Changes in Parent Psychological Flexibility after a One-Time Mindfulness-Based Intervention for Parents of Adolescents with Persistent Pain Conditions
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Participant Recruitment Procedure
2.3. Intervention
2.4. Data Collection
2.4.1. Demographic Information
2.4.2. Mindful Attention Awareness Scale (MAAS)
2.4.3. Parent Psychological Flexibility Questionnaire (PPFQ)
2.4.4. Post Session Questionnaire
2.5. Data Analysis
2.5.1. Descriptive Analyses
2.5.2. Quantitative Analyses
2.5.3. Qualitative Analyses
3. Results
3.1. Demographics
3.2. Primary Outcomes
3.2.1. Recruitment and Retention (Feasibility)
3.2.2. Treatment Acceptability
3.3. Secondary Outcomes
3.3.1. Mindfulness
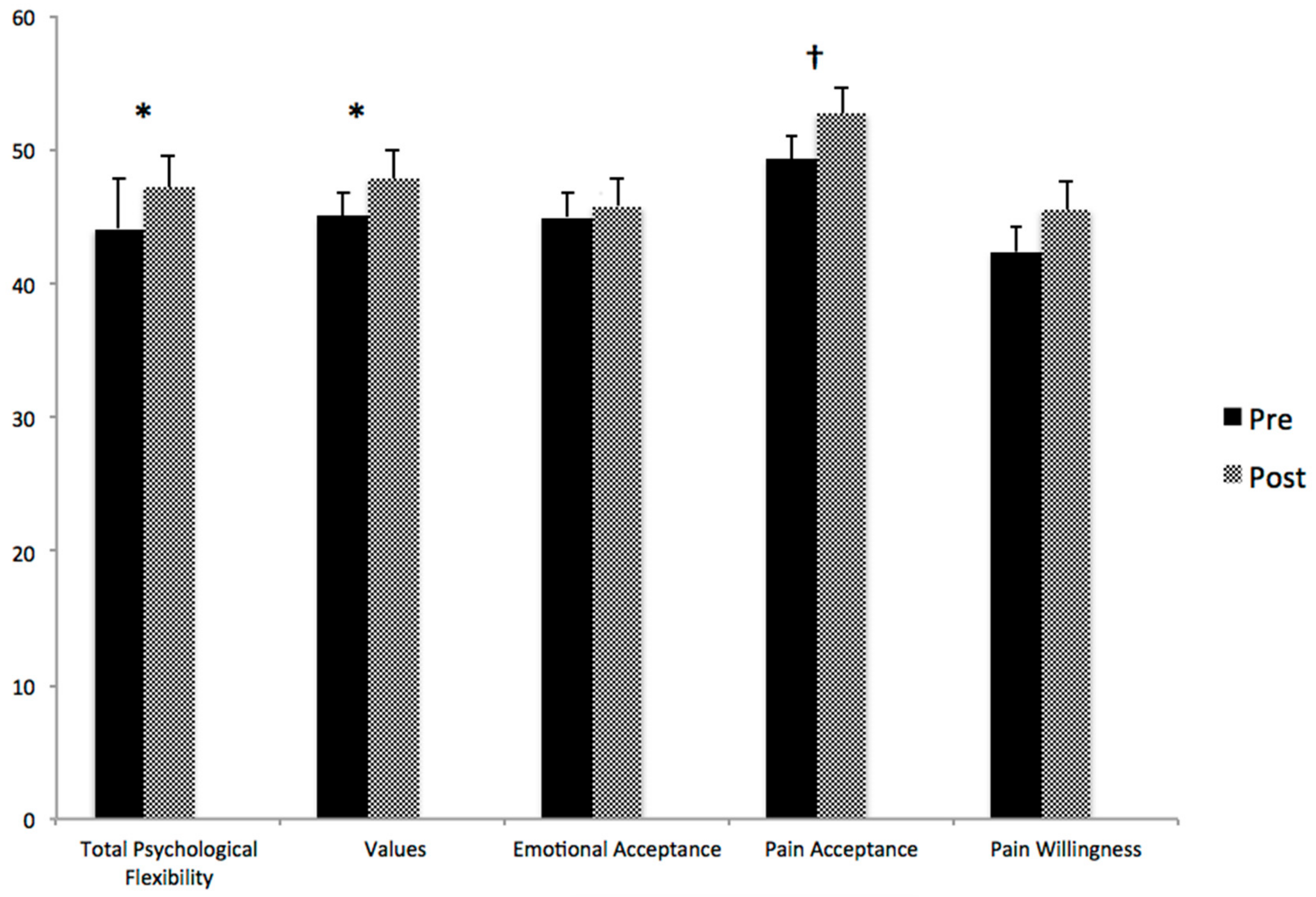
3.3.2. Psychological Flexibility
3.3.3. Post Hoc Exploratory Analyses
3.4. Qualitative Analysis (Post-Session Questionnaire)
3.4.1. Mindfulness Skills
3.4.2. Not Alone
3.4.3. Psychological Flexibility
3.4.4. Parent–Child Interactions
3.4.5. Self-Efficacy
3.4.6. Optimism/Positivity/Hope
3.4.7. Awareness of Values
4. Discussion
4.1. Limitations
4.2. Future Directions
Author Contributions
Funding
Conflicts of Interest
References
- Fisher, E.; Law, E.; Palermo, T.M.; Eccleston, C. Psychological therapies (remotely delivered) for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst. Rev. 2015, 3, CD011118. [Google Scholar] [CrossRef] [PubMed]
- Eccleston, C.; Crombez, G.; Scotford, A.; Clinch, J.; Connell, H. Adolescent chronic pain: Patterns and predictors of emotional distress in adolescents with chronic pain and their parents. Pain 2004, 108, 221–229. [Google Scholar] [CrossRef] [PubMed]
- King, S.; Chambers, C.T.; Huguet, A.; MacNevin, R.C.; McGrath, P.J.; Parker, L.; MacDonald, A.J. The epidemiology of chronic pain in children and adolescents revisited: A systematic review. Pain 2011, 152, 2729–2738. [Google Scholar] [CrossRef] [PubMed]
- Huguet, A.; Miró, J. The severity of chronic pediatric pain: An epidemiological study. J. Pain 2008, 9, 226–236. [Google Scholar] [CrossRef] [PubMed]
- Kamper, S.J.; Henschke, N.; Hestbaek, L.; Dunn, K.M.; Williams, C.M. Musculoskeletal pain in children and adolescents. Braz. J. Phys. Ther. 2016. [Google Scholar] [CrossRef] [PubMed]
- Tracey, I.; Bushnell, M.C. How neuroimaging studies have challenged us to rethink: Is chronic pain a disease? J. Pain 2009, 10, 1113–1120. [Google Scholar] [CrossRef] [PubMed]
- Palermo, T.M. Impact of recurrent and chronic pain on child and family daily functioning: A critical review of the literature. J. Dev. Behav. Pediatr. 2000, 21, 58–69. [Google Scholar] [CrossRef] [PubMed]
- Jordan, A.L.; Eccleston, C.; Osborn, M. Being a parent of the adolescent with complex chronic pain: An interpretative phenomenological analysis. Eur. J. Pain 2007, 11, 49–49. [Google Scholar] [CrossRef] [PubMed]
- Palermo, T.M.; Eccleston, C. Parents of children and adolescents with chronic pain. Pain 2009, 146, 15. [Google Scholar] [CrossRef] [PubMed]
- Ruskin, D.A.; Gagnon, M.M.; Kohut, S.A.; Stinson, J.N.; Walker, K.S. A mindfulness program adapted for adolescents with chronic pain: Feasibility, acceptability, and initial outcomes. Clin. J. Pain 2017, 33, 1019–1029. [Google Scholar] [CrossRef] [PubMed]
