Reflux Incidence among Exclusively Breast Milk Fed Infants: Differences of Feeding at Breast versus Pumped Milk
Abstract
:1. Introduction
2. Materials and Methods
2.1. Population
2.2. Data Collection
2.3. Outcome Assessment
2.4. Exposure Assessment
2.5. Analysis
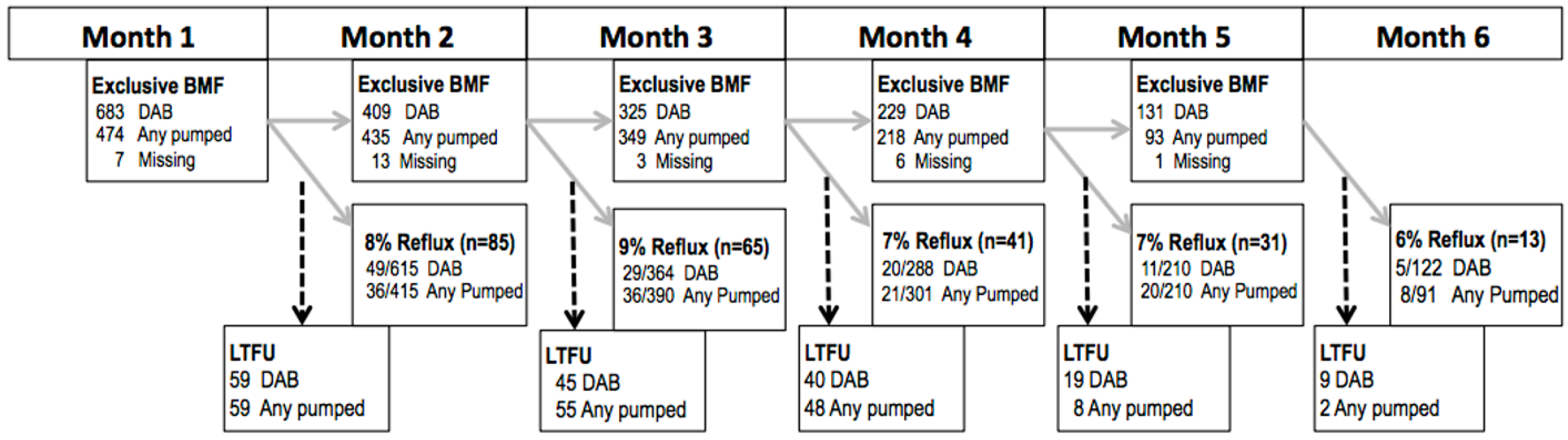
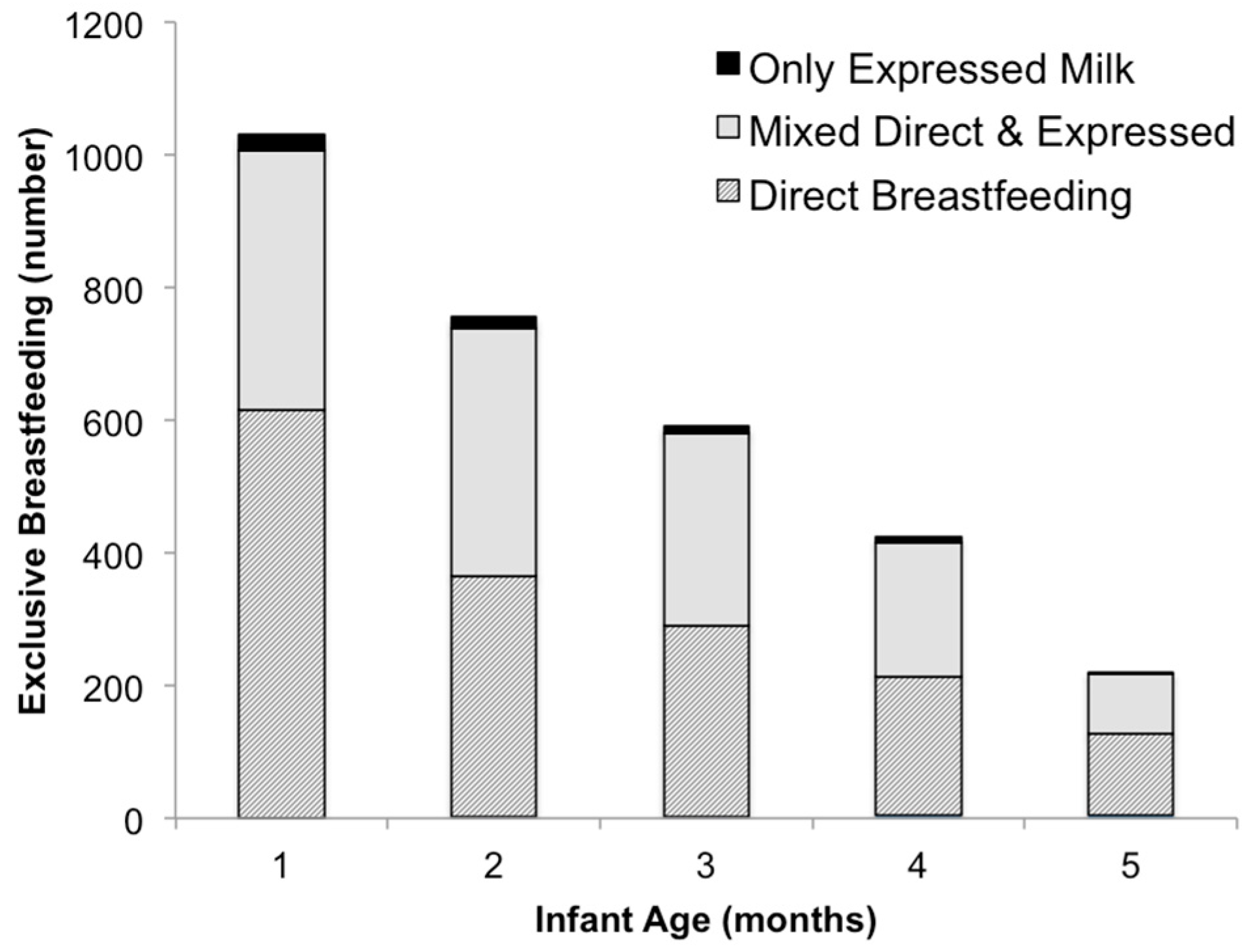
3. Results
4. Discussion
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Dogra, H.; Lad, B.; Sirisena, D. Paediatric gastro-oesophageal reflux disease. Gastroenterol. Clin. N. Am. 1990, 19, 617–629. [Google Scholar]
- Hegar, B.; Dewanti, N.R.; Kadim, M.; Alatas, S.; Firmansyah, A.; Vandenplas, Y. Natural evolution of regurgitation in healthy infants. Acta Paediatr. 2009, 98, 1189–1193. [Google Scholar] [CrossRef] [PubMed]
- Orenstein, S.; Shalaby, T.; Cohn, J. Reflux symptoms in 100 normal infants: Diagnositic validity of the Infant Gastroesophageal Reflux Questionnaire. Clin. Pediatr. 1996, 35, 607–614. [Google Scholar] [CrossRef]
- Heacock, H.; Jeffery, H.; Baker, J.; Page, M. Influence of breast versus formula milk on physiological gastroesophageal reflux in healthy, newborn infants. J. Pediatr. Gastroenterol. Nutr. 1992, 14, 41–46. [Google Scholar] [CrossRef] [PubMed]
- WHO. Exclusive Breastfeeding for Six Months Best for Babies Everywhere; WHO: Geneva, Switzerland, 2011. [Google Scholar]
- American Academy of Pediatrics Section on Breastfeeding Medicine. Breastfeeding and the use of human milk. Pediatrics 2012, 129, e827. [Google Scholar]
- American Academy of Pediatrics Section on Breastfeeding Medicine. Breastfeeding and the use of human milk. Pediatrics 2005, 115, 496–506. [Google Scholar]
- Institute of Medicine, Committee on Nutritional Status during Pregnancy and Lactation. Nutrition during Lactation; National Academy Press: Washington, DC, USA, 1991; pp. 166–175; 179–180; 198–200.
