Parental Perception, Prevalence and Primary Care Physicians’ Knowledge on Childhood Food Allergy in Croatia
Abstract
:1. Introduction
Aims of the Study
2. Patients and Methods
2.1. Patients
2.2. Methods
2.2.1. Investigators
2.2.2. The Questionnaire
2.2.3. Severe Reactions
2.2.4. Allergy Workup and Treatment
2.2.5. Statistical Methods
3. Results
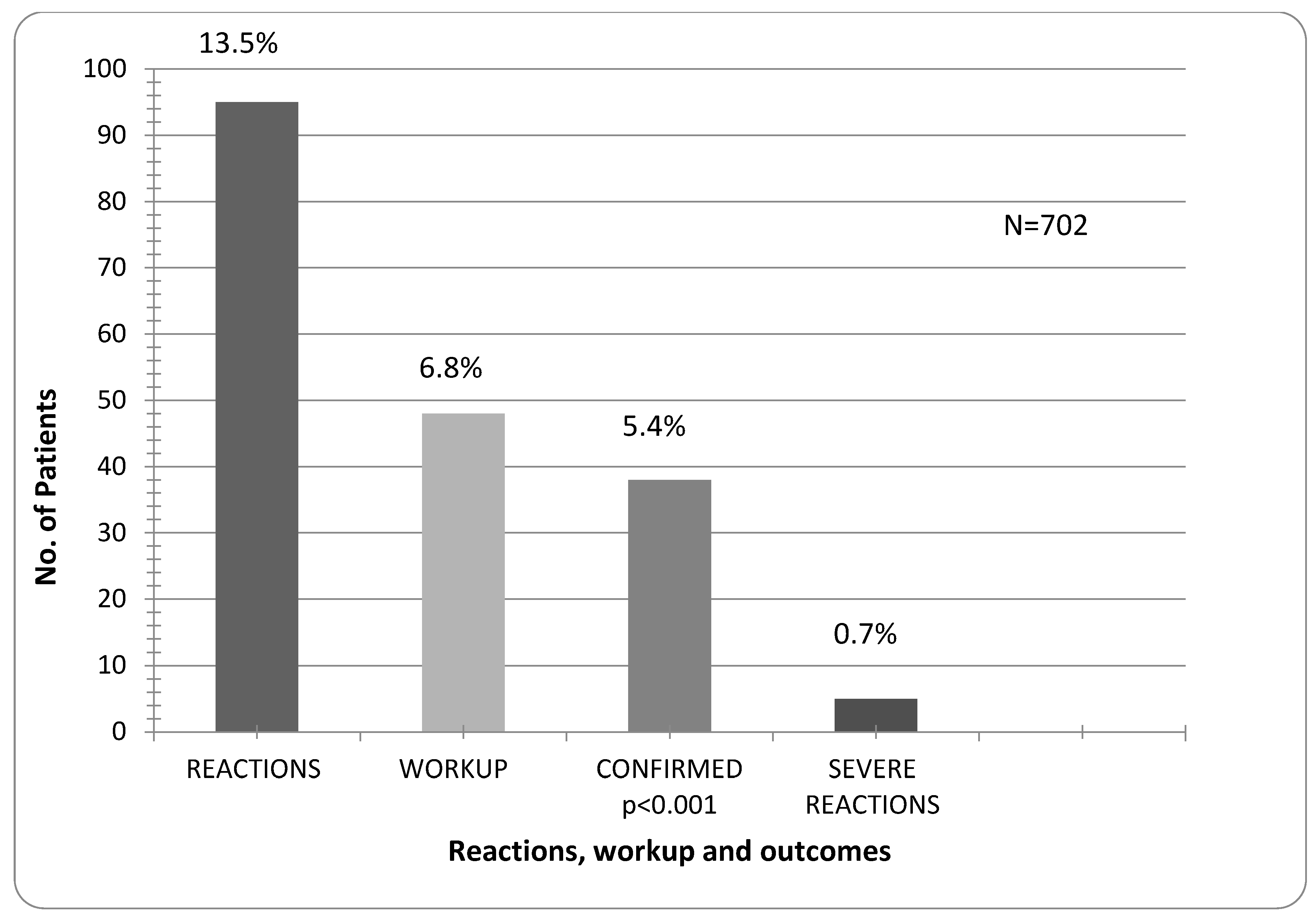
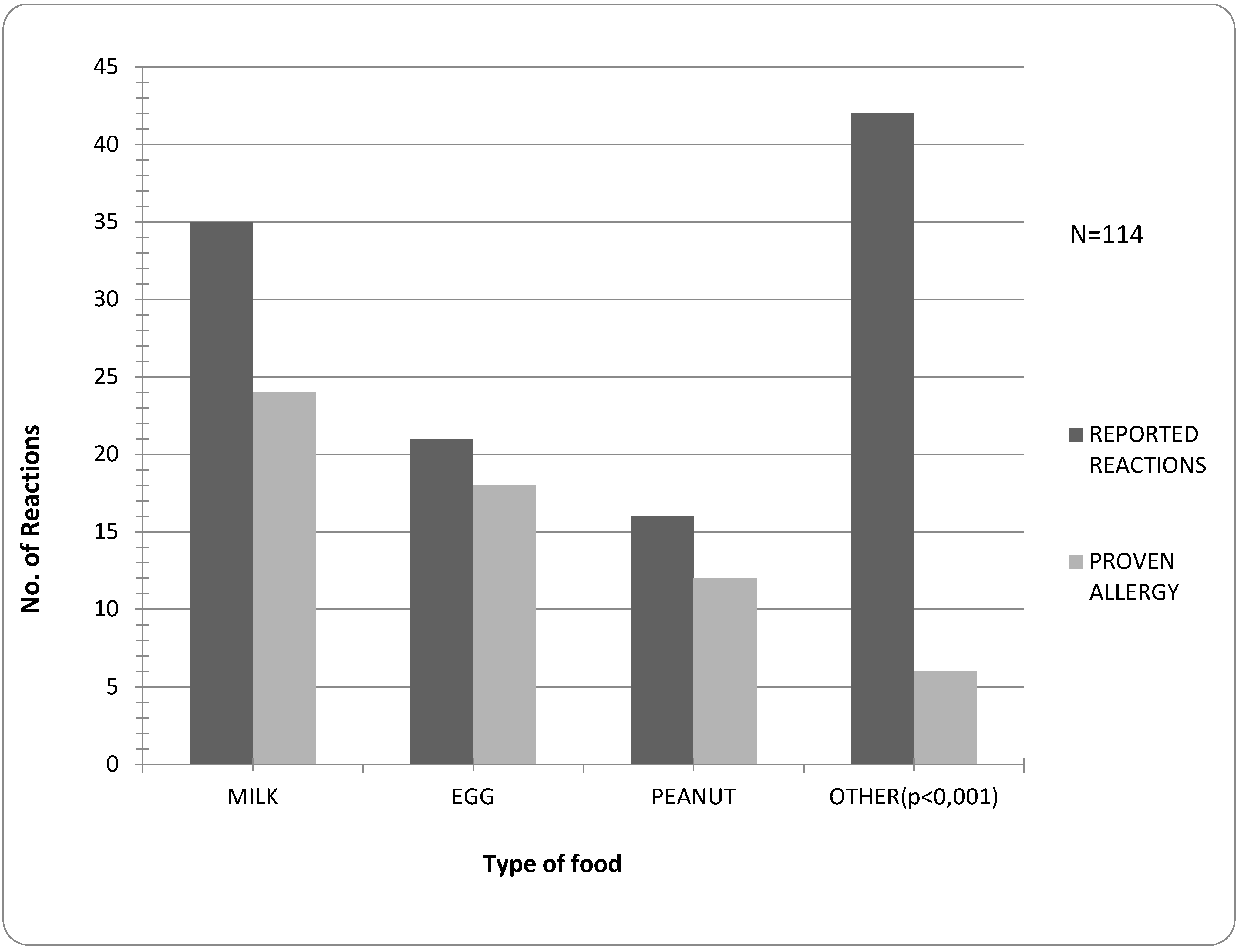
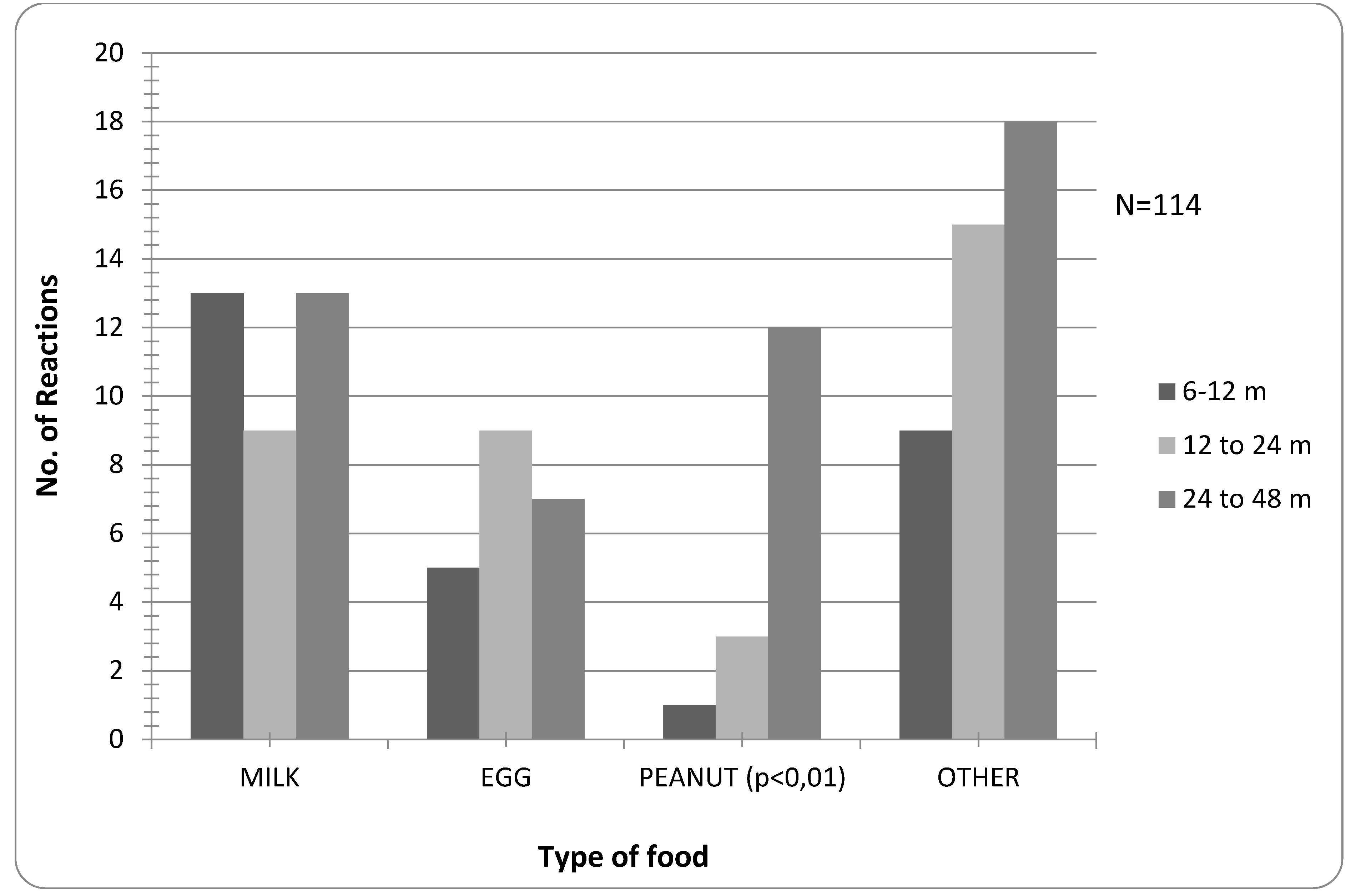
| Age Groups/months | Reactions | Confirmed Allergy | Severe Reactions | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Milk | Egg | Peanut | Other * | N = 702 | N = 702 | |||||||
| N | % | N | % | N | % | N | % | N | % | N | % | ||
| 6–48 | 114 | 35 | 31 | 21 | 18 | 16 | 14 | 42 | 37 | 38 | 5.4 | 5.2 | |
| 5 | 13.1 ** | ||||||||||||
| 6–12 | 28 | 13 | 37 | 5 | 24 | 1 | 6 | 9 | 12 | 9 | 1.2 | 1 | 0.1 |
| 12–24 | 36 | 9 | 26 | 9 | 43 | 3 | 18 | 15 | 36 | 11 | 1.5 | 2 | 0.2 |
| 24–48 | 50 | 13 | 37 | 7 | 33 | 12 | 75 | 18 | 43 | 18 | 2.5 | 2 | 0.2 |


4. Discussion
5. Conclusions
Supplementary Files
Supplementary File 1Acknowledgments
Author Contributions
Conflicts of Interest
References