- Ruskin, D.; Harris, L.; Stinson, J.; Kohut, S.A.; Walker, K.; McCarthy, E. “I Learned to Let Go of My Pain”. The Effects of Mindfulness Meditation on Adolescents with Chronic Pain: An Analysis of Participants’ Treatment Experience. Children 2017, 4, 110. [Google Scholar] [CrossRef] [PubMed]
- Kabat-Zinn, J. Full Catastrophe Living: How to Cope with Stress, Pain and Illness Using Mindfulness Meditation; Piatkus: London, UK, 1996. [Google Scholar]
- Eccleston, C.; Fisher, E.; Law, E.; Bartlett, J.; Palermo, T.M. Psychological interventions for parents of children and adolescents with chronic illness. Cochrane Database Syst. Rev. 2015, 4, CD009660. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, S.G.; Sawyer, A.T.; Witt, A.A.; Oh, D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. J. Consult. Clin. Psychol. 2010, 78, 169. [Google Scholar] [CrossRef] [PubMed]
- McCracken, L.M.; Gauntlett-Gilbert, J. Role of psychological flexibility in parents of adolescents with chronic pain: Development of a measure and preliminary correlation analyses. Pain 2011, 152, 780–785. [Google Scholar] [CrossRef] [PubMed]
- Wallace, D.P.; McCracken, L.M.; Weiss, K.E.; Harbeck-Weber, C. The role of parent psychological flexibility in relation to adolescent chronic pain: Further instrument development. J. Pain 2015, 16, 235–246. [Google Scholar] [CrossRef] [PubMed]
- Bazzano, A.; Wolfe, C.; Zylowska, L.; Wang, S.; Schuster, E.; Barrett, C.; Lehrer, D. Mindfulness based stress reduction (MBSR) for parents and caregivers of individuals with developmental disabilities: A community-based approach. J. Child Fam. Stud. 2015, 24, 298–308. [Google Scholar] [CrossRef]
- Benn, R.; Akiva, T.; Arel, S.; Roeser, R.W. Mindfulness training effects for parents and educators of children with special needs. Dev. Psychol. 2012, 48, 1476. [Google Scholar] [CrossRef] [PubMed]
- Blackledge, J.T.; Hayes, S.C. Using acceptance and commitment training in the support of parents of children diagnosed with autism. Child Fam. Behav. Ther. 2006, 28, 1–18. [Google Scholar] [CrossRef]
- Dykens, E.M.; Fisher, M.H.; Taylor, J.L.; Lambert, W.; Miodrag, N. Reducing distress in mothers of children with autism and other disabilities: A randomized trial. Pediatrics 2014, 134, e454–e463. [Google Scholar] [CrossRef] [PubMed]
- Ferraioli, S.J.; Harris, S.L. Comparative effects of mindfulness and skills-based parent training programs for parents of children with autism: Feasibility and preliminary outcome data. Mindfulness 2013, 4, 89–101. [Google Scholar] [CrossRef]
- Lunsky, Y.; Hastings, R.P.; Weiss, J.A.; Palucka, A.M.; Hutton, S.; White, K. Comparative effects of mindfulness and support and information group interventions for parents of adults with autism spectrum disorder and other developmental disabilities. J. Autism Dev. Disord. 2017, 47, 1769–1779. [Google Scholar] [CrossRef] [PubMed]
- Lunsky, Y.; Robinson, S.; Reid, M.; Palucka, A. Development of a mindfulness-based coping with stress group for parents of adolescents and adults with developmental disabilities. Mindfulness 2015, 6, 1335–1344. [Google Scholar] [CrossRef]
