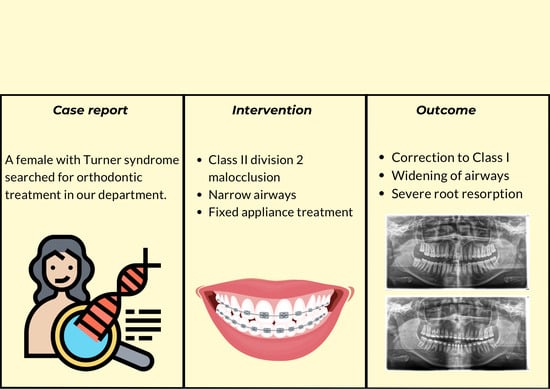
Complication of Orthodontic Treatment: A Case Report on Severe Apical Root Resorption (ARR) in a Patient with Turner Syndrome
Abstract
:1. Introduction
2. Materials and Methods
2.1. Diagnosis and Aetiology
2.2. Treatment Objectives
2.3. Treatment Progress
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gravholt, C.H.; Viuff, M.H.; Brun, S.; Stochholm, K.; Andersen, N.H. Turner syndrome: Mechanisms and management. Nat. Rev. Endocrinol. 2019, 15, 601–614. [Google Scholar] [CrossRef] [PubMed]
- Caino, S.; Cubilla, M.A.; Alba, R.; Obregón, M.G.; Fano, V.; Gómez, A.; Zecchini, L.; Lapunzina, P.; Aza-Carmona, M.; Heath, K.E.; et al. Clinical and Genetic Analysis of Multiple Osteochondromas in a Cohort of Argentine Patients. Genes 2022, 13, 2063. [Google Scholar] [CrossRef] [PubMed]
- Isojima, T.; Yokoya, S. Growth in girls with Turner syndrome. Front. Endocrinol. 2023, 13, 1068128. [Google Scholar] [CrossRef] [PubMed]
- Leone, P.E.; Yumiceba, V.; Jijón-Vergara, A.; Pérez-Villa, A.; Armendáriz-Castillo, I.; García-Cárdenas, J.M.; Guerrero, S.; Guevara-Ramírez, P.; López-Cortés, A.; Zambrano, A.K.; et al. Cytogenetic and genomic analysis of a patient with turner syndrome and t(2;12): A case report. Mol. Cytogenet. 2020, 13, 46. [Google Scholar] [CrossRef] [PubMed]
- Ahiko, N.; Baba, Y.; Tsuji, M.; Horikawa, R.; Moriyama, K. Investigation of maxillofacial morphology and oral characteristics with Turner syndrome and early mixed dentition. Congenit. Anom. 2019, 59, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Horrocks, L.R.; Brook, A.; Alvesalo, L.; Smith, R.N. A three-dimensional comparison of the modifying effects of familial genetic contribution in Turner syndrome. Front. Oral Biol. 2009, 13, 148–152. [Google Scholar] [CrossRef] [PubMed]
- Rizell, S.; Barrenäs, M.L.; Andlin-Sobocki, A.; Stecksén-Blicks, C.; Kjellberg, H. Turner syndrome isochromosome karyotype correlates with decreased dental crown width. Eur. J. Orthod. 2012, 34, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Kjellberg, H.; Lundgren, T.; Barrenäs, M.L.; Rizell, S. Apical root resorptions in girls with Turner syndrome: A controlled longitudinal study. Eur. J. Orthod. 2022, 44, 705–710. [Google Scholar] [CrossRef] [PubMed]
- Calheiros-Lobo, M.J.; Costa, F.; Pinho, T. Infraocclusion level and root resorption of the primary molar in second premolar agenesis: A retrospective cross-sectional study in the Portuguese population. Dent. Med. Probl. 2022, 59, 195–207. [Google Scholar] [CrossRef] [PubMed]
- Vidal-Manyari, P.A.; Arriola-Guillén, L.E.; Jimenez-Valdivia, L.M.; Dias-Da Silveira, H.L.; Boessio-Vizzotto, M. Effect of the application of software on the volumetric and cross-sectional assessment of the oropharyngeal airway of patients with and without an open bite: A CBCT study. Dent. Med. Probl. 2022, 59, 397–405. [Google Scholar] [CrossRef] [PubMed]
- Tahmasbi, S.; Seifi, M.; Soleymani, A.A.; Mohamadian, F.; Alam, M. Comparative study of changes in the airway dimensions following the treatment of Class II malocclusion patients with the twin-block and Seifi appliances. Dent. Med. Probl. 2023, 60, 247–254. [Google Scholar] [CrossRef] [PubMed]
- Villaman-Santacruz, H.; Torres-Rosas, R.; Acevedo-Mascarúa, A.E.; Argueta-Figueroa, L. Root resorption factors associated with orthodontic treatment with fixed appliances: A systematic review and meta-analysis. Dent. Med. Probl. 2022, 59, 437–450. [Google Scholar] [CrossRef] [PubMed]