- Sicherer, S.H. Epidemiology of food allergy. J. Allergy Clin. Immunol. 2011, 127, 594–602. [Google Scholar] [CrossRef] [PubMed]
- Allen, K.J.; Koplin, J.J. The epidemiology of IgE-mediated food allergy and anaphylaxis. Immunol. Allergy Clin. N. Am. 2012, 32, 35–50. [Google Scholar] [CrossRef] [PubMed]
- Nwaru, B.I.; Hickstein, L.; Panesar, S.S.; Muraro, A.; Werfel, T.; Cardona, V.; Dubois, A.E.J.; Halken, S.; Hoffmann-Sommergruber, K.; Poulsen, L.K.; et al. The epidemiology of food allergy in Europe: A systematic review and meta-analysis. Allergy 2014, 69, 62–75. [Google Scholar] [CrossRef] [PubMed]
- Rona, R.J.; Keil, T.; Summers, C.; Gislason, D.; Zuidmeer, L.; Sodergren, E.; Sigurdardottir, S.T.; Lindner, T.; Goldhahn, K.; Dahlstrom, J.; et al. The prevalence of food allergy: A meta-analysis. J. Allergy Clin. Immunol. 2007, 120, 638–646. [Google Scholar] [CrossRef] [PubMed]
- Comberiati, P.; Cipriani, F.; Schwarz, A.; Posa, D.; Host, C.; Peroni, D.G. Diagnosis and treatment of pediatric food allergy: An update. Ital. J. Pediatr. 2015. [Google Scholar] [CrossRef] [PubMed]
- Kummeling, I.; Mills, E.N.; Clausen, M.; Dubakiene, R.; Pérez, C.F.; Fernández-Rivas, M.; Knulst, A.C.; Kowalski, M.L.; Lidholm, J.; Le, T.M.; et al. The EuroPrevall surveys on the prevalence of food allergies in children and adults: Background and study methodology. Allergy 2009, 64, 1493–1497. [Google Scholar] [CrossRef] [PubMed]