- Mohrbacher, N. The Breastfeeding Answer Book; La Leche League International: Schaumburg, IL, USA, 2005. [Google Scholar]
- Ip, S.; Chung, M.; Raman, G.; Chew, P.; Magula, N.; DeVine, D.; Trikalinos, T.; Lau, J. Agency for Healthcare Research and Quality. In Breastfeeding and Maternal and Infant Health Outcomes in Developed Countries; Evidence Report/Technology Assessment No. 153 (Prepared by Tufts-New England Medical Center Evidence-based Practice Center, under Contract No. 290-02-0022); AHRQ Publication No. 07-E007; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2007. [Google Scholar]
- U.S. Department of Health and Human Services. The Surgeon General’s Call to Action to Support Breastfeeding; U.S. Department of Health and Human Services, Office of the Surgeon General: Washington, DC, USA, 2011.
- Dermer, A. A well-kept secret: Breastfeeding’s benefits to mothers. New Begin. 2001, 18, 124–127. [Google Scholar]
- Bachrach, V.R.; Schwarz, E.; Bachrach, L.R. Breastfeeding and the risk of hospitalization for respiratory disease in infancy: A meta-analysis. Arch. Pediatr. Adolesc. Med. 2003, 157, 237–243. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, R.; Lawrence, R. Breastfeeding: A Guide for the Medical Profession; Mosby: St. Louis, MO, USA, 1999. [Google Scholar]
- Ladomenou, F.; Moschandreas, J.; Kafatos, A.; Tselentis, Y.; Galanikis, E. Protective effect of exclusive breastfeeding against infections during infancy: A prospective study. Arch. Dis. Child 2010, 95, 1004–1008. [Google Scholar] [CrossRef] [PubMed]
- McNiel, M.E.; Labbok, M.H.; Abrahams, S.W. What are the risks associated with formula feeding? A re-analysis and review. Birth 2010, 37, 50–58. [Google Scholar] [CrossRef] [PubMed]
- Victora, C.G.; Bahol, R.; Barros, A.; Franca, G.V.A.; Horton, S.; Krasevec, J.; Murch, S.; Sandar, M.J.; Walker, N.; Rollins, N. Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet 2016, 387, 475–490. [Google Scholar] [CrossRef]
- Weimer, J. The Economic Benefits of Breast Feeding: A Review and Analysis; Food Assistance and Nutrition Research Report No. 13; Food and Rural Economics Division, Economic Research Service, US Department of Agriculture: Washington, DC, USA, 2001.
- Ball, T.M.; Wright, A.L. Health care cost of formula-feeding in the first year of life. Pediatrics 1999, 103, 870–887. [Google Scholar] [PubMed]
- Bartick, M.; Stuebe, A.; Schwarz, E.; Luongo, C.; Reinhold, A.; Foster, E. Cost analysis of maternal disease associated with suboptimal breastfeeding. Obstet. Gynecol. 2013, 122, 111–119. [Google Scholar] [CrossRef] [PubMed]
- Tuttle, C.R.; Dewey, K.G. Potential cost savings for Medi-Cal, AFDC, food stamps, and WIC programs associated with increasing breast-feeding among low-income Hmong women in California. J. Am. Diet. Assoc. 1996, 96, 885–890. [Google Scholar] [CrossRef]
- Cohen, R.; Mrtek, M.B.; Mrtek, R.G. Comparison of maternal absenteeism and infant illness rates among breast-feeding and formula-feeding women in two corporations. Am. J. Health Promot. 1995, 10, 148–153. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Breastfeeding Data. 2015. Available online: http://www.cdc.gov/breastfeeding/data/nis_data/ (accessed on 29 June 2016). [Google Scholar]
- Johns, H.; Forster, D.; Amir, L.; McLachlan, H. Prevalence and outcomes in breast milk expressing in women with healthy term infants: A systematic review. BMC Pregnancy Childbirth 2013, 13, 212. [Google Scholar] [CrossRef] [PubMed]
- Labiner-Wolfe, J.; Fein, S.; Shealy, K.; Wang, C. Prevalence of breast milk expression and associated factors. Pediatrics 2008, 122 (Suppl. 2), S63–S68. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Pediatrics. Federal Support for Breastfeeding; American Academy of Pediatrics: Elk Grove Village, IL, USA, 2013; Available online: http://www2.aap.org/breastfeeding/files/pdf/FederalSupportforBreastfeedingResource.pdf (accessed on 29 June 2016).