- Neece, C.L. Mindfulness-based stress reduction for parents of young children with developmental delays: Implications for parental mental health and child behavior problems. J. Appl. Res. Intellect. Disabil. 2014, 27, 174–186. [Google Scholar] [CrossRef] [PubMed]
- Singh, N.N.; Lancioni, G.E.; Winton, A.S.; Fisher, B.C.; Wahler, R.G.; Mcaleavey, K.; Sabaawi, M. Mindful parenting decreases aggression, noncompliance, and self-injury in children with autism. J. Emot. Behav. Disord. 2006, 14, 169–177. [Google Scholar] [CrossRef]
- Singh, N.N.; Lancioni, G.E.; Winton, A.S.; Karazsia, B.T.; Myers, R.E.; Latham, L.L.; Singh, J. Mindfulness-based positive behavior support (MBPBS) for mothers of adolescents with autism spectrum disorder: Effects on adolescents’ behavior and parental stress. Mindfulness 2014, 5, 646–657. [Google Scholar] [CrossRef]
- Singh, N.N.; Lancioni, G.E.; Winton, A.S.; Singh, J.; Curtis, W.J.; Wahler, R.G.; McAleavey, K.M. Mindful parenting decreases aggression and increases social behavior in children with developmental disabilities. Behav. Modif. 2007, 31, 749–771. [Google Scholar] [CrossRef] [PubMed]
- Geurtzen, N.; Scholte, R.H.; Engels, R.C.; Tak, Y.R.; van Zundert, R.M. Association between mindful parenting and adolescents’ internalizing problems: Non-judgmental acceptance of parenting as core element. J. Child Fam. Stud. 2015, 24, 1117–1128. [Google Scholar] [CrossRef]
- Parent, J.; Garai, E.; Forehand, R.; Roland, E.; Potts, J.; Haker, K.; Compas, B.E. Parent mindfulness and child outcome: The roles of parent depressive symptoms and parenting. Mindfulness 2010, 1, 254–264. [Google Scholar] [CrossRef] [PubMed]
- Bögels, S.; Hoogstad, B.; van Dun, L.; de Schutter, S.; Restifo, K. Mindfulness training for adolescents with externalizing disorders and their parents. Behav. Cogn. Psychother. 2008, 36, 193–209. [Google Scholar] [CrossRef]
- Dumas, J.E. Mindfulness-based parent training: Strategies to lessen the grip of automaticity in families with disruptive children. J. Clin. Child Adolesc. Psychol. 2005, 34, 779–791. [Google Scholar] [CrossRef] [PubMed]
- Singh, N.N.; Singh, A.N.; Lancioni, G.E.; Singh, J.; Winton, A.S.; Adkins, A.D. Mindfulness training for parents and their children with ADHD increases the children’s compliance. J. Child Fam. Stud. 2010, 19, 157–166. [Google Scholar] [CrossRef]
- Srivastava, M.; Gupta, A.; Talukdar, U.; Kalra, B.P.; Lahan, V. Effect of parental training in managing the behavioral problems of early childhood. Indian J. Pediatr. 2011, 78, 973–978. [Google Scholar] [CrossRef] [PubMed]
- Van der Oord, S.; Bögels, S.M.; Peijnenburg, D. The effectiveness of mindfulness training for children with ADHD and mindful parenting for their parents. J. Child Fam. Stud. 2012, 21, 139–147. [Google Scholar] [CrossRef] [PubMed]
- Van de Weijer-Bergsma, E.; Formsma, A.R.; de Bruin, E.I.; Bögels, S.M. The effectiveness of mindfulness training on behavioral problems and attentional functioning in adolescents with ADHD. J. Child Fam. Stud. 2012, 21, 775–787. [Google Scholar] [CrossRef] [PubMed]
