Effect of a Novel E3 Probiotics Formula on the Gut Microbiome in Atopic Dermatitis Patients: A Pilot Study
Abstract
:1. Introduction
2. Materials and Methods
3. Results
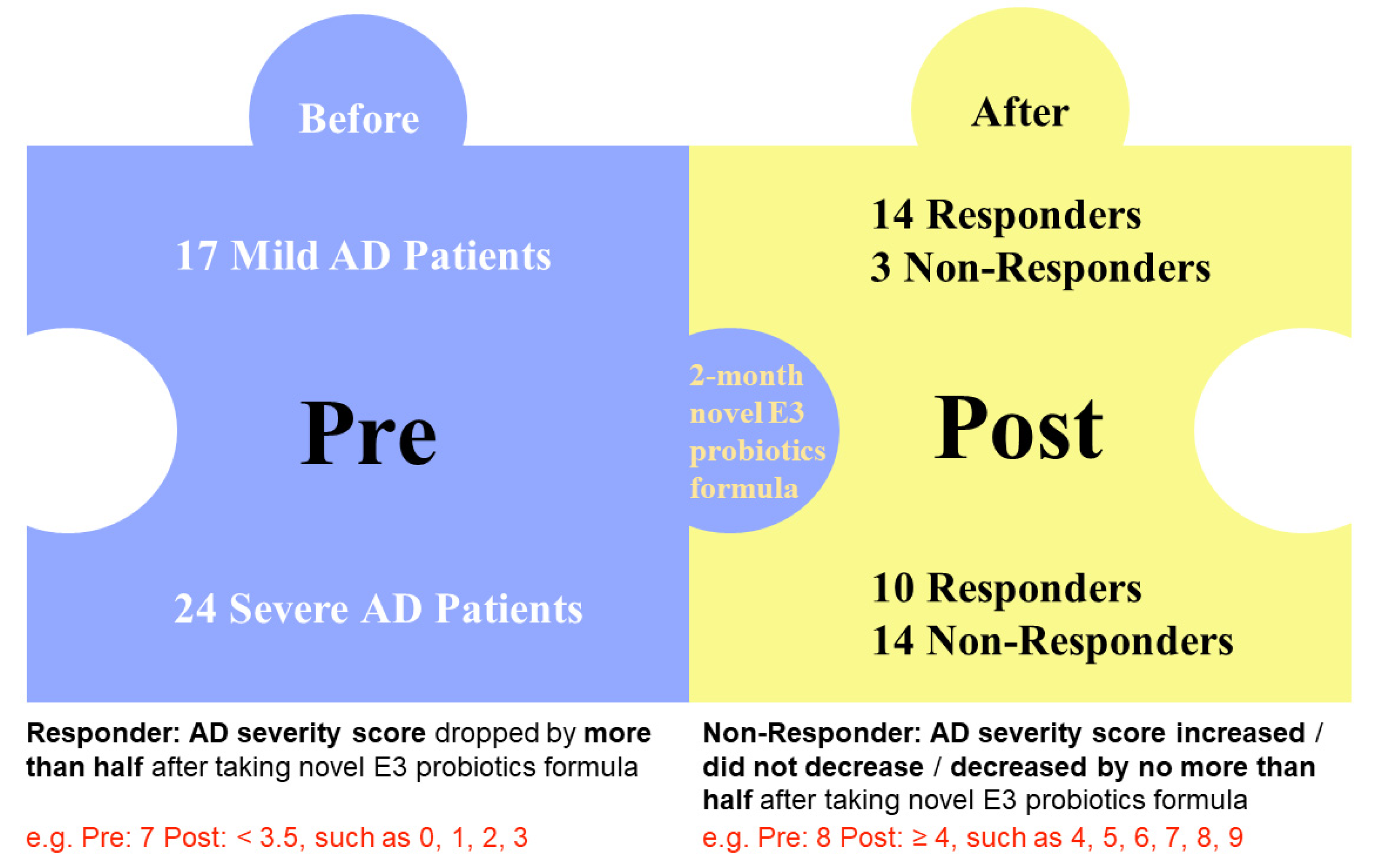
3.1. Study Population
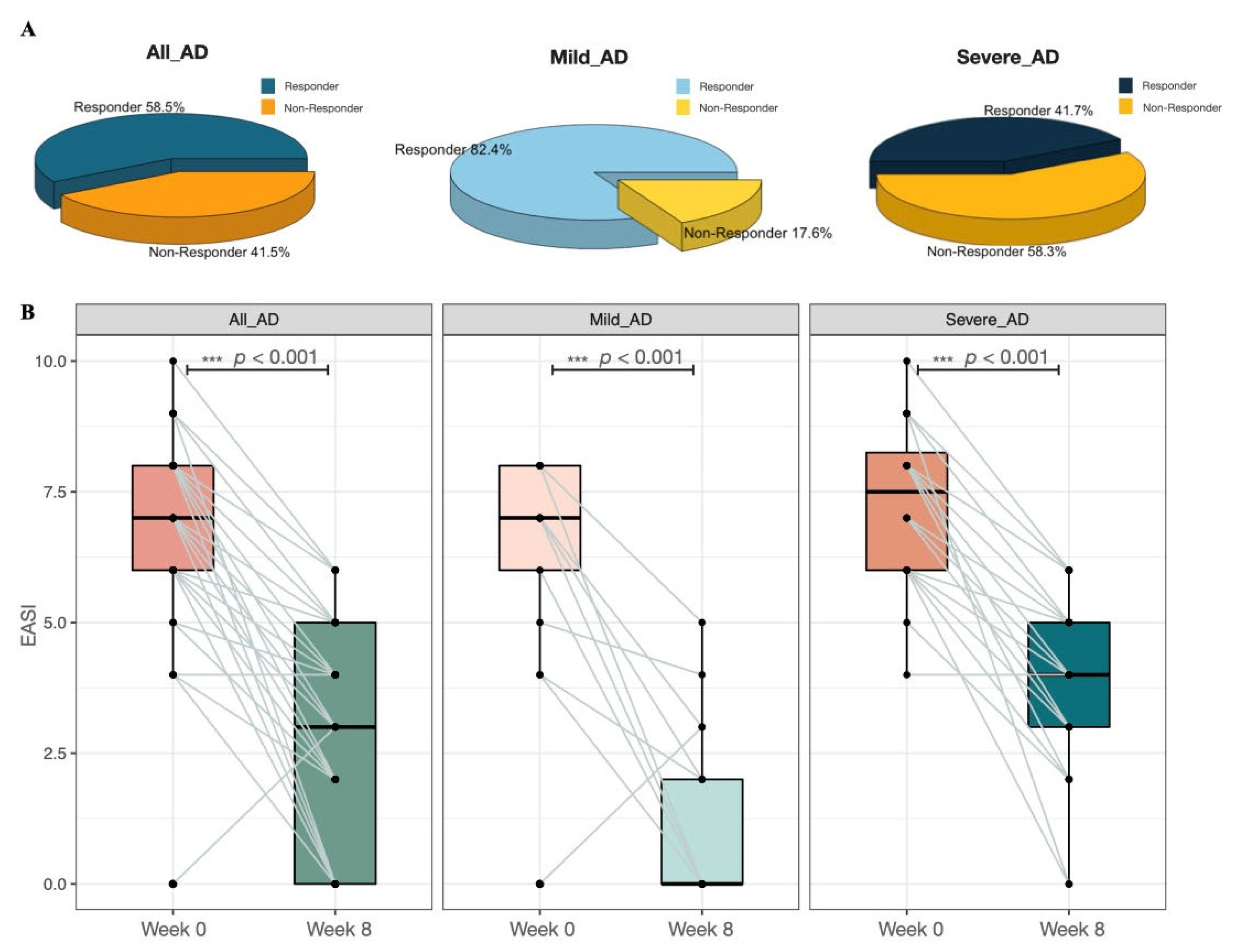
3.2. Probiotic Mixture Significantly Ameliorates AD Severity
3.3. Probiotic Mixture Improves the Diversity of Gut Microbiome in AD Patients
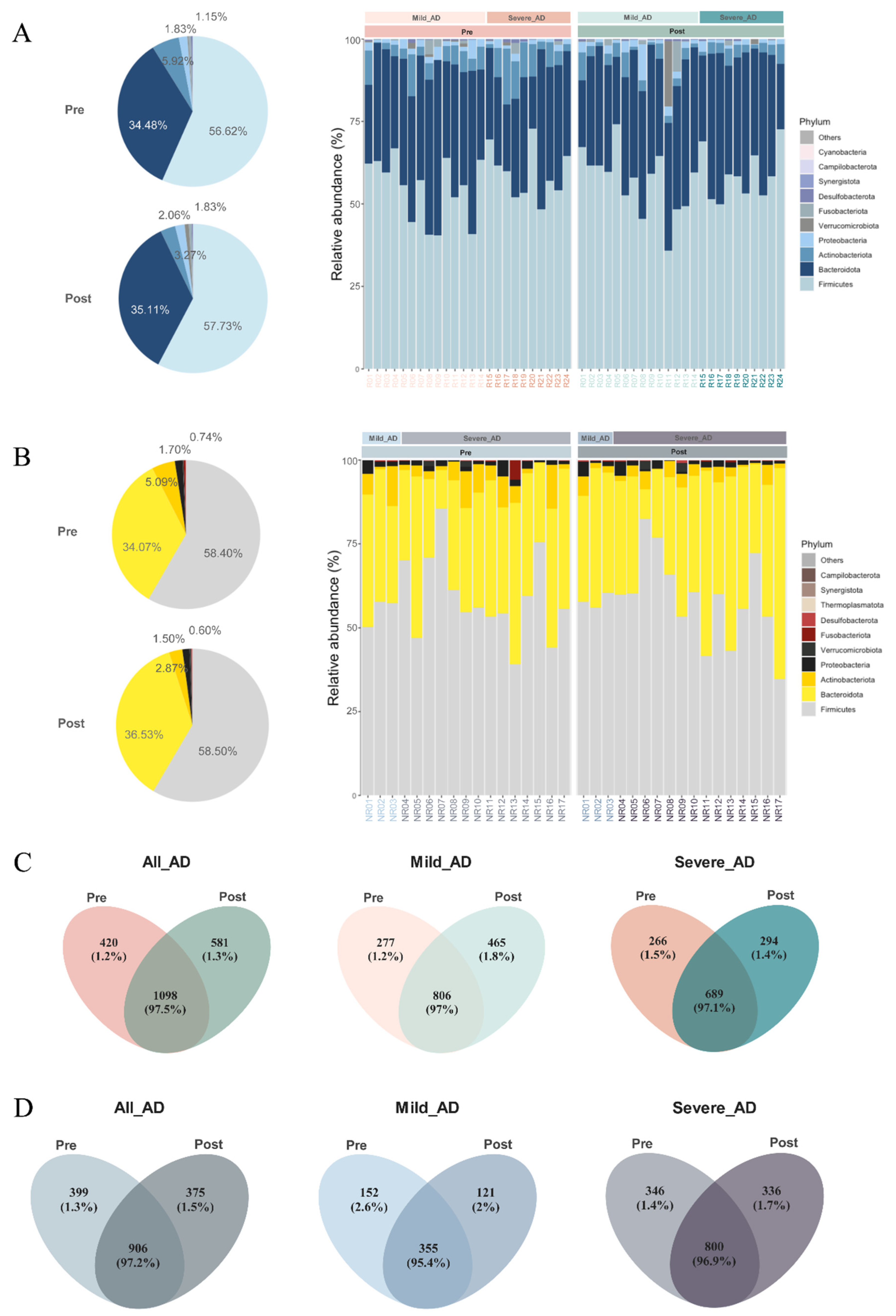
3.4. Gut Microbiome Profiling
3.5. The Relative Abundance of Lactobacillus Increased Significantly after Oral Administration of Probiotic Mixture
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lopez Carrera, Y.I.; al Hammadi, A.; Huang, Y.H.; Llamado, L.J.; Mahgoub, E.; Tallman, A.M. Epidemiology, Diagnosis, and Treatment of Atopic Dermatitis in the Developing Countries of Asia, Africa, Latin America, and the Middle East: A Review. Dermatol. Ther. 2019, 9, 685–705. [Google Scholar] [CrossRef] [Green Version]
- Kaufman, B.P.; Guttman-Yassky, E.; Alexis, A.F. Atopic Dermatitis in Diverse Racial and Ethnic Groups-Variations in Epidemiology, Genetics, Clinical Presentation and Treatment. Exp. Dermatol. 2018, 27, 340–357. [Google Scholar] [CrossRef] [Green Version]
- Mei-Yen Yong, A.; Tay, Y.K. Atopic Dermatitis: Racial and Ethnic Differences. Dermatol. Clin. 2017, 35, 395–402. [Google Scholar] [CrossRef]
- Flohr, C.; Mann, J. New Insights into the Epidemiology of Childhood Atopic Dermatitis. Allergy 2014, 69, 3–16. [Google Scholar] [CrossRef]
- Deckers, I.A.G.; McLean, S.; Linssen, S.; Mommers, M.; van Schayck, C.P.; Sheikh, A. Investigating International Time Trends in the Incidence and Prevalence of Atopic Eczema 1990–2010: A Systematic Review of Epidemiological Studies. PLoS ONE 2012, 7, e39803. [Google Scholar] [CrossRef] [Green Version]
- Verboom, P.; Hakkaart-Van Roijen, L.; Sturkenboom, M.; de Zeeuw, R.; Menke, H.; Rutten, F. The Cost of Atopic Dermatitis in the Netherlands: An International Comparison. Br. J. Dermatol. 2002, 147, 716–724. [Google Scholar] [CrossRef]
