Endothelial Damage and the Microcirculation in Critical Illness
Abstract
:1. Introduction
Endothelial Glycocalyx in Clinical Practice
2. Measuring the Glycocalyx
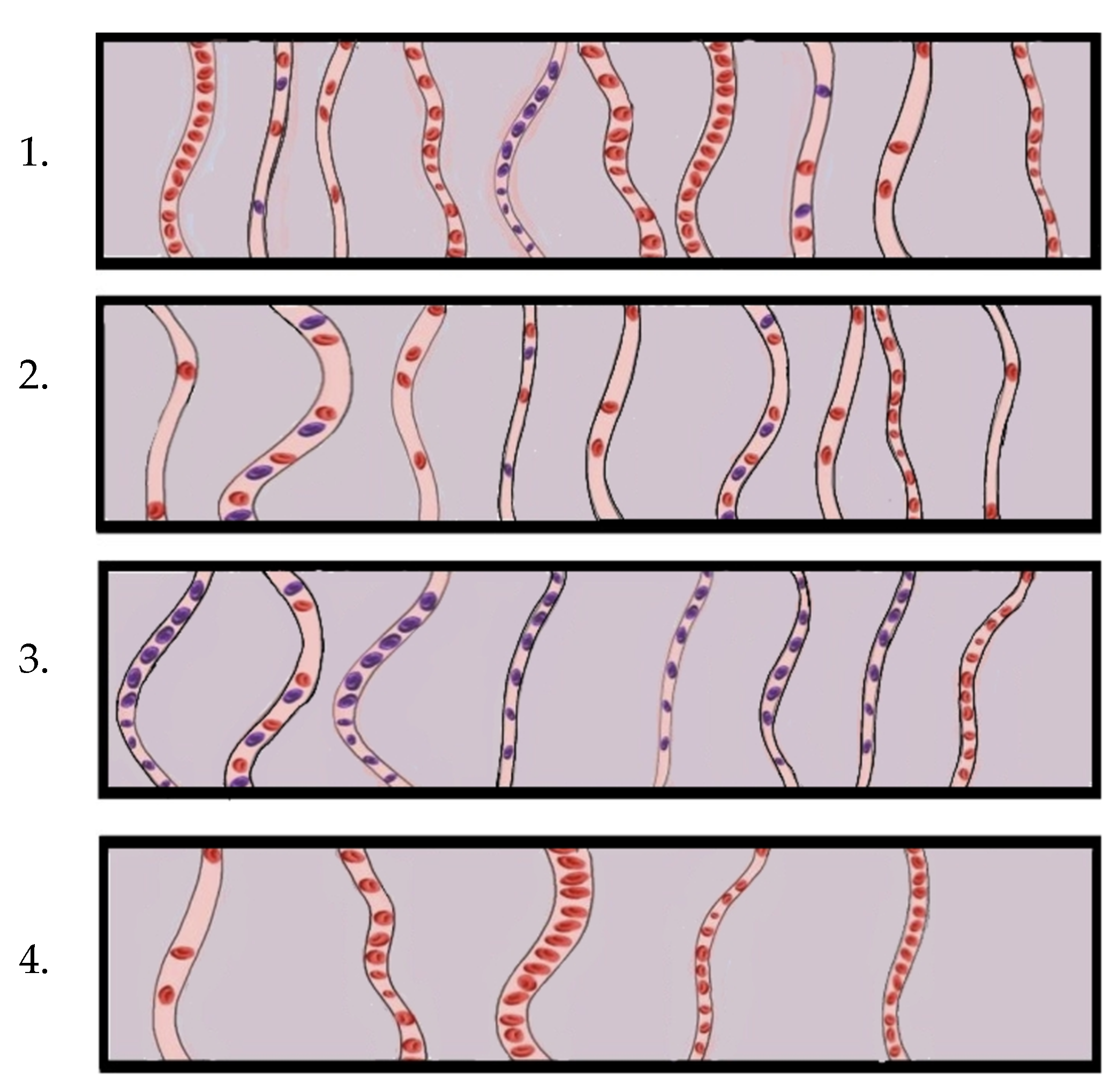
3. Visualising the Microcirculation and the Endothelial Glycocalyx
3.1. The Sublingual Target Region
3.2. Near Infrared Spectroscopy and the Microcirculation
4. Clinical Applications of Microcirculation Monitoring
4.1. Haemorrhage and Trauma
4.2. Cardiac Component
4.3. Sepsis and Septic Shock
5. Haemodynamic Coherence and Personalised Treatment in ICU
6. Prognostic Value of Glycocalyx Damage in Critical Illness
7. Restoration of Glycocalyx Function
7.1. Fluid Therapy and the Glycocalyx
7.2. Corticosteroids and the Glycocalyx
7.3. Anticoagulants and the Glycocalyx
8. Future Directions
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Scorcella, C.; Damiani, E.; Domizi, R.; Pierantozzi, S.; Tondi, S.; Carsetti, A.; Ciucani, S.; Monaldi, V.; Rogani, M.; Marini, B.; et al. MicroDAIMON Study: Microcirculatory DAIly MONitoring in Critically Ill Patients: A Prospective Observational Study. Ann. Intensive Care 2018, 8, 64. [Google Scholar] [CrossRef] [PubMed]
- Vellinga, N.A.R.; Boerma, E.C.; Koopmans, M.; Donati, A.; Dubin, A.; Shapiro, N.I.; Pearse, R.M.; Machado, F.R.; Fries, M.; Akarsu-Ayazoglu, T.; et al. International Study on Microcirculatory Shock Occurrence in Acutely Ill Patients. Crit. Care Med. 2015, 43, 48–56. [Google Scholar] [CrossRef] [PubMed]
- De Backer, D.; Donadello, K.; Sakr, Y.; Ospina-Tascon, G.; Salgado, D.; Scolletta, S.; Vincent, J.-L. Microcirculatory Alterations in Patients with Severe Sepsis: Impact of Time of Assessment and Relationship with Outcome. Crit. Care Med. 2013, 41, 791–799. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ghitescu, L.; Robert, M. Diversity in Unity: The Biochemical Composition of the Endothelial Cell Surface Varies between the Vascular Beds. Microsc. Res. Tech. 2002, 57, 381–389. [Google Scholar] [CrossRef] [PubMed]
- Reitsma, S.; Slaaf, D.W.; Vink, H.; van Zandvoort, M.A.M.J.; oude Egbrink, M.G.A. The Endothelial Glycocalyx: Composition, Functions, and Visualization. Pflugers Arch. 2007, 454, 345–359. [Google Scholar] [CrossRef] [Green Version]
- Iba, T.; Levy, J.H. Derangement of the Endothelial Glycocalyx in Sepsis. J. Thromb. Haemost. 2019, 17, 283–294. [Google Scholar] [CrossRef] [Green Version]
- De Backer, D.; Creteur, J.; Preiser, J.-C.; Dubois, M.-J.; Vincent, J.-L. Microvascular Blood Flow Is Altered in Patients with Sepsis. Am. J. Respir. Crit. Care Med. 2002, 166, 98–104. [Google Scholar] [CrossRef]
- Van den Berg, B.; Vink, H. Glycocalyx Perturbation: Cause or Consequence of Damage to the Vasculature? Am. J. Physiol.-Heart Circ. Physiol. 2006, 290, H2174–H2175. [Google Scholar] [CrossRef]
- Van den Berg, B.M.; Vink, H.; Spaan, J.A.E. The Endothelial Glycocalyx Protects against Myocardial Edema. Circ. Res. 2003, 92, 592–594. [Google Scholar] [CrossRef] [Green Version]
- Van Golen, R.F.; van Gulik, T.M.; Heger, M. Mechanistic Overview of Reactive Species-Induced Degradation of the Endothelial Glycocalyx during Hepatic Ischemia/Reperfusion Injury. Free Radic. Biol. Med. 2012, 52, 1382–1402. [Google Scholar] [CrossRef]
- Nieuwdorp, M.; Mooij, H.L.; Kroon, J.; Atasever, B.; Spaan, J.A.E.; Ince, C.; Holleman, F.; Diamant, M.; Heine, R.J.; Hoekstra, J.B.L.; et al. Endothelial Glycocalyx Damage Coincides with Microalbuminuria in Type 1 Diabetes. Diabetes 2006, 55, 1127–1132. [Google Scholar] [CrossRef] [Green Version]
- Ikonomidis, I.; Thymis, J.; Simitsis, P.; Koliou, G.-A.; Katsanos, S.; Triantafyllou, C.; Kousathana, F.; Pavlidis, G.; Kountouri, A.; Polyzogopoulou, E.; et al. Impaired Endothelial Glycocalyx Predicts Adverse Outcome in Subjects Without Overt Cardiovascular Disease: A 6-Year Follow-up Study. J. Cardiovasc. Transl. Res. 2021, 15, 890–902. [Google Scholar] [CrossRef]
- Ikonomidis, I.; Voumvourakis, A.; Makavos, G.; Triantafyllidi, H.; Pavlidis, G.; Katogiannis, K.; Benas, D.; Vlastos, D.; Trivilou, P.; Varoudi, M.; et al. Association of Impaired Endothelial Glycocalyx with Arterial Stiffness, Coronary Microcirculatory Dysfunction, and Abnormal Myocardial Deformation in Untreated Hypertensives. J. Clin. Hypertens. Greenwich Conn 2018, 20, 672–679. [Google Scholar] [CrossRef] [Green Version]
- Keramida, K.; Thymis, J.; Anastasiou, M.; Katogiannis, K.; Kotsantis, I.; Economopoulou, P.; Pappa, V.; Tsirigotis, P.; Bistola, V.; Thodi, M.; et al. Endothelial Glycocalyx Integrity in Oncological Patients. Int. J. Cardiol. 2022, 360, 62–67. [Google Scholar] [CrossRef]