- Bögels, S.M.; Hellemans, J.; van Deursen, S.; Römer, M.; van der Meulen, R. Mindful parenting in mental health care: Effects on parental and child psychopathology, parental stress, parenting, coparenting, and marital functioning. Mindfulness 2014, 5, 536–551. [Google Scholar] [CrossRef]
- Parent, J.; McKee, L.G.; Rough, J.N.; Forehand, R. The association of parent mindfulness with parenting and youth psychopathology across three developmental stages. J. Abnorm. Child Psychol. 2016, 44, 191–202. [Google Scholar] [CrossRef] [PubMed]
- Altmaier, E.; Maloney, R. An initial evaluation of a mindful parenting program. J. Clin. Psychol. 2007, 63, 1231–1238. [Google Scholar] [CrossRef] [PubMed]
- Minor, H.G.; Carlson, L.E.; Mackenzie, M.J.; Zernicke, K.; Jones, L. Evaluation of a mindfulness-based stress reduction (MBSR) program for caregivers of children with chronic conditions. Soc. Work. Health Care 2006, 43, 91–109. [Google Scholar] [CrossRef] [PubMed]
- Brown, K.W.; Ryan, R.M. The benefits of being present: Mindfulness and its role in psychological well-being. J. Pers. Soc. Psychol. 2003, 84, 822. [Google Scholar] [CrossRef] [PubMed]
- Wallace, D.P.; Woodford, B.; Connelly, M. Promoting psychological flexibility in parents of adolescents with chronic pain: Pilot study of an 8-week group intervention. Clin. Pr. Pediatr. Psychol. 2016, 4, 405. [Google Scholar] [CrossRef]
- Esteve, R.; Ramírez-Maestre, C. Pain fear avoidance and pain acceptance: A cross-sectional study comparing their influence on adjustment to chronic pain across three samples of patients. Ann. Behav. Med. 2013, 46, 169–180. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Informatics 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Turner, D.; Otley, A.R.; Mack, D.; Hyams, J.; De Bruijne, J.; Uusoue, K.; Steinhart, A.H. Development, validation, and evaluation of a pediatric ulcerative colitis activity index: A prospective multicenter study. Gastroenterology 2007, 133, 423–432. [Google Scholar] [CrossRef] [PubMed]
- Turner, D.; Griffiths, A.M.; Walters, T.D.; Seah, T.; Markowitz, J.; Pfefferkorn, M.; Hyams, J. Appraisal of the pediatric Crohn’s disease activity index on four prospectively collected datasets: Recommended cutoff values and clinimetric properties. Am. J. Gastroenterol. 2010, 105, 2085. [Google Scholar] [CrossRef] [PubMed]
- Elo, S.; Kyngäs, H. The qualitative content analysis process. J. Adv. Nurs. 2008, 62, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Sandelowski, M. What’s in a name? Qualitative description revisited. Res. Nurs. Health 2010, 33, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Lustria, M.L.A.; Noar, S.M.; Cortese, J.; Van Stee, S.K.; Glueckauf, R.L.; Lee, J. A meta-analysis of web-delivered tailored health behavior change interventions. J. Health Commun. 2013, 18, 1039–1069. [Google Scholar] [CrossRef] [PubMed]
- Brassell, A.A.; Rosenberg, E.; Parent, J.; Rough, J.N.; Fondacaro, K.; Seehuus, M. Parent’s psychological flexibility: Associations with parenting and child psychosocial well-being. J. Context. Behav. Sci. 2016, 5, 111–120. [Google Scholar] [CrossRef]