- Noda, S.; Suárez-Fariñas, M.; Ungar, B.; Kim, S.J.; de Guzman Strong, C.; Xu, H.; Peng, X.; Estrada, Y.D.; Nakajima, S.; Honda, T.; et al. The Asian Atopic Dermatitis Phenotype Combines Features of Atopic Dermatitis and Psoriasis with Increased TH17 Polarization. J. Allergy Clin. Immunol. 2015, 136, 1254–1264. [Google Scholar] [CrossRef]
- David Boothe, W.; Tarbox, J.A.; Tarbox, M.B. Atopic Dermatitis: Pathophysiology. Adv. Exp. Med. Biol. 2017, 1027, 21–37. [Google Scholar] [CrossRef]
- Barnes, E.M.; Carter, E.L.; Lewis, J.D. Predicting Microbiome Function Across Space Is Confounded by Strain-Level Differences and Functional Redundancy Across Taxa. Front. Microbiol. 2020, 11, 101. [Google Scholar] [CrossRef] [Green Version]
- Sun, S.; Chang, G.; Zhang, L. The Prevention Effect of Probiotics against Eczema in Children: An Update Systematic Review and Meta-Analysis. J. Dermatol. Treat. 2022, 33, 1844–1854. [Google Scholar] [CrossRef]
- Ambrożej, D.; Kunkiel, K.; Dumycz, K.; Feleszko, W. The Use of Probiotics and Bacteria-Derived Preparations in Topical Treatment of Atopic Dermatitis-A Systematic Review. J. Allergy Clin. Immunol. Pract. 2021, 9, 570–575.e2. [Google Scholar] [CrossRef]
- Reynolds, G.; Vegh, P.; Fletcher, J.; Poyner, E.F.M.; Stephenson, E.; Goh, I.; Botting, R.A.; Huang, N.; Olabi, B.; Dubois, A.; et al. Developmental Cell Programs Are Co-Opted in Inflammatory Skin Disease. Science 2021, 371, eaba6500. [Google Scholar] [CrossRef]
- Williams, H.C.; Grindlay, D.J.C. What’s New in Atopic Eczema? An Analysis of Systematic Reviews Published in 2007 and 2008. Part 1. Definitions, Causes and Consequences of Eczema. Clin. Exp. Dermatol. 2010, 35, 12–15. [Google Scholar] [CrossRef]
- On, H.R.; Lee, S.E.; Kim, S.E.; Hong, W.J.; Kim, H.J.; Nomura, T.; Suzuki, S.; Shimizu, H.; Kim, S.C. Filaggrin Mutation in Korean Patients with Atopic Dermatitis. Yonsei Med. J. 2017, 58, 395–400. [Google Scholar] [CrossRef]