- Zhang, C.E.; Staals, J.; van Oostenbrugge, R.J.; Vink, H. Uncoupling of Microvascular Blood Flow and Capillary Density in Vascular Cognitive Impairment. Front. Neurol. 2019, 10, 1268. [Google Scholar] [CrossRef] [Green Version]
- Weissgerber, T.L.; Garcia-Valencia, O.; Milic, N.; Codsi, E.; Cubro, H.; Nath, M.C.; White, W.M.; Nath, K.A.; Garovic, V.D. Early Onset Preeclampsia Is Associated with Glycocalyx Degradation and Reduced Microvascular Perfusion. J. Am. Heart Assoc. 2019, 8, 10647. [Google Scholar] [CrossRef] [Green Version]
- Mitsides, N.; Cornelis, T.; Broers, N.J.H.; Diederen, N.M.P.; Brenchley, P.; van der Sande, F.M.; Schalkwijk, C.G.; Kooman, J.P.; Mitra, S. Extracellular Overhydration Linked with Endothelial Dysfunction in the Context of Inflammation in Haemodialysis Dependent Chronic Kidney Disease. PLoS ONE 2017, 12, e0183281. [Google Scholar] [CrossRef] [Green Version]
- Dane, M.J.C.; Khairoun, M.; Lee, D.H.; van den Berg, B.M.; Eskens, B.J.M.; Boels, M.G.S.; van Teeffelen, J.W.G.E.; Rops, A.L.W.M.M.; van der Vlag, J.; van Zonneveld, A.J.; et al. Association of Kidney Function with Changes in the Endothelial Surface Layer. Clin. J. Am. Soc. Nephrol. 2014, 9, 698–704. [Google Scholar] [CrossRef] [Green Version]
- Van der Velden, A.I.M.; van den Berg, B.M.; de Mutsert, R.; van der Vlag, J.; Jukema, J.W.; Rosendaal, F.R.; Rabelink, T.J.; Vink, H. Microvascular Differences in Individuals with Obesity at Risk of Developing Cardiovascular Disease. Obesity 2021, 29, 1439–1444. [Google Scholar] [CrossRef]
- Martens, R.J.H.; Vink, H.; van Oostenbrugge, R.J.; Staals, J. Sublingual Microvascular Glycocalyx Dimensions in Lacunar Stroke Patients. Cerebrovasc. Dis. 2013, 35, 451–454. [Google Scholar] [CrossRef]
- Machin, D.R.; Bloom, S.I.; Campbell, R.A.; Phuong, T.T.T.; Gates, P.E.; Lesniewski, L.A.; Rondina, M.T.; Donato, A.J. Advanced Age Results in a Diminished Endothelial Glycocalyx. Am. J. Physiol.-Heart Circ. Physiol. 2018, 315, 18. [Google Scholar] [CrossRef]
- Lambadiari, V.; Mitrakou, A.; Kountouri, A.; Thymis, J.; Katogiannis, K.; Korakas, E.; Varlamos, C.; Andreadou, I.; Tsoumani, M.; Triantafyllidi, H.; et al. Association of COVID-19 with Impaired Endothelial Glycocalyx, Vascular Function and Myocardial Deformation Four Months after Infection. Eur. J. Heart Fail. 2021, 23, 1916–1926. [Google Scholar] [CrossRef] [PubMed]
- Hou, P.C.; Filbin, M.R.; Wang, H.; Ngo, L.; Huang, D.T.; Aird, W.C.; Yealy, D.M.; Angus, D.C.; Kellum, J.A.; Shapiro, N.I. Endothelial Permeability and Hemostasis in Septic Shock: Results from the ProCESS Trial. Chest 2017, 152, 22–31. [Google Scholar] [CrossRef] [PubMed]
- Boscolo, A.; Pasin, L.; Sella, N.; Pretto, C.; Tocco, M.; Tamburini, E.; Rosi, P.; Polati, E.; Donadello, K.; Gottin, L.; et al. Outcomes of COVID-19 Patients Intubated after Failure of Non-Invasive Ventilation: A Multicenter Observational Study. Sci. Rep. 2021, 11, 17730. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Torres, V.; Muñoz-Serrano, A.; Calderón-Parra, J.; Mills-Sánchez, P.; Pintos-Pascual, I.; Rodríguez-Olleros, C.; Ibánez-Estéllez, F.; Tung-Chen, Y.; Ramos-Martínez, A.; Vargas-Núñez, J.A.; et al. Mortality by COVID-19 Before Vaccination—One Year Experience of Hospitalized Patients in Madrid. Int. J. Infect. Dis. 2022, 116, 339–343. [Google Scholar] [CrossRef]
- Hamming, I.; Timens, W.; Bulthuis, M.; Lely, A.; Navis, G.; van Goor, H. Tissue Distribution of ACE2 Protein, the Functional Receptor for SARS Coronavirus. A First Step in Understanding SARS Pathogenesis. J. Pathol. 2004, 203, 631–637. [Google Scholar] [CrossRef]
- Astapenko, D.; Tomasova, A.; Ticha, A.; Hyspler, R.; Chua, H.S.; Manzoor, M.; Skulec, R.; Lehmann, C.; Hahn, R.; Malbrain, M.L.; et al. Endothelial Glycocalyx Damage in Patients with Severe COVID-19 on Mechanical Ventilation—A Prospective Observational Pilot Study. Clin. Hemorheol. Microcirc. 2022, 81, 205–219. [Google Scholar] [CrossRef]
- Rovas, A.; Osiaevi, I.; Buscher, K.; Sackarnd, J.; Tepasse, P.-R.; Fobker, M.; Kühn, J.; Braune, S.; Göbel, U.; Thölking, G.; et al. Microvascular Dysfunction in COVID-19: The MYSTIC Study. Angiogenesis 2021, 24, 145–157. [Google Scholar] [CrossRef]
- Borgel, D.; Chocron, R.; Grimaud, M.; Philippe, A.; Chareyre, J.; Brakta, C.; Lasne, D.; Bonnet, D.; Toubiana, J.; Angoulvant, F.; et al. Endothelial Dysfunction as a Component of Severe Acute Respiratory Syndrome Coronavirus 2–Related Multisystem Inflammatory Syndrome in Children with Shock. Crit. Care Med. 2021, 49, e1151–e1156. [Google Scholar] [CrossRef]
- Hu, B.; Huang, S.; Yin, L. The Cytokine Storm and COVID-19. J. Med. Virol. 2020, 93, 250–256. [Google Scholar] [CrossRef]
