925. [Google Scholar] [CrossRef]
- Zhang, J.; Zhu, W.; Radisic, M.; Vunjak-Novakovic, G. Can We Engineer a Human Cardiac Patch for Therapy? Circ. Res. 2018, 123, 244–265. [Google Scholar] [CrossRef]
- Nicolas, J.; Magli, S.; Rabbachin, L.; Sampaolesi, S.; Nicotra, F.; Russo, L. 3D Extracellular Matrix Mimics: Fundamental Concepts and Role of Materials Chemistry to Influence Stem Cell Fate. Biomacromolecules 2020, 21, 1968–1994. [Google Scholar] [CrossRef]
- Sugiura, T.; Hibino, N.; Breuer, C.K.; Shinoka, T. Tissue-engineered cardiac patch seeded with human induced pluripotent stem cell derived cardiomyocytes promoted the regeneration of host cardiomyocytes in a rat model. J. Cardiothorac. Surg. 2016, 11, 163. [Google Scholar] [CrossRef]
- Matsuzaki, Y.; Miyamoto, S.; Miyachi, H.; Sugiura, T.; Reinhardt, J.W.; Yu-Chun, C.; Zbinden, J.; Breuer, C.K.; Shinoka, T. The evaluation of a tissue-engineered cardiac patch seeded with hips derived cardiac progenitor cells in a rat left ventricular model. PLoS ONE 2020, 15, e0234087. [Google Scholar] [CrossRef]
- Czosseck, A.; Chen, M.M.; Nguyen, H.; Meeson, A.; Hsu, C.C.; Chen, C.C.; George, T.A.; Ruan, S.C.; Cheng, Y.Y.; Lin, P.J.; et al. Porous scaffold for mesenchymal cell encapsulation and exosome-based therapy of ischemic diseases. J. Control. Release. 2022, 352, 879–892. [Google Scholar] [CrossRef]
- Gaballa, M.A.; Sunkomat, J.N.E.; Thai, H.; Morkin, E.; Ewy, G.; Goldman, S. Grafting an acellular 3-dimensional collagen scaffold onto a non-transmural infarcted myocardium induces neo-angiogenesis and reduces cardiac remodeling. J. Heart Lung Transplant. 2006, 25, 946–954. [Google Scholar] [CrossRef]
- Miyagi, Y.; Chiu, L.L.Y.; Cimini, M.; Weisel, R.D.; Radisic, M.; Li, R. Biodegradable collagen patch with covalently immobilized VEGF for myocardial repair. Biomaterials 2011, 32, 1280–1290. [Google Scholar] [CrossRef]
- Chi, N.; Yang, M.; Chung, T.; Chou, N.; Wang, S. Cardiac repair using chitosan-hyaluronan/silk fibroin patches in a rat heart model with myocardial infarction. Carbohydr. Polym. 2013, 92, 591–597. [Google Scholar] [CrossRef] [PubMed]
- Yin, Q.; Zhu, P.; Liu, W.; Gao, Z.; Zhao, L.; Wang, C.; Li, S.; Zhu, M.; Zhang, Q.; Zhang, X.; et al. A conductive bioengineered cardiac patch for myocardial infarction treatment by improving tissue electrical integrity. Adv. Healthc. Mater. 2022, 13, e2201856. [Google Scholar] [CrossRef]
- Engelmayr, G.C., Jr.; Cheng, M.; Bettinger, C.J.; Borenstein, J.T.; Langer, R.; Freed, L.E. Accordion-like honeycombs for tissue engineering of cardiac anisotropy. Nat. Mater. 2008, 7, 1003–1010. [Google Scholar] [CrossRef]
- Afewerki, S.; Sheikhi, A.; Kannan, S.; Ahadian, S.; Khademhosseini, A. Gelatin-polysaccharide composite scaffolds for 3D cell culture and tissue engineering: Towards natural therapeutics. Bioeng. Transl. Med. 2018, 4, 96–115. [Google Scholar] [CrossRef] [PubMed]
- Chai, Q.; Jiao, Y.; Yu, X. Hydrogels for Biomedical Applications: Their Characteristics and the Mechanisms behind Them. Gels 2017, 3, 6. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Huang, Y. Rational Design of Smart Hydrogels for Biomedical Applications. Front. Chem. 2021, 8, 615665. [Google Scholar] [CrossRef] [PubMed]
- Pena, B.; Laughter, M.; Jett, S.; Rowland, T.J.; Taylor, M.R.G.; Mestroni, L.; Park, D. Injectable Hydrogels for Cardiac Tissue Engineering. Macromol. Biosci. 2018, 18, e1800079. [Google Scholar] [CrossRef]
- Smith, R.R.; Marban, E.; Marban, L. Enhancing retention and efficacy of cardiosphere-derived cells administered after myocardial infarction using a hyaluronan-gelatin hydrogel. Biomatter 2013, 3, e24490. [Google Scholar] [CrossRef]
- Wang, L.L.; Liu, Y.; Chung, J.J.; Wang, T.; Gaffey, A.C.; Lu, M.; Cavanaugh, C.A.; Zhou, S.; Kanade, R.; Atluri, P.; et al. Local and sustained miRNA delivery from an injectable hydrogel promotes cardiomyocyte proliferation and functional regeneration after ischemic injury. Nat. Biomed. Eng. 2018, 1, 983–992. [Google Scholar] [CrossRef] [Green Version]
| Response | Ideal Pore Size (um or ↑/↓) | Ideal Porosity (Value or ↑/↓) |
|---|---|---|
| Macrophage polarization | M1: <20 or >60 (at surface), 34 (intrapore) M2: 30–50 (at surface), >360 | M1: ↓ M2: ↑ |
| Angiogenesis | >5, ~40 | ↑ |
| Hemocompatibility | <10 to limit platelet activation | ↓to limit platelet activation; <50 mL H2O min−1 cm2 at 120 mmHg to limit leakage with anti-coagulants |
| Calcification | ↑ | ↑; <5000 mL H2O min−1 cm2 at 120 mmHg to prevent inflammation |
| Reduction of fibrous capsule | 30–40 | ↑ |