- Hassani, B.; Isaian, A.; Shariat, M.; Mollanoori, H.; Sotoudeh, S.; Babaei, V.; Ziaali, A.; Teimourian, S. Filaggrin Gene Polymorphisms in Iranian Ichthyosis Vulgaris and Atopic Dermatitis Patients. Int. J. Dermatol. 2018, 57, 1485–1491. [Google Scholar] [CrossRef]
- Rather, I.A.; Bajpai, V.K.; Kumar, S.; Lim, J.; Paek, W.K.; Park, Y.H. Probiotics and Atopic Dermatitis: An Overview. Front. Microbiol. 2016, 7, 507. [Google Scholar] [CrossRef] [Green Version]
- Thomas, C.L.; Fernández-Peñas, P. The Microbiome and Atopic Eczema: More than Skin Deep. Australas. J. Dermatol. 2017, 58, 18–24. [Google Scholar] [CrossRef] [Green Version]
- Sugita, K.; Akdis, C.A. Recent Developments and Advances in Atopic Dermatitis and Food Allergy. Allergol. Int. 2020, 69, 204–214. [Google Scholar] [CrossRef]
- Shen, X.; Wang, M.; Zhang, X.; He, M.; Li, M.; Cheng, G.; Wan, C.; He, F. Dynamic Construction of Gut Microbiota May Influence Allergic Diseases of Infants in Southwest China. BMC Microbiol. 2019, 19, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Song, H.; Yoo, Y.; Hwang, J.; Na, Y.C.; Kim, H.S. Faecalibacterium Prausnitzii Subspecies-Level Dysbiosis in the Human Gut Microbiome Underlying Atopic Dermatitis. J. Allergy Clin. Immunol. 2016, 137, 852–860. [Google Scholar] [CrossRef]
- Lee, E.; Lee, S.Y.; Kang, M.J.; Kim, K.; Won, S.; Kim, B.J.; Choi, K.Y.; Kim, B.S.; Cho, H.J.; Kim, Y.; et al. Clostridia in the Gut and Onset of Atopic Dermatitis via Eosinophilic Inflammation. Ann. Allergy Asthma Immunol. 2016, 117, 91–92.e1. [Google Scholar] [CrossRef]
- Fujimura, K.E.; Sitarik, A.R.; Havstad, S.; Lin, D.L.; Levan, S.; Fadrosh, D.; Panzer, A.R.; Lamere, B.; Rackaityte, E.; Lukacs, N.W.; et al. Neonatal Gut Microbiota Associates with Childhood Multisensitized Atopy and T Cell Differentiation. Nat. Med. 2016, 22, 1187–1191. [Google Scholar] [CrossRef] [Green Version]