- Keil, T. Epidemiology of food allergy: What’s new? A critical appraisal of recent population-based studies. Curr. Opin. Allergy Clin. Immunol. 2007, 7, 259–263. [Google Scholar] [CrossRef] [PubMed]
- Sicherer, S.H.; Sampson, H.A. Food allergy. J. Allergy Clin. Immunol. 2010, 125, S116–S125. [Google Scholar] [CrossRef] [PubMed]
- Keil, T.; McBride, D.; Grimshaw, K.; Niggemann, B.; Xepapadaki, P.; Zannikos, K.; Sigurdardottir, S.T.; Clausen, M.; Reche, M.; Pascual, C.; et al. The multinational birth cohort of EuroPrevall: Background, aims and methods. Allergy 2010, 65, 482–490. [Google Scholar] [CrossRef] [PubMed]
- Osborne, N.J.; Koplin, J.J.; Martin, P.E.; Gurrin, L.C.; Lowe, A.J.; Matheson, M.C.; Ponsonby, A.L.; Wake, M.; Tang, M.L.; Dharmage, S.C.; et al. Prevalence of challenge-proven IgE-mediated food allergy using population-based sampling and predetermined challenge criteria in infants. J. Allergy Clin. Immunol. 2011, 127, 668.e1-2–676.e1-2. [Google Scholar] [CrossRef] [PubMed]