- Ackermann, M.; Verleden, S.E.; Kuehnel, M.; Haverich, A.; Welte, T.; Laenger, F.; Vanstapel, A.; Werlein, C.; Stark, H.; Tzankov, A.; et al. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in COVID-19. N. Engl. J. Med. 2020, 383, 120–128. [Google Scholar] [CrossRef]
- Varga, Z.; Flammer, A.J.; Steiger, P.; Haberecker, M.; Andermatt, R.; Zinkernagel, A.S.; Mehra, M.R.; Schuepbach, R.A.; Ruschitzka, F.; Moch, H. Endothelial Cell Infection and Endotheliitis in COVID-19. Lancet 2020, 395, 1417–1418. [Google Scholar] [CrossRef]
- Pries, A.R.; Secomb, T.W.; Gaehtgens, P. The Endothelial Surface Layer. Pflüg. Arch. Eur. J. Physiol. 2000, 440, 653–666. [Google Scholar] [CrossRef]
- Luft, J.H. Fine Structures of Capillary and Endocapillary Layer as Revealed by Ruthenium Red. Fed. Proc. 1966, 25, 1773–1783. [Google Scholar]
- Kolářová, H.; Ambrůzová, B.; Švihálková Šindlerová, L.; Klinke, A.; Kubala, L. Modulation of Endothelial Glycocalyx Structure under Inflammatory Conditions. Mediators Inflamm. 2014, 2014, 694312. [Google Scholar] [CrossRef] [Green Version]
- Subramanian, S.V.; Fitzgerald, M.L.; Bernfield, M. Regulated Shedding of Syndecan-1 and -4 Ectodomains by Thrombin and Growth Factor Receptor Activation. J. Biol. Chem. 1997, 272, 14713–14720. [Google Scholar] [CrossRef] [Green Version]
- Götte, M. Syndecans in Inflammation. FASEB J. 2003, 17, 575–591. [Google Scholar] [CrossRef] [Green Version]
- Alexopoulou, A.N.; Multhaupt, H.A.B.; Couchman, J.R. Syndecans in Wound Healing, Inflammation and Vascular Biology. Int. J. Biochem. Cell Biol. 2007, 39, 505–528. [Google Scholar] [CrossRef]
- Voyvodic, P.L.; Min, D.; Liu, R.; Williams, E.; Chitalia, V.; Dunn, A.K.; Baker, A.B. Loss of Syndecan-1 Induces a Pro-Inflammatory Phenotype in Endothelial Cells with a Dysregulated Response to Atheroprotective Flow. J. Biol. Chem. 2014, 289, 9547–9559. [Google Scholar] [CrossRef] [Green Version]
- Bertrand, J.; Bollmann, M. Soluble Syndecans: Biomarkers for Diseases and Therapeutic Options. Br. J. Pharmacol. 2019, 176, 67–81. [Google Scholar] [CrossRef]
- Nelson, A.; Berkestedt, I.; Bodelsson, M. Circulating Glycosaminoglycan Species in Septic Shock. Acta Anaesthesiol. Scand. 2014, 58, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Steppan, J.; Hofer, S.; Funke, B.; Brenner, T.; Henrich, M.; Martin, E.; Weitz, J.; Hofmann, U.; Weigand, M.A. Sepsis and Major Abdominal Surgery Lead to Flaking of the Endothelial Glycocalix. J. Surg. Res. 2011, 165, 136–141. [Google Scholar] [CrossRef] [PubMed]
- Rehm, M.; Bruegger, D.; Christ, F.; Conzen, P.; Thiel, M.; Jacob, M.; Chappell, D.; Stoeckelhuber, M.; Welsch, U.; Reichart, B.; et al. Shedding of the Endothelial Glycocalyx in Patients Undergoing Major Vascular Surgery with Global and Regional Ischemia. Circulation 2007, 116, 1896–1906. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seidel, C.; Ringdén, O.; Remberger, M. Increased Levels of Syndecan-1 in Serum during Acute Graft-versus-Host Disease. Transplantation 2003, 76, 423–426. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.; Nagar, H.; Lee, J.W.; Kim, S.; Lee, I.; Piao, S.; Choi, S.; Kim, C.-S. Effect of Ulinastatin on Syndecan-2-Mediated Vascular Damage in IDH2-Deficient Endothelial Cells. Biomedicines 2022, 10, 187. [Google Scholar] [CrossRef]
- Choi, S.; Chung, H.; Hong, H.; Kim, S.Y.; Kim, S.-E.; Seoh, J.-Y.; Moon, C.M.; Yang, E.G.; Oh, E.-S. Inflammatory Hypoxia Induces Syndecan-2 Expression through IL-1b–Mediated FOXO3a Activation in Colonic Epithelia. FASEB J. 2017, 31, 1516–1530. [Google Scholar] [CrossRef] [Green Version]
- Halden, Y.; Rek, A.; Atzenhofer, W.; Szilak, L.; Wabnig, A.; Kungl, A.J. Interleukin-8 Binds to Syndecan-2 on Human Endothelial Cells. Biochem. J. 2004, 377, 533–538. [Google Scholar] [CrossRef] [Green Version]
- Arokiasamy, S.; Balderstone, M.J.M.; De Rossi, G.; Whiteford, J.R. Syndecan-3 in Inflammation and Angiogenesis. Front. Immunol. 2020, 10, 3010. [Google Scholar]
- Thrombin-Cleaved Syndecan-3/-4 Ectodomain Fragments Mediate Endothelial Barrier Dysfunction | PLoS ONE. Available online: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0214737 (accessed on 22 November 2022).
- Götte, M.; Joussen, A.M.; Klein, C.; Andre, P.; Wagner, D.D.; Hinkes, M.T.; Kirchhof, B.; Adamis, A.P.; Bernfield, M. Role of Syndecan-1 in Leukocyte–Endothelial Interactions in the Ocular Vasculature. Invest. Ophthalmol. Vis. Sci. 2002, 43, 1135–1141. [Google Scholar]
- JCI—Delayed Wound Repair and Impaired Angiogenesis in Mice Lacking Syndecan-4. Available online: https://www.jci.org/articles/view/10559 (accessed on 22 November 2022).