- Dindaroğlu, F.; Doğan, S. Root Resorption in Orthodontics. Turk. J. Orthod. 2016, 29, 103–108. [Google Scholar] [CrossRef] [PubMed]
- Clemente, E.G.; Penukonda, S.K.; Doan, T.; Sullivan, B.; Kanungo, S. Turner Syndrome. Endocrines 2022, 3, 240–254. [Google Scholar] [CrossRef]
- Väänänen, H.K.; Härkönen, P.L. Estrogen and bone metabolism. Maturitas 1996, 23, S65–S69. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Deng, S.; Mei, L.; Li, Z.; Zhang, X.; Yang, C.; Li, Y. Prevalence and severity of apical root resorption during orthodontic treatment with clear aligners and fixed appliances: A cone beam computed tomography study. Prog. Orthod. 2020, 21, 1. [Google Scholar] [CrossRef] [PubMed]
- Yassir, Y.A.; Nabbat, S.A.; McIntyre, G.T.; Bearn, D.R. Clinical effectiveness of clear aligner treatment compared to fixed appliance treatment: An overview of systematic reviews. Clin. Oral Investig. 2022, 26, 2353–2370. [Google Scholar] [CrossRef] [PubMed]
- Chiarito, M.; Piacente, L.; Chaoul, N.; Pontrelli, P.; D’Amato, G.; Grandone, A.; Russo, G.; Street, M.E.; Wasniewska, M.G.; Brunetti, G.; et al. Role of Wnt-signaling inhibitors DKK-1 and sclerostin in bone fragility associated with Turner syndrome. J. Endocrinol. Investig. 2022, 45, 1255–1263. [Google Scholar] [CrossRef] [PubMed]
- Apajalahti, S.; Peltola, J.S. Apical root resorption after orthodontic treatment-a retrospective study. Eur. J. Orthod. 2007, 29, 408–411. [Google Scholar] [CrossRef] [PubMed]
- Smale, I.; Artun, J.; Behbehani, F.; Doppel, D.; van’t Hof, M.; Kuijpers-Jagtman, A.M. Apical root resorption 6 months after initiation of fixed orthodontic appliance therapy. Am. J. Orthod. 2005, 128, 57–67. [Google Scholar] [CrossRef] [PubMed]










| Pre-Treatment Value | Post-Treatment Value | Ref. Value | |
|---|---|---|---|
| SNA (°) | 81.03 | 80.69 | 82 |
| SNB (°) | 73.43 | 76.16 | 80 |
| ANB (°) | 7.61 | 4.52 | 2 |
| Wits appraisal (mm) | 6.73 | 2.17 | −0.3 |
| NS-Sar-ArGo-GoMe (°) | 398.9 | 398.7 | 396 |
| FMA (°) | 25 | 24.79 | 25 |
| Gonial angle (°) | 120 | 125 | 125 |
| U1–NA (mm) | 1.55 | 3.32 | 4 |
| U1–SN (°) | 89.48 | 111.48 | 102 |
| L1–NB (mm) | 5.2 | 5.98 | 4 |
| L1–NB (°) | 26.99 | 31.77 | 25 |
| L1–GoMe (°) | 90.3 | 94.8 | 95 |
| Nasolabial Angle | 100.84 | 75.32 | 95 |
| Lower Lip to E-Plane (mm) | 1.66 | 3.65 | −2 |
| Upper Lip to E-Plane (mm) | 2.55 | 1.97 | −4.7 |
| IMPA (°) | 98.81 | 101.16 | 90 |
| Overjet (mm) | 4.87 | 3.98 | 2 |
| Overbite (mm) | 6.43 | 0.74 | 2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Laskowska, J.; Paradowska-Stolarz, A.; Miralles-Jordá, L.; Schutty, D.; Mikulewicz, M. Complication of Orthodontic Treatment: A Case Report on Severe Apical Root Resorption (ARR) in a Patient with Turner Syndrome. Children 2024, 11, 358. https://doi.org/10.3390/children11030358
Laskowska J, Paradowska-Stolarz A, Miralles-Jordá L, Schutty D, Mikulewicz M. Complication of Orthodontic Treatment: A Case Report on Severe Apical Root Resorption (ARR) in a Patient with Turner Syndrome. Children. 2024; 11(3):358. https://doi.org/10.3390/children11030358
Chicago/Turabian StyleLaskowska, Joanna, Anna Paradowska-Stolarz, Lucía Miralles-Jordá, Dorota Schutty, and Marcin Mikulewicz. 2024. "Complication of Orthodontic Treatment: A Case Report on Severe Apical Root Resorption (ARR) in a Patient with Turner Syndrome" Children 11, no. 3: 358. https://doi.org/10.3390/children11030358