- Moyer, D.N.; Sandoz, E.K. The role of psychological flexibility in the relationship between parent and adolescent distress. J. Child Fam. Stud. 2015, 24, 1406–1418. [Google Scholar] [CrossRef]
- Carmody, J.; Baer, R.A. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. J. Behav. Med. 2008, 31, 23–33. [Google Scholar] [CrossRef] [PubMed]
- Huppert, F.A.; Johnson, D.M. A controlled trial of mindfulness training in schools: The importance of practice for an impact on well-being. J. Posit. Psychol. 2010, 5, 264–274. [Google Scholar] [CrossRef]
- Ribeiro, L.; Atchley, R.M.; Oken, B.S. Adherence to practice of mindfulness in novice meditators: Practices chosen, amount of time practiced, and long-term effects following a mindfulness-based intervention. Mindfulness 2018, 9, 401–411. [Google Scholar] [CrossRef]
- Rolland, J.S. Chronic illness and the life cycle: A conceptual framework. Fam. Process. 1987, 26, 203–221. [Google Scholar] [CrossRef] [PubMed]
- Walker, L.S.; Sherman, A.L.; Bruehl, S.; Garber, J.; Smith, C.A. Functional abdominal pain patient subtypes in childhood predict functional gastrointestinal disorders with chronic pain and psychiatric comorbidities in adolescence and adulthood. Pain 2012, 153, 1798–1806. [Google Scholar] [CrossRef] [PubMed]
- Parsons, C.E.; Crane, C.; Parsons, L.J.; Fjorback, L.O.; Kuyken, W. Home practice in Mindfulness-Based Cognitive Therapy and Mindfulness-Based Stress Reduction: A systematic review and meta-analysis of participants’ mindfulness practice and its association with outcomes. Behav. Res. Ther. 2017, 95, 29–41. [Google Scholar] [CrossRef] [PubMed]
- Veehof, M.M.; Trompetter, H.R.; Bohlmeijer, E.T.; Schreurs, K.M.G. Acceptance-and mindfulness-based interventions for the treatment of chronic pain: A meta-analytic review. Cogn. Behav. Ther. 2016, 45, 5–31. [Google Scholar] [CrossRef] [PubMed]

| Schedule | Content |
|---|---|
| 5 min | Name tags, tea/coffee, and snacks |
| 10 min | Welcome and Introduction to Mindfulness |
| Teaching: What is mindfulness? | |
| Presentation of Jon Kabat Zinn’s definition of mindfulness (Kabat-Zinn, 1996) | |
| Mindfulness gives us flexibility/choice in how we respond to situations in our lives (our children, our colleagues, our partners, our own internal experiences). | |
| 20 min | Ice Breaker and Group Guidelines |
| Activity 1: Participants divide into dyads and are encouraged to pair up with someone unfamiliar. They are asked to introduce themselves to their partner and share elements in their lives that bring them joy. They are instructed to do so mindfully. The person speaking is asked to mindfully be aware of any sensations, emotions, thoughts, and/or judgments while they speak, and the listener is instructed to mindfully listen to their partner and be aware of any thoughts, emotions, sensations, or judgments that might take them away from mindful listening. After 4 min, participants are asked to switch roles and then introduce their partner to the group. The exercise is then processed by asking participants what they noticed during the activity and relating their observations back to mindfulness concepts (e.g., nonjudgment, present moment awareness, monkey mind, beginners mind). | |