- Jiang, D.; Liang, J.; Campanella, G.S.; Guo, R.; Yu, S.; Xie, T.; Liu, N.; Jung, Y.; Homer, R.; Meltzer, E.B.; et al. Inhibition of Pulmonary Fibrosis in Mice by CXCL10 Requires Glycosaminoglycan Binding and Syndecan-4. J. Clin. Invest. 2010, 120, 2049–2057. [Google Scholar] [CrossRef]
- Tanino, Y.; Wang, X.; Nikaido, T.; Misa, K.; Sato, Y.; Togawa, R.; Kawamata, T.; Kikuchi, M.; Frevert, C.W.; Tanino, M.; et al. Syndecan-4 Inhibits the Development of Pulmonary Fibrosis by Attenuating TGF-β Signaling. Int. J. Mol. Sci. 2019, 20, 4989. [Google Scholar] [CrossRef] [Green Version]
- Nikaido, T.; Tanino, Y.; Wang, X.; Sato, S.; Misa, K.; Fukuhara, N.; Sato, Y.; Fukuhara, A.; Uematsu, M.; Suzuki, Y.; et al. Serum Syndecan-4 as a Possible Biomarker in Patients with Acute Pneumonia. J. Infect. Dis. 2015, 212, 1500–1508. [Google Scholar] [CrossRef] [Green Version]
- VanTeeffelen, J.W.; Brands, J.; Stroes, E.S.; Vink, H. Endothelial Glycocalyx: Sweet Shield of Blood Vessels. Trends Cardiovasc. Med. 2007, 17, 101–105. [Google Scholar] [CrossRef]
- Drost, C.C.; Rovas, A.; Kusche-Vihrog, K.; Van Slyke, P.; Kim, H.; Hoang, V.C.; Maynes, J.T.; Wennmann, D.O.; Pavenstädt, H.; Linke, W.; et al. Tie2 Activation Promotes Protection and Reconstitution of the Endothelial Glycocalyx in Human Sepsis. Thromb. Haemost. 2019, 119, 1827–1838. [Google Scholar] [CrossRef]
- Hahn, R.G.; Hasselgren, E.; Björne, H.; Zdolsek, M.; Zdolsek, J. Biomarkers of Endothelial Injury in Plasma Are Dependent on Kidney Function. Clin. Hemorheol. Microcirc. 2019, 72, 161–168. [Google Scholar] [CrossRef]
- Lebel, L. Clearance of Hyaluronan from the Circulation. Adv. Drug Deliv. Rev. 1991, 7, 221–235. [Google Scholar] [CrossRef]
- Salmon, A.H.J.; Satchell, S.C. Endothelial Glycocalyx Dysfunction in Disease: Albuminuria and Increased Microvascular Permeability. J. Pathol. 2012, 226, 562–574. [Google Scholar] [CrossRef]
- Tuma, M.; Canestrini, S.; Alwahab, Z.; Marshall, J. Trauma and Endothelial Glycocalyx: The Microcirculation Helmet? Shock Augusta Ga 2016, 46, 352–357. [Google Scholar] [CrossRef]
- Anand, D.; Ray, S.; Srivastava, L.M.; Bhargava, S. Evolution of Serum Hyaluronan and Syndecan Levels in Prognosis of Sepsis Patients. Clin. Biochem. 2016, 49, 768–776. [Google Scholar] [CrossRef]
- Filho, I.P.T.; Torres, L.N.; Salgado, C.; Dubick, M.A. Plasma Syndecan-1 and Heparan Sulfate Correlate with Microvascular Glycocalyx Degradation in Hemorrhaged Rats after Different Resuscitation Fluids. Am. J. Physiol.-Heart Circ. Physiol. 2016, 310, 16. [Google Scholar] [CrossRef] [Green Version]
- Sack, K.D.; Kellum, J.A.; Parikh, S.M. The Angiopoietin-Tie2 Pathway in Critical Illness. Crit. Care Clin. 2020, 36, 201–216. [Google Scholar] [CrossRef] [PubMed]
- Lukasz, A.; Hillgruber, C.; Oberleithner, H.; Kusche-Vihrog, K.; Pavenstädt, H.; Rovas, A.; Hesse, B.; Goerge, T.; Kümpers, P. Endothelial Glycocalyx Breakdown Is Mediated by Angiopoietin-2. Cardiovasc. Res. 2017, 113, 671–680. [Google Scholar] [CrossRef] [Green Version]
- Vink, H.; Duling, B.R. Identification of Distinct Luminal Domains for Macromolecules, Erythrocytes, and Leukocytes within Mammalian Capillaries. Circ. Res. 1996, 79, 581–589. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.L.; Long, D.S.; Damiano, E.R.; Ley, K. Near-Wall μ-PIV Reveals a Hydrodynamically Relevant Endothelial Surface Layer in Venules In Vivo. Biophys. J. 2003, 85, 637–645. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dilken, O.; Ergin, B.; Ince, C. Assessment of Sublingual Microcirculation in Critically Ill Patients: Consensus and Debate. Ann. Transl. Med. 2020, 8, 793. [Google Scholar] [CrossRef]
- Boerma, E.C. Imaging of the Microcirculation in ICU Patients. Vox Sang. 2013, 105, 25. [Google Scholar] [CrossRef]
- Boerma, E.C. The Microcirculation as a Clinical Concept: Work in Progress. Curr. Opin. Crit. Care 2009, 15, 261–265. [Google Scholar] [CrossRef]
- Van Elteren, H.A.; Ince, C.; Tibboel, D.; Reiss, I.K.M.; de Jonge, R.C.J. Cutaneous Microcirculation in Preterm Neonates: Comparison between Sidestream Dark Field (SDF) and Incident Dark Field (IDF) Imaging. J. Clin. Monit. Comput. 2015, 29, 543–548. [Google Scholar] [CrossRef] [Green Version]
- Goedhart, P.T.; Khalilzada, M.; Bezemer, R.; Merza, J.; Ince, C. Sidestream Dark Field (SDF) Imaging: A Novel Stroboscopic LED Ring-Based Imaging Modality for Clinical Assessment of the Microcirculation. Opt. Express 2007, 15, 15101–15114. [Google Scholar] [CrossRef]
- Lee, D.H.; Dane, M.J.C.; van den Berg, B.M.; Boels, M.G.S.; van Teeffelen, J.W.; de Mutsert, R.; den Heijer, M.; Rosendaal, F.R.; van der Vlag, J.; van Zonneveld, A.J.; et al. Deeper Penetration of Erythrocytes into the Endothelial Glycocalyx Is Associated with Impaired Microvascular Perfusion. PLoS ONE 2014, 9, e96477. [Google Scholar] [CrossRef] [Green Version]
- Eickhoff, M.K.; Winther, S.A.; Hansen, T.W.; Diaz, L.J.; Persson, F.; Rossing, P.; Frimodt-Møller, M. Assessment of the Sublingual Microcirculation with the GlycoCheck System: Reproducibility and Examination Conditions. PLoS ONE 2020, 15, e0243737. [Google Scholar] [CrossRef]
- Rovas, A.; Lukasz, A.-H.; Vink, H.; Urban, M.; Sackarnd, J.; Pavenstädt, H.; Pavenstädt, H.; Kümpers, P. Bedside Analysis of the Sublingual Microvascular Glycocalyx in the Emergency Room and Intensive Care Unit—The GlycoNurse Study. Scand. J. Trauma Resusc. Emerg. Med. 2018, 26, 16. [Google Scholar] [CrossRef] [Green Version]
- Cerny, V.; Astapenko, D.; Burkovskiy, I.; Hyspler, R.; Ticha, A.; Trevors, M.A.; Lehmann, C. Glycocalyx in Vivo Measurement. Clin. Hemorheol. Microcirc. 2017, 67, 499–503. [Google Scholar] [CrossRef]
- Rovas, A.; Sackarnd, J.; Rossaint, J.; Kampmeier, S.; Pavenstädt, H.; Vink, H.; Kümpers, P. Identification of Novel Sublingual Parameters to Analyze and Diagnose Microvascular Dysfunction in Sepsis: The NOSTRADAMUS Study. Crit. Care 2021, 25, 112. [Google Scholar] [CrossRef]
- Verdant, C.; De Backer, D.; Bruhn, A.; Clausi, C.; Su, F.; Wang, Z.; Rodriguez, H.; Pries, A.R. Evaluation of Sublingual and Gut Mucosal Microcirculation in Sepsis: A Quantitative Analysis. Crit. Care Med. 2009, 37, 2875–2881. [Google Scholar] [CrossRef]
- Boerma, E.C.; van der Voort, P.H.J.; Spronk, P.E.; Ince, C. Relationship between Sublingual and Intestinal Microcirculatory Perfusion in Patients with Abdominal Sepsis. Crit. Care Med. 2007, 35, 1055–1060. [Google Scholar] [CrossRef]