- Odom, E.; Li, R.; Scanlon, K.; Perrine, C.; Grummer-Strawn, L. Reasons for earlier than desired cessation of breastfeeding. Pediatrics 2013, 131, e726–e732. [Google Scholar] [CrossRef] [PubMed]
- Ghoshal, B.; Lahiri, S.; Kar, K.; Sarkar, N. Changes in biochemical contents of expressed breast milk on refrigerator storage. Indian Pediatr. 2012, 49, 836–837. [Google Scholar] [CrossRef] [PubMed]
- Bertino, E.; Giribaldi, M.; Baro, C.; Giancotti, V.; Pazzi, M.; Peila, C.; Tonetto, P.; Arslanoglu, S.; Moro, G.E.; Cavallarin, L.; et al. Effect of prolonged refrigeration on the lipid profile, lipase activity, and oxidative status of human milk. J. Pediatr. Gastroenterol. Nutr. 2013, 56, 390–396. [Google Scholar] [CrossRef] [PubMed]
- Takci, S.; Gulmez, D.; Yigit, S.; Dogan, O.; Hascelik, G. Container type and bactericidal activity of human milk during refrigerated storage. J. Hum. Lact. 2013, 29, 406–411. [Google Scholar] [CrossRef] [PubMed]
- Silvestre, D.; López, M.C.; March, L.; Plaza, A.; Martínez-Costa, C. Bactericidal activity of human milk: Stability during storage. Br. J. Biomed. Sci. 2006, 63, 59–62. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, R.A. Storage of human milk and the influence of procedures on immunological components of human milk. Acta Paediatr. 1999, 88, 14–18. [Google Scholar] [CrossRef]
- Rasmussen, K.; Geraghty, S. The quiet revolution: Breastfeeding transformed with the use of breast pumps. Am. J. Public Health 2011, 101, 1356–1359. [Google Scholar] [CrossRef] [PubMed]
- Geraghty, S.; Rasmussen, K. Redefining “breastfeeding” initiation and duration in the age of breastmilk pumping. Breastfeeding Med. 2010, 5, 135–137. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Fein, S.; Grummer-Strawn, L. Do infants fed from bottles lack self-regulation of milk intake compared with directly breastfed infants? Pediatrics 2010, 125, e1386–e1393. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Magadia, J.; Fein, S.; Grummer-Strawn, L. Risk of bottle-feeding for rapid weight gain during the first year of life. Arch. Pediatr. Adolesc. Med. 2012, 166, 431–436. [Google Scholar] [PubMed]
- Soto-Ramírez, N.; Karmaus, W.; Zhang, H.; Davis, S.; Agarwal, S.; Albergottie, A. Modes of infant feeding and the occurrence of coughing/wheezing in the first year of life. J. Hum. Lact. 2013, 29, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Woolridge, M.W.; Fisher, C. Colic, “overfeeding,” and symptoms of lactose malabsorption in the breast-fed baby: A possible artifact of feed management? Lancet 1988, 2, 382–384. [Google Scholar] [CrossRef]
- Fein, S.B.; Labiner-Wolfe, J.; Shealy, K.R.; Li, R.; Chen, J.; Grummer-Strawn, L.M. Infant Feeding Practices Study II: Study methods. Pediatrics 2008, 122 (Suppl. 2), S28–S35. [Google Scholar] [CrossRef] [PubMed]
- Greenland, S.; Pearl, J.; Robins, J.M. Causal diagrams for epidemiologic research. Epidemiology 1999, 10, 37–48. [Google Scholar] [CrossRef] [PubMed]
- DiSantis, K.I.; Collins, B.N.; Fisher, J.O.; Davey, A. Do infants fed directly from the breast have improved appetite regulation and slower growth during early childhood compared with infants fed from a bottle? Int. J. Behav. Nutr. Phys. Act. 2011, 8, 89. [Google Scholar] [CrossRef] [PubMed]