- Nylund, L.; Nermes, M.; Isolauri, E.; Salminen, S.; de Vos, W.M.; Satokari, R. Severity of Atopic Disease Inversely Correlates with Intestinal Microbiota Diversity and Butyrate-Producing Bacteria. Allergy 2015, 70, 241–244. [Google Scholar] [CrossRef]
- Bertelsen, R.J.; Brantsæter, A.L.; Magnus, M.C.; Haugen, M.; Myhre, R.; Jacobsson, B.; Longnecker, M.P.; Meltzer, H.M.; London, S.J. Probiotic Milk Consumption in Pregnancy and Infancy and Subsequent Childhood Allergic Diseases. J. Allergy Clin. Immunol. 2014, 133, 165–171. [Google Scholar] [CrossRef] [Green Version]
- Penders, J.; Gerhold, K.; Stobberingh, E.E.; Thijs, C.; Zimmermann, K.; Lau, S.; Hamelmann, E. Establishment of the Intestinal Microbiota and Its Role for Atopic Dermatitis in Early Childhood. J. Allergy Clin. Immunol. 2013, 132, 601–607. [Google Scholar] [CrossRef]
- Han, P.; Gu, J.Q.; Li, L.S.; Wang, X.Y.; Wang, H.T.; Wang, Y.; Chang, C.; Sun, J.L. The Association Between Intestinal Bacteria and Allergic Diseases-Cause or Consequence? Front. Cell. Infect. Microbiol. 2021, 11, 284. [Google Scholar] [CrossRef]
- Stokes, J.H.; Pillsbury, D.M. The effect on the skin of emotional and nervous states: iii. theoretical and practical consideration of a gastro-intestinal mechanism. Arch. Derm. Syphilol. 1930, 22, 962–993. [Google Scholar] [CrossRef]
- Bowe, W.P.; Logan, A.C. Acne Vulgaris, Probiotics and the Gut-Brain-Skin Axis—Back to the Future? Gut Pathog. 2011, 3, 1. [Google Scholar] [CrossRef] [Green Version]
- Feleszko, W.; Jaworska, J.; Rha, R.D.; Steinhausen, S.; Avagyan, A.; Jaudszus, A.; Ahrens, B.; Groneberg, D.A.; Wahn, U.; Hamelmann, E. Probiotic-Induced Suppression of Allergic Sensitization and Airway Inflammation Is Associated with an Increase of T Regulatory-Dependent Mechanisms in a Murine Model of Asthma. Clin. Exp. Allergy 2007, 37, 498–505. [Google Scholar] [CrossRef]