- Edul, V.S.K.; Ince, C.; Navarro, N.; Previgliano, L.; Risso-Vazquez, A.; Rubatto, P.N.; Dubin, A. Dissociation between Sublingual and Gut Microcirculation in the Response to a Fluid Challenge in Postoperative Patients with Abdominal Sepsis. Ann. Intensive Care 2014, 4, 39. [Google Scholar]
- De Bruin, A.F.J.; Kornmann, V.N.N.; van der Sloot, K.; van Vugt, J.L.; Gosselink, M.P.; Smits, A.; Van Ramshorst, B.; Boerma, E.C.; Noordzij, P.G.; Boerma, D.; et al. Sidestream Dark Field Imaging of the Serosal Microcirculation during Gastrointestinal Surgery. Colorectal Dis. Off. J. Assoc. Coloproctol. 2016, 18, 103–110. [Google Scholar] [CrossRef]
- Neto, A.S.; Pereira, V.G.M.; Manetta, J.A.; Espósito, D.C.; Schultz, M.J. Association between Static and Dynamic Thenar Near-Infrared Spectroscopy and Mortality in Patients with Sepsis: A Systematic Review and Meta-Analysis. J. Trauma Acute Care Surg. 2014, 76, 226–233. [Google Scholar] [CrossRef]
- Shapiro, N.I.; Arnold, R.; Sherwin, R.; O’Connor, J.; Najarro, G.; Singh, S.; Lundy, D.; Nelson, T.; Trzeciak, S.W.; Jones, A.E.; et al. The Association of Near-Infrared Spectroscopy-Derived Tissue Oxygenation Measurements with Sepsis Syndromes, Organ Dysfunction and Mortality in Emergency Department Patients with Sepsis. Crit. Care 2011, 15, R223. [Google Scholar] [CrossRef] [Green Version]
- Donati, A.; Damiani, E.; Domizi, R.; Scorcella, C.; Carsetti, A.; Tondi, S.; Monaldi, V.; Adrario, E.; Romano, R.; Pelaia, P.; et al. Near-Infrared Spectroscopy for Assessing Tissue Oxygenation and Microvascular Reactivity in Critically Ill Patients: A Prospective Observational Study. Crit. Care 2016, 20, 311. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Backer, D.; Donadello, K.; Taccone, F.S.; Ospina-Tascon, G.; Salgado, D.; Vincent, J.-L. Microcirculatory Alterations: Potential Mechanisms and Implications for Therapy. Ann. Intensive Care 2011, 1, 27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kao, R.; Xenocostas, A.; Rui, T.; Yu, P.; Huang, W.; Rose, J.; Martin, C.M. Erythropoietin Improves Skeletal Muscle Microcirculation and Tissue Bioenergetics in a Mouse Sepsis Model. Crit. Care 2007, 11, R58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bateman, R.M.; Tokunaga, C.; Kareco, T.; Dorscheid, D.R.; Walley, K.R. Myocardial Hypoxia-Inducible HIF-1alpha, VEGF, and GLUT1 Gene Expression Is Associated with Microvascular and ICAM-1 Heterogeneity during Endotoxemia. Am. J. Physiol. Heart Circ. Physiol. 2007, 293, H448–H456. [Google Scholar] [CrossRef] [PubMed]
- Ince, C. Hemodynamic Coherence and the Rationale for Monitoring the Microcirculation. Crit. Care 2015, 19, S8. [Google Scholar] [CrossRef] [Green Version]
- Tachon, G.; Harrois, A.; Tanaka, S.; Kato, H.; Huet, O.; Pottecher, J.; Vicaut, E.; Duranteau, J. Microcirculatory Alterations in Traumatic Hemorrhagic Shock. Crit. Care Med. 2014, 42, 1433–1441. [Google Scholar] [CrossRef]
- Hutchings, S.D.; Naumann, D.N.; Hopkins, P.; Mellis, C.; Riozzi, P.; Sartini, S.; Mamuza, J.; Harris, T.; Midwinter, M.J.; Wendon, J. Microcirculatory Impairment Is Associated with Multiple Organ Dysfunction Following Traumatic Hemorrhagic Shock: The MICROSHOCK Study. Crit. Care Med. 2018, 46, e889–e896. [Google Scholar] [CrossRef]
- Naumann, D.N.; Mellis, C.; Smith, I.M.; Mamuza, J.; Skene, I.; Harris, T.; Midwinter, M.J.; Hutchings, S.D. Safety and Feasibility of Sublingual Microcirculation Assessment in the Emergency Department for Civilian and Military Patients with Traumatic Haemorrhagic Shock: A Prospective Cohort Study. BMJ Open 2016, 6, e014162. [Google Scholar] [CrossRef] [Green Version]
- Naumann, D.N.; Hazeldine, J.; Midwinter, M.J.; Hutchings, S.; Harrison, P. Poor Microcirculatory Flow Dynamics Are Associated with Endothelial Cell Damage and Glycocalyx Shedding after Traumatic Hemorrhagic Shock. J. Trauma-Inj. Infect. Crit. Care 2018, 84, 81–88. [Google Scholar] [CrossRef] [Green Version]
- De Backer, D.; Creteur, J.; Dubois, M.-J.; Sakr, Y.; Vincent, J.-L. Microvascular Alterations in Patients with Acute Severe Heart Failure and Cardiogenic Shock. Am. Heart J. 2004, 147, 91–99. [Google Scholar] [CrossRef]
- Fries, M.; Weil, M.H.; Chang, Y.-T.; Castillo, C.; Tang, W. Microcirculation during Cardiac Arrest and Resuscitation. Crit. Care Med. 2006, 34, S454–S457. [Google Scholar] [CrossRef]
- Wijntjens, G.W.; Fengler, K.; Fuernau, G.; Jung, C.; den Uil, C.; Akin, S.; van de Hoef, T.P.; Šerpytis, R.; Diletti, R.; Henriques, J.P.; et al. Prognostic Implications of Microcirculatory Perfusion versus Macrocirculatory Perfusion in Cardiogenic Shock: A Culprit-Shock Substudy. Eur. Heart J. Acute Cardiovasc. Care 2020, 9, 108–119. [Google Scholar] [CrossRef] [Green Version]
- Jung, C.; Fuernau, G.; Muench, P.; Desch, S.; Eitel, I.; Schuler, G.; Adams, V.; Figulla, H.R.; Thiele, H. Impairment of the Endothelial Glycocalyx in Cardiogenic Shock and Its Prognostic Relevance. Shock 2015, 43, 450–455. [Google Scholar] [CrossRef]
- Li, J.; Yu, Z.; Zeng, J.; Liu, Z.; Zhao, Z.; Zhang, Y.; Li, G. Circular RNA UBAP2 (Hsa_circ_0007367) Correlates with Microcirculatory Perfusion and Predicts Outcomes of Cardiogenic Shock Patients Undergoing Extracorporeal Membrane Oxygenation Support. Shock Augusta Ga 2022, 57, 200–210. [Google Scholar] [CrossRef]
- Akin, S.; Dos Reis Miranda, D.; Caliskan, K.; Soliman, O.I.; Guven, G.; Struijs, A.; van Thiel, R.J.; Jewbali, L.S.; Lima, A.; Gommers, D.; et al. Functional Evaluation of Sublingual Microcirculation Indicates Successful Weaning from VA-ECMO in Cardiogenic Shock. Crit. Care 2017, 21, 265. [Google Scholar] [CrossRef] [Green Version]
- Dekker, N.A.M.; Veerhoek, D.; Koning, N.J.; van Leeuwen, A.L.; Elbers, P.W.G.; van den Brom, C.E. Postoperative Microcirculatory Perfusion and Endothelial Glycocalyx Shedding Following Cardiac Surgery with Cardiopulmonary Bypass. Anaesthesia 2019, 74, 609–618. [Google Scholar] [CrossRef] [Green Version]
- Wu, Q.; Gao, W.; Zhou, J.; He, G.; Ye, J.-X.; Fang, F.-Q.; Luo, J.; Wang, M.; Xu, H.; Wang, W. Correlation between Acute Degradation of the Endothelial Glycocalyx and Microcirculation Dysfunction during Cardiopulmonary Bypass in Cardiac Surgery. Microvasc. Res. 2019, 124, 37–42. [Google Scholar] [CrossRef]
- Dekker, N.A.M.; Veerhoek, D.; van Leeuwen, A.L.I.; Alexander, B.; Vonk, A.B.A.; van den Brom, C.E.; Boer, C. Microvascular Alterations During Cardiac Surgery Using a Heparin or Phosphorylcholine-Coated Circuit. J. Cardiothorac. Vasc. Anesth. 2020, 34, 912–919. [Google Scholar] [CrossRef] [Green Version]