| Material | Animal Species | Number | Surgery or Intervention | Findings | Reference |
|---|---|---|---|---|---|
| PCL | rat | 15 | infra-renal abdominal aorta interposition with the graft | Rapid endothelialization, good patency and mechanical properties, insufficient regeneration of the vascular wall on the long term. | [81] |
| PU/PCL | rabbit | 7 | Carotid artery replacement. | Good anti-thrombosis, host cell infiltration, neotissue formation in 5 months. | [60] |
| PLA/PCL and PGA or PLLA | human | 1 | pulmonary artery recontruction | No evidence of graft occlusion or aneurysmal changes in 7 months. | [82] |
| Slik fibroin | dog | 5 | Carotid srtery replacement. | One of the implanted graft showed the pstency more than a year. Development of elastic fiber and reendothelialization. | [68] |
| PCL with decellularized Rat aorta | rat | 6 | infra-renal abdominal aorta interposition with the graft | Reduced neointimal hyperplasia. Progressed reendothelialization at 12 weeks. | [83] |
| Study Phase | Target Disease, or Situations | Scaffold | Original Estimated Enrollment | Outcome Measurement | Follow Up | Status |
|---|---|---|---|---|---|---|
| 1 | Single ventricle cardiac anatomy | synthetic polymer | 4 | Primary: Graft failure requiring intervention Second: Graft growth | 3 years | completed |
| 2 | Vascular conduits for extracardiac total cavopulmonary connections | synthetic polymer | 24 | Primary: Safety and tolerability Secondary: Efficacy of TEVG determined by MRI | 2 years | recruiting |
| 1 | Chronic venous insufficiency | ECM | 15 | Primary: Thrombosis, infection, surgical complications Secondary: symptoms of target disease, QOL, Graft durability, Flow abnormality, wall degeneration | 1 year | recruiting |
| N/A | peripheral arterial disease | Collagen | 20 | Primary: Graft safety and adverse events Secondary: immunoreaction, graft patency, effect to symptoms a d anke-brachial index | 2 years | Active, not recruiting |
| 1 | Hemodialysis access | Collagen | 20 | Primary: graft patency, intervention and adverse evemts Secondary: immunoreaction, patency and interventions | 6 months | completed |
| N/A | Hemodialysis access | Collagen | 40 | Primary: Safety, tolerability and patency rate Secondary: | 57 weeks | Active, not recruiting |
| N/A | Hemodialysis access | synthetic polymer | 110 | Primary: patency rate, freedom from device-related adverse events Secondary: implantation success rate, patency, interventions, infection | 6 months | Recruiting |
| N/A | Hemodialysis access | synthetic polymer | 20 | Primary: device-related adverse events, patency Secondary: patency, adverse events | 5 years | Active, not recruiting |
| N/A | Coronary artery bypass graft | synthetic polymer | 15 | Primary: Procedural success, device-related serious adverse events Secondary: intimal hyperplasia, patency, Major adverse events, mortality | 5 years | Enrolling by invitation |
| Material | Animal Species | Number | Surgery or Intervention | Findings | Reference |
|---|---|---|---|---|---|
| Upy-polyester-urethanes | Sheep | 33 | Transcatheter AVR | Good hemodynamics with acceptable degree of valve regurgitation | [99] |
| Upy-polyester-urethanes | Sheep | 20 | Surgical PVR | Durable hemodynamics, no stenosis or severe regurgitation | [97] |
| Upy-polyester-urethanes | Sheep | 18 | Surgical PVR | Neointima formation was observed, inflamation was peaked at 6 month while degradation peaked at 12 month. | [101] |
| Bisurea polycarbonate | Sheep | 10 | Surgical PVR | Remodeling with collagen and elastin synthesis, incomplete scaffold resorption in 12 months | [96] |
| Polycarbonate urethane urea and AZ31 magnesium alloy stent | Pig | 5 | Surgical PVR | Normal leaflet function in acute phase, no thrombosis or regurgitation | [100] |
| P4HB-gelatin | Sheep | 4 | Transcatheter PVR | Good hemodynamics, competence after implantation | [98] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Watanabe, T.; Sassi, S.; Ulziibayar, A.; Hama, R.; Kitsuka, T.; Shinoka, T. The Application of Porous Scaffolds for Cardiovascular Tissues. Bioengineering 2023, 10, 236. https://doi.org/10.3390/bioengineering10020236
Watanabe T, Sassi S, Ulziibayar A, Hama R, Kitsuka T, Shinoka T. The Application of Porous Scaffolds for Cardiovascular Tissues. Bioengineering. 2023; 10(2):236. https://doi.org/10.3390/bioengineering10020236
Chicago/Turabian StyleWatanabe, Tatsuya, Salha Sassi, Anudari Ulziibayar, Rikako Hama, Takahiro Kitsuka, and Toshiharu Shinoka. 2023. "The Application of Porous Scaffolds for Cardiovascular Tissues" Bioengineering 10, no. 2: 236. https://doi.org/10.3390/bioengineering10020236