- Kim, H.J.; Kim, Y.J.; Kang, M.J.; Seo, J.H.; Kim, H.Y.; Jeong, S.K.; Lee, S.H.; Kim, J.M.; Hong, S.J. A Novel Mouse Model of Atopic Dermatitis with Epicutaneous Allergen Sensitization and the Effect of Lactobacillus Rhamnosus. Exp. Dermatol. 2012, 21, 672–675. [Google Scholar] [CrossRef]
- Kim, J.Y.; Park, B.K.; Park, H.J.; Park, Y.H.; Kim, B.O.; Pyo, S. Atopic Dermatitis-Mitigating Effects of New Lactobacillus Strain, Lactobacillus Sakei Probio 65 Isolated from Kimchi. J. Appl. Microbiol. 2013, 115, 517–526. [Google Scholar] [CrossRef]
- Matsumoto, M.; Aranami, A.; Ishige, A.; Watanabe, K.; Benno, Y. LKM512 Yogurt Consumption Improves the Intestinal Environment and Induces the T-Helper Type 1 Cytokine in Adult Patients with Intractable Atopic Dermatitis. Clin. Exp. Allergy 2007, 37, 358–370. [Google Scholar] [CrossRef]
- Weston, S.; Halbert, A.; Richmond, P.; Prescott, S.L. Effects of Probiotics on Atopic Dermatitis: A Randomised Controlled Trial. Arch. Dis. Child. 2005, 90, 892–897. [Google Scholar] [CrossRef] [Green Version]
- Kalliomäki, M.; Salminen, S.; Arvilommi, H.; Kero, P.; Koskinen, P.; Isolauri, E. Probiotics in Primary Prevention of Atopic Disease: A Randomised Placebo-Controlled Trial. Lancet 2001, 357, 1076–1079. [Google Scholar] [CrossRef]
- Kukkonen, K.; Savilahti, E.; Haahtela, T.; Juntunen-Backman, K.; Korpela, R.; Poussa, T.; Tuure, T.; Kuitunen, M. Probiotics and Prebiotic Galacto-Oligosaccharides in the Prevention of Allergic Diseases: A Randomized, Double-Blind, Placebo-Controlled Trial. J. Allergy Clin. Immunol. 2007, 119, 192–198. [Google Scholar] [CrossRef]
- Lee, J.; Seto, D.; Bielory, L. Meta-Analysis of Clinical Trials of Probiotics for Prevention and Treatment of Pediatric Atopic Dermatitis. J. Allergy Clin. Immunol. 2008, 121, 116–121. [Google Scholar] [CrossRef]
- Michail, S.K.; Stolfi, A.; Johnson, T.; Onady, G.M. Efficacy of Probiotics in the Treatment of Pediatric Atopic Dermatitis: A Meta-Analysis of Randomized Controlled Trials. Ann. Allergy Asthma Immunol. 2008, 101, 508–516. [Google Scholar] [CrossRef]