- Giantsos-Adams, K.M.; Koo, A.J.-A.; Song, S.; Sakai, J.; Sankaran, J.; Shin, J.H.; Garcia-Cardena, G.; Dewey, C.F. Heparan Sulfate Regrowth Profiles Under Laminar Shear Flow Following Enzymatic Degradation. Cell. Mol. Bioeng. 2013, 6, 160–174. [Google Scholar] [CrossRef] [Green Version]
- Koo, A.; Dewey, C.F.; García-Cardeña, G. Hemodynamic Shear Stress Characteristic of Atherosclerosis-Resistant Regions Promotes Glycocalyx Formation in Cultured Endothelial Cells. Am. J. Physiol. Cell Physiol. 2013, 304, C137–C146. [Google Scholar] [CrossRef] [Green Version]
- Potter, D.R.; Jiang, J.; Damiano, E.R. The Recovery Time Course of the Endothelial Cell Glycocalyx In Vivo and Its Implications In Vitro. Circ. Res. 2009, 104, 1318–1325. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Siner, J.M.; Bhandari, V.; Engle, K.M.; Elias, J.A.; Siegel, M.D. Elevated Serum Angiopoietin 2 Levels Are Associated with Increased Mortality in Sepsis. Shock Augusta Ga 2009, 31, 348–353. [Google Scholar] [CrossRef] [PubMed]
- Belousoviene, E.; Kiudulaite, I.; Pilvinis, V.; Pranskunas, A. Links between Endothelial Glycocalyx Changes and Microcirculatory Parameters in Septic Patients. Life 2021, 11, 790. [Google Scholar] [CrossRef] [PubMed]
- Georger, J.-F.; Hamzaoui, O.; Chaari, A.; Maizel, J.; Richard, C.; Teboul, J.-L. Restoring Arterial Pressure with Norepinephrine Improves Muscle Tissue Oxygenation Assessed by Near-Infrared Spectroscopy in Severely Hypotensive Septic Patients. Intensive Care Med. 2010, 36, 1882–1889. [Google Scholar] [CrossRef]
- Dünser, M.W.; Takala, J.; Ulmer, H.; Mayr, V.D.; Luckner, G.; Jochberger, S.; Daudel, F.; Lepper, P.; Hasibeder, W.R.; Jakob, S.M. Arterial Blood Pressure during Early Sepsis and Outcome. Intensive Care Med. 2009, 35, 1225–1233. [Google Scholar] [CrossRef] [Green Version]
- Trzeciak, S.; McCoy, J.V.; Dellinger, R.P.; Arnold, R.C.; Rizzuto, M.; Abate, N.L.; Shapiro, N.I.; Parrillo, J.E.; Hollenberg, S.M. Early Increases in Microcirculatory Perfusion During Protocol-Directed Resuscitation Are Associated with Reduced Multi-Organ Failure at 24 Hours in Patients with Sepsis. Intensive Care Med. 2008, 34, 2210–2217. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dubin, A.; Pozo, M.O.; Casabella, C.A.; Pálizas, F.; Murias, G.; Moseinco, M.C.; Kanoore Edul, V.S.; Pálizas, F.; Estenssoro, E.; Ince, C. Increasing Arterial Blood Pressure with Norepinephrine Does Not Improve Microcirculatory Blood Flow: A Prospective Study. Crit. Care 2009, 13, R92. [Google Scholar] [CrossRef] [Green Version]
- Leone, M.; Asfar, P.; Radermacher, P.; Vincent, J.-L.; Martin, C. Optimizing Mean Arterial Pressure in Septic Shock: A Critical Reappraisal of the Literature. Crit. Care 2015, 19, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Leone, M.; Blidi, S.; Antonini, F.; Meyssignac, B.; Bordon, S.; Garcin, F.; Charvet, A.; Blasco, V.; Albanèse, J.; Martin, C. Oxygen Tissue Saturation Is Lower in Nonsurvivors than in Survivors after Early Resuscitation of Septic Shock. Anesthesiology 2009, 111, 366–371. [Google Scholar] [CrossRef] [Green Version]
- Ince, C.; Guerci, P. Why and When the Microcirculation Becomes Disassociated from the Macrocirculation. Intensive Care Med. 2016, 42, 1645–1646. [Google Scholar] [CrossRef]
- Marshall, J.C. Why Have Clinical Trials in Sepsis Failed? Trends Mol. Med. 2014, 20, 195–203. [Google Scholar] [CrossRef]
- Sinha, P.; Calfee, C.S. Phenotypes in ARDS: Moving Towards Precision Medicine. Curr. Opin. Crit. Care 2019, 25, 12–20. [Google Scholar] [CrossRef]
- Papazian, L.; Forel, J.-M.; Gacouin, A.; Penot-Ragon, C.; Perrin, G.; Loundou, A.; Jaber, S.; Arnal, J.-M.; Perez, D.; Seghboyan, J.-M.; et al. Neuromuscular Blockers in Early Acute Respiratory Distress Syndrome. N. Engl. J. Med. 2010, 363, 1107–1116. [Google Scholar] [CrossRef] [Green Version]
- Guérin, C.; Reignier, J.; Richard, J.-C.; Beuret, P.; Gacouin, A.; Boulain, T.; Mercier, E.; Badet, M.; Mercat, A.; Baudin, O.; et al. Prone Positioning in Severe Acute Respiratory Distress Syndrome. N. Engl. J. Med. 2013, 368, 2159–2168. [Google Scholar] [CrossRef]
- den Uil, C.A.; Lagrand, W.K.; van der Ent, M.; Jewbali, L.S.D.; Cheng, J.M.; Spronk, P.E.; Simoons, M.L. Impaired Microcirculation Predicts Poor Outcome of Patients with Acute Myocardial Infarction Complicated by Cardiogenic Shock. Eur. Heart J. 2010, 31, 3032–3039. [Google Scholar] [CrossRef] [Green Version]
- Holley, A.D.; Dulhunty, J.; Udy, A.; Midwinter, M.; Lukin, B.; Stuart, J.; Boots, R.; Lassig-Smith, M.; Holley, R.B.; Paratz, J.; et al. Early Sequential Microcirculation Assessment in Shocked Patients as a Predictor of Outcome: A Prospective Observational Cohort Study. Shock Augusta Ga 2021, 55, 581–586. [Google Scholar] [CrossRef]
- Sakr, Y.; Chierego, M.; Piagnerelli, M.; Verdant, C.; Dubois, M.-J.; Koch, M.; Creteur, J.; Gullo, A.; Vincent, J.-L.; De Backer, D. Microvascular Response to Red Blood Cell Transfusion in Patients with Severe Sepsis. Crit. Care Med. 2007, 35, 1639–1644. [Google Scholar] [CrossRef]
- Pranskunas, A.; Tamošuitis, T.; Balciuniene, N.; Damanskyte, D.; Šneider, E.; Vitkauskiene, A.; Širvinskas, E.; Širvinskas, E.; Pilvinis, V.; Boerma, E.C. Alterations of Conjunctival Glycocalyx and Microcirculation in Non-Septic Critically Ill Patients. Microvasc. Res. 2018, 118, 44–48. [Google Scholar] [CrossRef]
- Rovas, A.; Seidel, L.M.; Vink, H.; Pohlkötter, T.; Pavenstädt, H.; Ertmer, C.; Hessler, M.; Kümpers, P. Association of Sublingual Microcirculation Parameters and Endothelial Glycocalyx Dimensions in Resuscitated Sepsis. Crit. Care 2019, 23, 260. [Google Scholar] [CrossRef] [Green Version]
- ProCESS Investigators; Yealy, D.M.; Kellum, J.A.; Huang, D.T.; Barnato, A.E.; Weissfeld, L.A.; Pike, F.; Terndrup, T.; Wang, H.E.; Hou, P.C.; et al. A Randomized Trial of Protocol-Based Care for Early Septic Shock. N. Engl. J. Med. 2014, 370, 1683–1693. [Google Scholar] [CrossRef] [Green Version]
- Fernández-Sarmiento, J.; Molina, C.F.; Salazar-Pelaez, L.M.; Flórez, S.; Alarcón-Forero, L.C.; Sarta, M.; Hernández-Sarmiento, R.; Villar, J.C. Biomarkers of Glycocalyx Injury and Endothelial Activation Are Associated with Clinical Outcomes in Patients with Sepsis: A Systematic Review and Meta-Analysis. J. Intensive Care Med. 2022, 2022, 8850666221109186. [Google Scholar] [CrossRef]