- Nelson, S.P.; Chen, E.H.; Syniar, G.M.; Christoffel, K.K. Prevalence of symptoms of gastroesophageal reflux during infancy. Arch. Pediatr. Adolesc. Med. 1997, 151, 569–572. [Google Scholar] [CrossRef] [PubMed]
- Iacono, G.; Merolla, R.; D’Amico, D.; Bonci, E.; Cavataio, F.; Di Prima, L.; Scalicia, C.; Indinnimeoc, L.; Avernad, M.R.; Carrocciod, A. Gastrointestinal symptoms in infancy: A population-based prospective study. Dig. Liver Dis. 2005, 37, 432–438. [Google Scholar] [CrossRef] [PubMed]
- Mathisen, B.; Worrall, L.; Masel, J.; Wall, C.; Shepherd, R.W. Feeding problems in infants with gastro-oesophageal reflux disease: A controlled study. J. Paediatr. Child Health 1999, 35, 163–169. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Labor, Bureau of Labor Statistics. Table 6. Employment Status of Mothers with Own Children under 3 Years Old by Single Year of Age of Youngest Child and Marital Status, 2014–15 Annual Averages. 2016. Available online: http://www.bls.gov/news.release/famee.t06.htm (accessed on 28 June 2016). [Google Scholar]
| Direct Breastfeeding (n = 683) | Any Pumped Milk Feeding (n = 474) | |||
|---|---|---|---|---|
| n | (%) | n | (%) | |
| Maternal Variables | ||||
| Education | ||||
| High School or Less | 91 | (14) | 49 | (11) |
| Some College | 256 | (38) | 150 | (33) |
| College Graduate or more | 318 | (48) | 252 | (56) |
| Primiparous | 121 | (18) | 174 | (37) |
| Race/Ethnicity | ||||
| White, non-Hispanic | 614 | (91) | 400 | (86) |
| Black, non-Hispanic | 6 | (1) | 13 | (3) |
| Hispanic | 25 | (4) | 29 | (6) |
| Other | 27 | (4) | 23 | (5) |
| Cesarean Delivery | 151 | (22) | 127 | (27) |
| Smoking | 17 | (2) | 25 | (5) |
| WIC * | 170 | (25) | 90 | (19) |
| Maternal BMI * (pre-pregnancy) | ||||
| Underweight (<18.5) | 38 | (6) | 9 | (2) |
| Normal (18.5–24.9) | 344 | (50) | 250 | (53) |
| Overweight (>25.0–29.9) | 174 | (25) | 121 | (26) |
| Obese (>30.0) | 122 | (18) | 89 | (19) |
| Infant Variables | ||||
| NICU * Stay | 12 | (1) | 0 | (0) |
| Birthweight | ||||
| <2500 g | 1 | (0) | 3 | (0) |
| 2500–4000 g | 578 | (85) | 421 | (89) |
| >4000 g | 104 | (15) | 50 | (11) |
| Model | Risk Ratio | 95% Confidence Interval |
|---|---|---|
| Crude | 0.87 | 0. 68–1.12 |
| Adjusted ** | 0.88 | 0.69–1.13 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yourkavitch, J.; Zadrozny, S.; Flax, V.L. Reflux Incidence among Exclusively Breast Milk Fed Infants: Differences of Feeding at Breast versus Pumped Milk. Children 2016, 3, 18. https://doi.org/10.3390/children3040018
Yourkavitch J, Zadrozny S, Flax VL. Reflux Incidence among Exclusively Breast Milk Fed Infants: Differences of Feeding at Breast versus Pumped Milk. Children. 2016; 3(4):18. https://doi.org/10.3390/children3040018
Chicago/Turabian StyleYourkavitch, Jennifer, Sabrina Zadrozny, and Valerie L. Flax. 2016. "Reflux Incidence among Exclusively Breast Milk Fed Infants: Differences of Feeding at Breast versus Pumped Milk" Children 3, no. 4: 18. https://doi.org/10.3390/children3040018