- Wickens, K.; Black, P.N.; Stanley, T.V.; Mitchell, E.; Fitzharris, P.; Tannock, G.W.; Purdie, G.; Crane, J. A Differential Effect of 2 Probiotics in the Prevention of Eczema and Atopy: A Double-Blind, Randomized, Placebo-Controlled Trial. J. Allergy Clin. Immunol. 2008, 122, 788–794. [Google Scholar] [CrossRef]
- Woo, S.I.; Kim, J.Y.; Lee, Y.J.; Kim, N.S.; Hahn, Y.S. Effect of Lactobacillus Sakei Supplementation in Children with Atopic Eczema-Dermatitis Syndrome. Ann. Allergy Asthma Immunol. 2010, 104, 343–348. [Google Scholar] [CrossRef]
- Betsi, G.I.; Papadavid, E.; Falagas, M.E. Probiotics for the Treatment or Prevention of Atopic Dermatitis: A Review of the Evidence from Randomized Controlled Trials. Am. J. Clin. Dermatol. 2008, 9, 93–103. [Google Scholar] [CrossRef]
- Han, Y.; Kim, B.; Ban, J.; Lee, J.; Kim, B.J.; Choi, B.S.; Hwang, S.; Ahn, K.; Kim, J. A Randomized Trial of Lactobacillus Plantarum CJLP133 for the Treatment of Atopic Dermatitis. Pediatr. Allergy Immunol. 2012, 23, 667–673. [Google Scholar] [CrossRef]
- Rautava, S.; Kainonen, E.; Salminen, S.; Isolauri, E. Maternal Probiotic Supplementation during Pregnancy and Breast-Feeding Reduces the Risk of Eczema in the Infant. J. Allergy Clin. Immunol. 2012, 130, 1355–1360. [Google Scholar] [CrossRef]
- Wickens, K.; Black, P.; Stanley, T.V.; Mitchell, E.; Barthow, C.; Fitzharris, P.; Purdie, G.; Crane, J. A Protective Effect of Lactobacillus Rhamnosus HN001 against Eczema in the First 2 Years of Life Persists to Age 4 Years. Clin. Exp. Allergy 2012, 42, 1071–1079. [Google Scholar] [CrossRef]
- Kim, S.O.; Ah, Y.M.; Yu, Y.M.; Choi, K.H.; Shin, W.G.; Lee, J.Y. Effects of Probiotics for the Treatment of Atopic Dermatitis: A Meta-Analysis of Randomized Controlled Trials. Ann. Allergy Asthma Immunol. 2014, 113, 217–226. [Google Scholar] [CrossRef]