| Review of group guidelines: (1) confidentiality, (2) respectful attitude | |
| The talking stick is introduced. When a participant is holding the talking stick, it is an invitation for them to speak from the heart and for others to give the speaker their full attention. | |
| Activity 2: | |
| Teaching: Suffering is optional (it is the distress, whether emotional or cognitive, associated with the pain that leads to a significant proportion of suffering) | |
| Exercises: Suffering Cup (participants add water to the cup to reflect the amount of space taken up by each of the following in their day-to-day lives: their child’s day-to-day physical symptoms, the parent’s own thoughts about their child’s symptoms, the parent’s own emotions about their child’s symptoms, the impact on the parent’s wellness of their child’s symptoms. Not only does their child’s actual symptoms lead to suffering, but a parent’s emotions and thoughts add to suffering, and are optional). | |
| 30 min | Meditation: Mindful Awareness Meditation |
| Participants are taken through a mindful awareness practice of being aware of the quality of their thoughts, emotions, physical sensations, and sounds in the room, and approaching these with nonjudgmental curiosity and openness. | |
| 30 min | Parenting According to Your Values |
| Teaching: Our values are a compass to guide interactions with our children. Mindfulness practice can help us connect with our values during difficult parenting situations. | |
| Parents are provided with a list of values and identify their top three values that guide their parenting. | |
| Parents were then asked to reflect on a situation where (a) they followed their values as a parent, and (b) they did not follow their values as a parent. In each situation, they notice their experience (their thoughts, emotions, and judgments). | |
| Responding versus Reacting | |
| Teaching: Responding versus reacting to strong sensations, emotions, or thoughts | |
| 15 min | How to bring mindfulness into your life |
| Informal versus formal meditation practices | |
| List of local mindfulness resources and books/apps provided | |
| Home practice: To practice informal mindfulness | |
| 15 min | Stone ceremony |
| Participants provide a good wish to one another, in turn. |
| Characteristic | Full Sample | Chronic Pain | IBD |
|---|---|---|---|
| (n = 34 Parents) | (n = 14 Parents) | (n = 20 Parents) | |
| Parent gender, n (%) | |||
| Female | 27 (79%) | 11 (79%) | 16 (80%) |
| Male | 7 (21%) | 3 (21%) | 4 (20%) |
| Adolescent age (years, mean SD) | 14.9 ± 1.5 | 15.5 ± 1.6 | 14.2 ± 1.2 * |
| Adolescent gender, n (%) | |||
| Female | 23 (68%) | 14 (100%) | 9 (45%) |
| Male | 11 (32%) | 0 (0%) | 11 (55%) * |
| Primary diagnosis for adolescent, n (%) | Musculoskeletal: 7 (50%) | Ulcerative colitis: 7 (41%) | |
| Neuropathic: 2 (14%) | |||
| Musculoskeletal + Neuropathic: 3 (21%) | Crohn’s disease: 10 (59%) | ||
| Other 1: 2 (14%) | |||
| Chronic pain: Adolescent’s duration of pain (months, mean SD) | 59.7 ± 57.8 | ||
| IBD: Adolescent disease activity 2 | 13.1 ± 11.8 |
| Theme | Parents (N = 32) | Subthemes | Exemplar Quotes |
|---|---|---|---|