- Woods, R.K.; Stoney, R.M.; Raven, J.; Walters, E.H.; Abramson, M.; Thien, F.C. Reported adverse food reactions overestimate true food allergy in the community. Eur. J. Clin. Nutr. 2002, 56, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Richter, D.; Puževski, D.; Mađerčić, L.; Kniewald, H.; Nogalo, B. Diagnostic work-up in children with nutritional allergy. Curr. Stud. Biotechnol. 2003, 3, 273–282. [Google Scholar]
- Wassenberg, J.; Cochard, M.M.; Dunngalvin, A.; Ballabeni, P.; Flokstra-de Blok, B.M.; Newman, C.J.; Hofer, M.; Eigenmann, P.A. Parent perceived quality of life is age-dependent in children with food allergy. Pediatr. Allergy Immunol. 2012, 23, 412–419. [Google Scholar] [CrossRef] [PubMed]
- Venter, C.; Sommer, I.; Moonesinghe, H.; Grundy, J.; Glasbey, G.; Patil, V.; Dean, T. Health-related quality of life in children with perceived and diagnosed food hypersensitivity. Pediatr. Allergy Immunol. 2015, 26, 126–132. [Google Scholar] [CrossRef] [PubMed]
- Lau, G.Y.; Patel, N.; Umasunthar, T.; Gore, C.; Warner, J.O.; Hanna, H.; Phillips, K.; Mohd Zaki, A.; Hodes, M.; Boyle, R.J. Anxiety and stress in mothers of food-allergic children. Pediatr. Allergy Immunol. 2014, 25, 236–242. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.S.; Springston, E.E.; Kim, J.S.; Smith, B.; Pongracic, J.A.; Wang, X.; Holl, J. Food allergy knowledge, attitudes, and beliefs of primary care physicians. Pediatrics 2010, 125, 126–132. [Google Scholar] [CrossRef] [PubMed]
- DunnGalvin, A.; Dubois, A.E.J.; Flokstra-de Blok, B.M.J.; Hourihane, J.O. The effects of food allergy on quality of life. Chem. Immunol. Allergy 2015, 101, 235–252. [Google Scholar] [PubMed]
- Sampson, H.A.; Muñoz-Furlong, A.; Campbell, R.L.; Adkinson, N.F., Jr.; Bock, S.A.; Branum, A.; Brown, S.G.; Camargo, C.A., Jr.; Cydulka, R.; Galli, S.J.; et al. Second symposium on the definition and management of anaphylaxis: Summary report—Second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network symposium. J. Allergy Clin. Immunol. 2006, 117, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Muraro, A.; Werfel, T.; Hoffmann-Sommergruber, K.; Roberts, G.; Beyer, K.; Bindslev-Jensen, C.; Cardona, V.; Dubois, A.; duToit, G.; Eigenmann, P.; et al. EAACI food allergy and anaphylaxis guidelines: Diagnosis and management of food allergy. Allergy 2014, 69, 1008–1025. [Google Scholar] [CrossRef] [PubMed]
- MedCalc—User-Friendly Statistical Software. Available online: https://www.medcalc.org (accessed on 20 June 2015).