- Enomoto, T.; Sowa, M.; Nishimori, K.; Shimazu, S.; Yoshida, A.; Yamada, K.; Furukawa, F.; Nakagawa, T.; Yanagisawa, N.; Iwabuchi, N.; et al. Effects of Bifidobacterial Supplementation to Pregnant Women and Infants in the Prevention of Allergy Development in Infants and on Fecal Microbiota. Allergol. Int. 2014, 63, 575–585. [Google Scholar] [CrossRef] [Green Version]
- Foolad, N.; Armstrong, A.W. Prebiotics and Probiotics: The Prevention and Reduction in Severity of Atopic Dermatitis in Children. Benef. Microbes 2014, 5, 151–160. [Google Scholar] [CrossRef]
- Makrgeorgou, A.; Leonardi-Bee, J.; Bath-Hextall, F.J.; Murrell, D.F.; Tang, M.L.K.; Roberts, A.; Boyle, R.J. Probiotics for Treating Eczema. Cochrane Database Syst. Rev. 2018, 11. [Google Scholar] [CrossRef]
- Tan-Lim, C.S.C.; Esteban-Ipac, N.A.R.; Recto, M.S.T.; Castor, M.A.R.; Casis-Hao, R.J.; Nano, A.L.M. Comparative Effectiveness of Probiotic Strains on the Prevention of Pediatric Atopic Dermatitis: A Systematic Review and Network Meta-Analysis. Pediatr. Allergy Immunol. 2021, 32, 1255–1270. [Google Scholar] [CrossRef]
- Pachacama López, A.F.; Tapia Portilla, M.F.; Moreno-Piedrahíta Hernández, F.; Palacios-Álvarez, S. Probiotics to Reduce the Severity of Atopic Dermatitis in Pediatric Patients: A Systematic Review and Meta-Analysis. Actas Dermo Sifiliográficas 2021, 112, 881–890. [Google Scholar] [CrossRef]
- Rosenfeldt, V.; Benfeldt, E.; Nielsen, S.D.; Michaelsen, K.F.; Jeppesen, D.L.; Valerius, N.H.; Paerregaard, A. Effect of Probiotic Lactobacillus Strains in Children with Atopic Dermatitis. J. Allergy Clin. Immunol. 2003, 111, 389–395. [Google Scholar] [CrossRef]
- Leshem, Y.A.; Hajar, T.; Hanifin, J.M.; Simpson, E.L. What the Eczema Area and Severity Index Score Tells Us about the Severity of Atopic Dermatitis: An Interpretability Study. Br. J. Dermatol. 2015, 172, 1353–1357. [Google Scholar] [CrossRef]
- Simpson, E.L.; Bieber, T.; Guttman-Yassky, E.; Beck, L.A.; Blauvelt, A.; Cork, M.J.; Silverberg, J.I.; Deleuran, M.; Kataoka, Y.; Lacour, J.-P.; et al. Two Phase 3 Trials of Dupilumab versus Placebo in Atopic Dermatitis. N. Engl. J. Med. 2016, 375, 2335–2348. [Google Scholar] [CrossRef]