- Beurskens, D.M.; Bol, M.E.; Delhaas, T.; van de Poll, M.C.; Reutelingsperger, C.P.; Nicolaes, G.A.; Sels, J.-W.E. Decreased Endothelial Glycocalyx Thickness Is an Early Predictor of Mortality in Sepsis. Anaesth. Intensive Care 2020, 48, 221–228. [Google Scholar] [CrossRef] [PubMed]
- Thorevska, N.; Sabahi, R.; Upadya, A.; Manthous, C.; Amoateng-Adjepong, Y. Microalbuminuria in Critically Ill Medical Patients: Prevalence, Predictors, and Prognostic Significance. Crit. Care Med. 2003, 31, 1075–1081. [Google Scholar] [CrossRef] [PubMed]
- Honarmand, A.; Safavi, M.; Baghery, K.; Momayezi, A. The Association of Microalbuminuria and Duration of Mechanical Ventilation in Critically Ill Trauma Patients. Turk. J. Trauma Emerg. Surg. 2009, 15, 12–18. [Google Scholar]
- Rinaldi, S.; Adembri, C.; Grechi, S.; De Gaudio, A.R. Low-Dose Hydrocortisone during Severe Sepsis: Effects on Microalbuminuria. Crit. Care Med. 2006, 34, 2334–2339. [Google Scholar] [CrossRef] [PubMed]
- Evans, L.; Rhodes, A.; Alhazzani, W.; Antonelli, M.; Coopersmith, C.M.; French, C.; Machado, F.R.; Mcintyre, L.; Ostermann, M.; Prescott, H.C.; et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock. Intensive Care Med. 2021, 47, 1181–1247. [Google Scholar] [CrossRef]
- Rivers, E.; Nguyen, B.; Havstad, S.; Ressler, J.; Muzzin, A.; Knoblich, B.; Peterson, E.; Tomlanovich, M. Early Goal-Directed Therapy Collaborative Group Early Goal-Directed Therapy in the Treatment of Severe Sepsis and Septic Shock. N. Engl. J. Med. 2001, 345, 1368–1377. [Google Scholar] [CrossRef] [Green Version]
- Bozza, F.A.; Carnevale, R.; Japiassú, A.M.; Castro-Faria-Neto, H.C.; Angus, D.C.; Salluh, J.I.F. Early Fluid Resuscitation in Sepsis: Evidence and Perspectives. Shock Augusta Ga 2010, 34, 40–43. [Google Scholar] [CrossRef]
- Hippensteel, J.A.; Uchimido, R.; Tyler, P.D.; Burke, R.C.; Han, X.; Zhang, F.; McMurtry, S.A.; Colbert, J.F.; Lindsell, C.J. Intravenous Fluid Resuscitation Is Associated with Septic Endothelial Glycocalyx Degradation. Crit. Care 2019, 23, 259. [Google Scholar] [CrossRef] [Green Version]
- Inkinen, N.; Pettilä, V.; Lakkisto, P.; Kuitunen, A.; Jukarainen, S.; Bendel, S.; Inkinen, O.; Ala-Kokko, T.; Vaara, S.T. Association of Endothelial and Glycocalyx Injury Biomarkers with Fluid Administration, Development of Acute Kidney Injury, and 90-Day Mortality: Data from the FINNAKI Observational Study. Ann. Intensive Care 2019, 9, 103. [Google Scholar] [CrossRef]
- Finfer, S.; Micallef, S.; Hammond, N.; Navarra, L.; Bellomo, R.; Billot, L.; Delaney, A.; Gallagher, M.; Gattas, D.; Li, Q.; et al. Balanced Multielectrolyte Solution versus Saline in Critically Ill Adults. N. Engl. J. Med. 2022, 386, 815–826. [Google Scholar] [CrossRef]
- Silversides, J.A.; Major, E.; Ferguson, A.J.; Mann, E.E.; McAuley, D.F.; Marshall, J.C.; Blackwood, B.; Fan, E. Conservative Fluid Management or Deresuscitation for Patients with Sepsis or Acute Respiratory Distress Syndrome Following the Resuscitation Phase of Critical Illness: A Systematic Review and Meta-Analysis. Intensive Care Med. 2017, 43, 155–170. [Google Scholar] [CrossRef] [Green Version]
- Silversides, J.A.; Perner, A.; Malbrain, M.L.N.G. Liberal versus Restrictive Fluid Therapy in Critically Ill Patients. Intensive Care Med. 2019, 45, 1440–1442. [Google Scholar] [CrossRef] [Green Version]
- Meyhoff, T.S.; Hjortrup, P.B.; Møller, M.H.; Wetterslev, J.; Lange, T.; Kjaer, M.-B.N.; Jonsson, A.B.; Hjortsø, C.J.S.; Cronhjort, M.; Laake, J.H.; et al. Conservative vs Liberal Fluid Therapy in Septic Shock (CLASSIC) Trial-Protocol and Statistical Analysis Plan. Acta Anaesthesiol. Scand. 2019, 63, 1262–1271. [Google Scholar] [CrossRef] [Green Version]
- Woodcock, T.E.; Woodcock, T.M. Revised Starling Equation and the Glycocalyx Model of Transvascular Fluid Exchange: An Improved Paradigm for Prescribing Intravenous Fluid Therapy. Br. J. Anaesth. 2012, 108, 384–394. [Google Scholar] [CrossRef]
- Uchimido, R.; Schmidt, E.P.; Shapiro, N.I. The Glycocalyx: A Novel Diagnostic and Therapeutic Target in Sepsis. Crit. Care 2019, 23, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Brandstrup, B.; Tønnesen, H.; Beier-Holgersen, R.; Hjortsø, E.; Ørding, H.; Lindorff-Larsen, K.; Rasmussen, M.S.; Lanng, C.; Wallin, L.; Iversen, L.H.; et al. Effects of Intravenous Fluid Restriction on Postoperative Complications: Comparison of Two Perioperative Fluid Regimens: A Randomized Assessor-Blinded Multicenter Trial. Ann. Surg. 2003, 238, 641–648. [Google Scholar] [CrossRef]
- Lobo, D.N.; Bostock, K.A.; Neal, K.R.; Perkins, A.C.; Rowlands, B.J.; Allison, S.P. Effect of Salt and Water Balance on Recovery of Gastrointestinal Function after Elective Colonic Resection: A Randomised Controlled Trial. Lancet 2002, 359, 1812–1818. [Google Scholar] [CrossRef]
- Tigabu, B.M.; Davari, M.; Kebriaeezadeh, A.; Mojtahedzadeh, M. Fluid Volume, Fluid Balance and Patient Outcome in Severe Sepsis and Septic Shock: A Systematic Review. J. Crit. Care 2018, 48, 153–159. [Google Scholar] [CrossRef]
- Boyd, J.H.; Forbes, J.; Nakada, T.; Walley, K.R.; Russell, J.A. Fluid Resuscitation in Septic Shock: A Positive Fluid Balance and Elevated Central Venous Pressure Are Associated with Increased Mortality. Crit. Care Med. 2011, 39, 259–265. [Google Scholar] [CrossRef]
- Saoraya, J.; Wongsamita, L.; Srisawat, N.; Musikatavorn, K. The Effects of a Limited Infusion Rate of Fluid in the Early Resuscitation of Sepsis on Glycocalyx Shedding Measured by Plasma Syndecan-1: A Randomized Controlled Trial. J. Intensive Care 2021, 9, 1. [Google Scholar] [CrossRef] [PubMed]
- Chappell, D.; Bruegger, D.; Potzel, J.; Jacob, M.; Brettner, F.; Vogeser, M.; Conzen, P.; Becker, B.F.; Rehm, M. Hypervolemia Increases Release of Atrial Natriuretic Peptide and Shedding of the Endothelial Glycocalyx. Crit. Care 2014, 18, 538. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Margraf, A.; Herter, J.M.; Kühne, K.; Stadtmann, A.; Ermert, T.; Wenk, M.; Meersch, M.; Van Aken, H.; Zarbock, A. 6% Hydroxyethyl Starch (HES 130/0.4) Diminishes Glycocalyx Degradation and Decreases Vascular Permeability during Systemic and Pulmonary Inflammation in Mice. Crit. Care 2018, 22, 111. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- EMA PRAC Recommends Suspending Hydroxyethyl-Starch Solutions for Infusion from the Market. Available online: https://www.ema.europa.eu/en/news/prac-recommends-suspending-hydroxyethyl-starch-solutions-infusion-market-0 (accessed on 4 May 2022).