| Mindfulness Skills | 29 (91%) | Present-Moment Awareness | “Trying to be more present and not just making it through the day” (Participant, IBD Group) |
| Compassion | “I need to learn how to take care of myself so I can look after my child” (Participant, Chronic Pain Group) | ||
| Acceptance | “The pain will stay, but we need to work collectively to develop and maintain coping strategies and work with our daughter to achieve some level of normalcy” (Participant, Chronic Pain Group) | ||
| Secondary Suffering | “Understanding the potential for how much of my thinking can be consumed by worry for my child” (Participant, IBD Group) | ||
| Importance of Regular Practice | “Strive to do mindfulness (MBSR) each day; to incorporate it into my daily routine” (Participant, IBD Group) | ||
| Not Alone | 19 (59%) | Sense of Community/Shared Experience | “We aren’t alone—many people/families are dealing with pain issues, and that there are people and resources available to help” (Participant, Chronic Pain Group) |
| Connection | “Parent sharing was very helpful” (Participant, IBD Group) | ||
| Psychological Flexibility | 11 (34%) | Emotion Regulation | “The STOP method of responding—it’s a good quick way to remind myself to take a step back from a knee-jerk response when I’m on edge” (Participant, Chronic Pain Group) |
| Perspective Taking | “Good experience to listen to other parents comments and struggles. Gain different perspectives and ideas” (Participant, IBD Group) | ||
| Parent–Child Interactions | 8 (25%) | N/A | “Understanding how my actions can impact my daughter’s health” (Participant, IBD Group) |
| Self-Efficacy | 7 (22%) | N/A | “I am not doing a bad job” (Participant, IBD Group) |
| Optimism/Positivity/Hope | 6 (19%) | N/A | “There are people and resources available to help” (Participant, Chronic Pain Group) |
| Awareness of Values | 5 (16%) | N/A | “To take the time to really realize what is important in the moment” (Participant, IBD Group) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ruskin, D.; Campbell, L.; Stinson, J.; Ahola Kohut, S. Changes in Parent Psychological Flexibility after a One-Time Mindfulness-Based Intervention for Parents of Adolescents with Persistent Pain Conditions. Children 2018, 5, 121. https://doi.org/10.3390/children5090121
Ruskin D, Campbell L, Stinson J, Ahola Kohut S. Changes in Parent Psychological Flexibility after a One-Time Mindfulness-Based Intervention for Parents of Adolescents with Persistent Pain Conditions. Children. 2018; 5(9):121. https://doi.org/10.3390/children5090121
Chicago/Turabian StyleRuskin, Danielle, Lauren Campbell, Jennifer Stinson, and Sara Ahola Kohut. 2018. "Changes in Parent Psychological Flexibility after a One-Time Mindfulness-Based Intervention for Parents of Adolescents with Persistent Pain Conditions" Children 5, no. 9: 121. https://doi.org/10.3390/children5090121
APA StyleRuskin, D., Campbell, L., Stinson, J., & Ahola Kohut, S. (2018). Changes in Parent Psychological Flexibility after a One-Time Mindfulness-Based Intervention for Parents of Adolescents with Persistent Pain Conditions. Children, 5(9), 121. https://doi.org/10.3390/children5090121