- Lomidze, N.; Gotua, M. Prevalence of self-reported food allergy in different age groups of georgian population. Georgian Med. News 2015, 241, 40–44. [Google Scholar] [PubMed]
- Nwaru, B.I.; Hickstein, L.; Panesar, S.S.; Roberts, G.; Muraro, A.; Sheikh, A.; EAACI Food Allergy and Anaphylaxis Guidelines Group. Prevalence of common food allergies in Europe: A systematic review and meta-analysis. Allergy 2014, 69, 992–1007. [Google Scholar] [PubMed]
- Dyer, A.A.; Rivkina, V.; Perumal, D.; Smeltzer, B.M.; Smith, B.M.; Gupta, R.S. Epidemiology of childhood peanut allergy. Allergy Asthma Proc. 2015, 36, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Umasunthar, T.; Leonardi-Bee, J.; Turner, P.J.; Hodes, M.; Gore, C.; Warner, J.O.; Boyle, R.J. Incidence of food anaphylaxis in people with food allergy: A systematic review and meta-analysis. Clin. Exp. Allergy 2014. [Google Scholar] [CrossRef] [PubMed]
- Saleh-Langenberg, J.; Goossens, N.J.; Flokstra-deBlok, B.M.J.; Kollen, B.J.; van der Meulen, G.N.; Le, T.M.; Knulst, A.C.; Jedrzejczak-Czechowica, M.; Kowalski, M.L.; Rokicka, E.; et al. Predictors of health-related quality of life of European food-allergic patients. Allergy 2015, 70, 616–624. [Google Scholar] [CrossRef] [PubMed]
- Chad, L.; Ben-Shoshan, M.; Asai, Y.; Cherkaoui, S.; Alizadehfar, R.; St-Pierre, Y.; Harada, L.; Allen, M.; Clarke, A. A majority of parents of children with peanut allergy fear using the epinephrine auto-injector. Allergy 2013, 68, 1605–1609. [Google Scholar] [CrossRef] [PubMed]
- Muraro, A.; Dubois, A.E.; DunnGalvin, A.; Hourihane, J.O.; de Jong, N.W.; Meyer, R.; Panesar, S.S.; Roberts, G.; Salvilla, S.; Sheikh, A.; et al. EAACI Food Allergy and Anaphylaxis Guidelines. Food allergy health-related quality of life measures. Allergy 2014, 69, 845–853. [Google Scholar] [CrossRef] [PubMed]
- Jutel, M.; Papadopoulos, N.G.; Gronlund, H.; Hoffman, H.J.; Bohle, B.; Hellings, P.; Brraunsthal, G.J.; Muraro, A.; Schmidt-Grendelmeier, P.; Zuberbier, T.; et al. Recommendations for the allergy menagement in the primary care. Allergy 2014, 69, 708–718. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baricic, T.V.; Catipovic, M.; Cetinic, E.L.; Krmek, V.; Horvat, I. Parental Perception, Prevalence and Primary Care Physicians’ Knowledge on Childhood Food Allergy in Croatia. Children 2015, 2, 305-316. https://doi.org/10.3390/children2030305
Baricic TV, Catipovic M, Cetinic EL, Krmek V, Horvat I. Parental Perception, Prevalence and Primary Care Physicians’ Knowledge on Childhood Food Allergy in Croatia. Children. 2015; 2(3):305-316. https://doi.org/10.3390/children2030305
Chicago/Turabian StyleBaricic, Tamara Voskresensky, Marija Catipovic, Erina L. Cetinic, Vlado Krmek, and Ivona Horvat. 2015. "Parental Perception, Prevalence and Primary Care Physicians’ Knowledge on Childhood Food Allergy in Croatia" Children 2, no. 3: 305-316. https://doi.org/10.3390/children2030305
APA StyleBaricic, T. V., Catipovic, M., Cetinic, E. L., Krmek, V., & Horvat, I. (2015). Parental Perception, Prevalence and Primary Care Physicians’ Knowledge on Childhood Food Allergy in Croatia. Children, 2(3), 305-316. https://doi.org/10.3390/children2030305