- Hahn, R.G. Do Intensivists Need to Care About the Revised Starling Principle. In Annual Update in Intensive Care and Emergency Medicine; Springer: Cham, Switzerland, 2020; pp. 137–144. [Google Scholar] [CrossRef]
- Torres, L.N.; Chung, K.K.; Salgado, C.L.; Dubick, M.A.; Torres Filho, I.P. Low-Volume Resuscitation with Normal Saline Is Associated with Microvascular Endothelial Dysfunction after Hemorrhage in Rats, Compared to Colloids and Balanced Crystalloids. Crit. Care 2017, 21, 160. [Google Scholar] [CrossRef] [PubMed]
- Milford, E.M.; Reade, M.C. Resuscitation Fluid Choices to Preserve the Endothelial Glycocalyx. Crit. Care 2019, 23, 77. [Google Scholar] [CrossRef] [Green Version]
- Yanase, F.; Yanase, F.; Tosif, S.; Churilov, L.; Yee, K.; Bellomo, R.; Gunn, K.; Kim, C.; Krizhanovskii, C.; Hahn, R.G.; et al. A Randomized, Multicenter, Open-Label, Blinded End Point, Phase 2, Feasibility, Efficacy, and Safety Trial of Preoperative Microvascular Protection in Patients Undergoing Major Abdominal Surgery. Anesth. Analg. 2021, 133, 1036–1047. [Google Scholar] [CrossRef]
- Adamson, R.H.; Clark, J.F.; Radeva, M.; Kheirolomoom, A.; Ferrara, K.W.; Curry, F.R.E. Albumin Modulates S1P Delivery from Red Blood Cells in Perfused Microvessels: Mechanism of the Protein Effect. Am. J. Physiol.-Heart Circ. Physiol. 2014, 306, 2013. [Google Scholar] [CrossRef] [Green Version]
- Diebel, L.N.; Liberati, D.M.; Hla, T.; Swendeman, S.L. Plasma Components to Protect the Endothelial Barrier after Shock: Arole for Sphingosine 1-Phosphate. Surgery 2021, 171, 825–832. [Google Scholar] [CrossRef]
- Dexamethasone in Hospitalized Patients with COVID-19. N. Engl. J. Med. 2021, 384, 693–704. [CrossRef]
- Yu, Z.; Ouyang, J.-P.; Li, Y. Dexamethasone Attenuated Endotoxin-Induced Acute Lung Injury through Inhibiting Expression of Inducible Nitric Oxide Synthase. Clin. Hemorheol. Microcirc. 2009, 41, 117–125. [Google Scholar] [CrossRef]
- Gao, S.; Zhang, Y.; Zhang, S.; Liang, Z.-Y.; Yu, W.-Q.; Yu, W.-Q.; Liang, T.-B. The Hydrocortisone Protection of Glycocalyx on the Intestinal Capillary Endothelium During Severe Acute Pancreatitis. Shock 2015, 43, 512–517. [Google Scholar] [CrossRef]
- Chappell, D.; Jacob, M.; Hofmann-Kiefer, K.; Bruegger, D.; Rehm, M.; Conzen, P.; Welsch, U.; Becker, B.F. Hydrocortisone Preserves the Vascular Barrier by Protecting the Endothelial Glycocalyx. Anesthesiology 2007, 107, 776–784. [Google Scholar] [CrossRef] [Green Version]
- Pillinger, N.; Kam, P. Endothelial Glycocalyx: Basic Science and Clinical Implications. Anaesth. Intensive Care 2017, 45, 295–307. [Google Scholar] [CrossRef] [Green Version]
- Newton, C.; Ran, G.; Xie, Y.-X.; Bilko, D.; Burgoyne, C.; Adams, I.P.; Abidia, A.; McCollum, P.T.; Atkin, S.L. Statin-Induced Apoptosis of Vascular Endothelial Cells Is Blocked by Dexamethasone. J. Endocrinol. 2002, 174, 7–16. [Google Scholar] [CrossRef]
- Rongcai, J.; Jianning, Z.; Wang, D.; Dong, W.; Fan, Y.-S.; Wang, B.; Xin, X.; Xu, X.; Dong, W.; Xin, X.; et al. Atorvastatin Combined with Low-Dose Dexamethasone for Vascular Endothelial Cell Dysfunction Induced by Chronic Subdural Hematoma. Neural Regen. Res. 2021, 16, 523–530. [Google Scholar] [CrossRef]
- Kim, W.-Y.; Kweon, O.J.; Cha, M.J.; Baek, M.S.; Choi, S.-H. Dexamethasone May Improve Severe COVID-19 via Ameliorating Endothelial Injury and Inflammation: A Preliminary Pilot Study. PLoS ONE 2021, 16, e0254167. [Google Scholar] [CrossRef]
- Becker, B.F.; Jacob, M.; Leipert, S.; Salmon, A.H.J.; Chappell, D. Degradation of the Endothelial Glycocalyx in Clinical Settings: Searching for the Sheddases. Br. J. Clin. Pharmacol. 2015, 80, 389–402. [Google Scholar] [CrossRef]
- Allingstrup, M.; Wetterslev, J.; Ravn, F.B.; Møller, A.M.; Afshari, A. Antithrombin III for Critically Ill Patients: A Systematic Review with Meta-Analysis and Trial Sequential Analysis. Intensive Care Med. 2016, 42, 505–520. [Google Scholar] [CrossRef] [Green Version]
- Iba, T.; Levy, J.H.; Aihara, K.; Kadota, K.; Tanaka, H.; Sato, K.; Nagaoka, I. Newly Developed Recombinant Antithrombin Protects the Endothelial Glycocalyx in an Endotoxin-Induced Rat Model of Sepsis. Int. J. Mol. Sci. 2020, 22, 176. [Google Scholar] [CrossRef]
- Spiess, B.D. Heparin: Effects upon the Glycocalyx and Endothelial Cells. J. Extra. Corpor. Technol. 2017, 49, 192–197. [Google Scholar]
- Potje, S.R.; Costa, T.J.; Fraga-Silva, T.F.C.; Martins, R.B.; Benatti, M.N.; Almado, C.E.L.; de Sá, K.S.G.; Bonato, V.L.D.; Arruda, E.; Louzada-Junior, P.; et al. Heparin Prevents in Vitro Glycocalyx Shedding Induced by Plasma from COVID-19 Patients. Life Sci. 2021, 276, 119376. [Google Scholar] [CrossRef] [PubMed]
- Research, C. for D.E. and Enrichment Strategies for Clinical Trials to Support Approval of Human Drugs and Biological Products. Available online: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/enrichment-strategies-clinical-trials-support-approval-human-drugs-and-biological-products (accessed on 23 May 2022).
- White House Precision Medicine Initiative. Available online: https://obamawhitehouse.archives.gov/node/333101 (accessed on 23 May 2022).
- Stanski, N.L.; Wong, H.R. Prognostic and Predictive Enrichment in Sepsis. Nat. Rev. Nephrol. 2020, 16, 20–31. [Google Scholar] [CrossRef] [PubMed]
- Song, J.W.; Zullo, J.A.; Liveris, D.; Dragovich, M.; Zhang, X.F.; Goligorsky, M.S. Therapeutic Restoration of Endothelial Glycocalyx in Sepsis. J. Pharmacol. Exp. Ther. 2017, 361, 115–121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Straat, M.; Müller, M.C.; Meijers, J.C.; Arbous, M.S.; de Man, A.M.S.; Beurskens, C.J.; Vroom, M.B.; Juffermans, N.P. Effect of Transfusion of Fresh Frozen Plasma on Parameters of Endothelial Condition and Inflammatory Status in Non-Bleeding Critically Ill Patients: A Prospective Substudy of a Randomized Trial. Crit. Care 2015, 19, 163. [Google Scholar] [CrossRef] [Green Version]
- Wang, G.; Zhang, H.; Liu, D.; Wang, X. Resuscitation Fluids as Drugs: Targeting the Endothelial Glycocalyx. Chin. Med. J. 2022, 135, 137–144. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cusack, R.; Leone, M.; Rodriguez, A.H.; Martin-Loeches, I. Endothelial Damage and the Microcirculation in Critical Illness. Biomedicines 2022, 10, 3150. https://doi.org/10.3390/biomedicines10123150
Cusack R, Leone M, Rodriguez AH, Martin-Loeches I. Endothelial Damage and the Microcirculation in Critical Illness. Biomedicines. 2022; 10(12):3150. https://doi.org/10.3390/biomedicines10123150
Chicago/Turabian StyleCusack, Rachael, Marc Leone, Alejandro H. Rodriguez, and Ignacio Martin-Loeches. 2022. "Endothelial Damage and the Microcirculation in Critical Illness" Biomedicines 10, no. 12: 3150. https://doi.org/10.3390/biomedicines10123150