- Szajewska, H.; Horvath, A. Lactobacillus Rhamnosus GG in the Primary Prevention of Eczema in Children: A Systematic Review and Meta-Analysis. Nutrients 2018, 10, 1319. [Google Scholar] [CrossRef] [Green Version]
- Tan, W.; Zhou, Z.; Li, W.; Lu, H.; Qiu, Z. Lactobacillus Rhamnosus GG for Cow’s Milk Allergy in Children: A Systematic Review and Meta-Analysis. Front. Pediatr. 2021, 9, 1127. [Google Scholar] [CrossRef]
- Boyle, R.J.; Ismail, I.H.; Kivivuori, S.; Licciardi, P.V.; Robins-Browne, R.M.; Mah, L.J.; Axelrad, C.; Moore, S.; Donath, S.; Carlin, J.B.; et al. Lactobacillus GG Treatment during Pregnancy for the Prevention of Eczema: A Randomized Controlled Trial. Allergy 2011, 66, 509–516. [Google Scholar] [CrossRef]
- Viljanen, M.; Savilahti, E.; Haahtela, T.; Juntunen-Backman, K.; Korpela, R.; Poussa, T.; Tuure, T.; Kuitunen, M. Probiotics in the Treatment of Atopic Eczema/Dermatitis Syndrome in Infants: A Double-Blind Placebo-Controlled Trial. Allergy 2005, 60, 494–500. [Google Scholar] [CrossRef]
- Viljanen, M.; Kuitunen, M.; Haahtela, T.; Juntunen-Backman, K.; Korpela, R.; Savilahti, E. Probiotic Effects on Faecal Inflammatory Markers and on Faecal IgA in Food Allergic Atopic Eczema/Dermatitis Syndrome Infants. Pediatr. Allergy Immunol. 2005, 16, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Hirose, Y.; Yamamoto, Y.; Yoshikai, Y.; Murosaki, S. Oral Intake of Heat-Killed Lactobacillus Plantarum L-137 Decreases the Incidence of Upper Respiratory Tract Infection in Healthy Subjects with High Levels of Psychological Stress. J. Nutr. Sci. 2013, 2, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Hirose, Y.; Murosaki, S.; Yamamoto, Y.; Yoshikai, Y.; Tsuru, T. Daily Intake of Heat-Killed Lactobacillus Plantarum L-137 Augments Acquired Immunity in Healthy Adults. J. Nutr. 2006, 136, 3069–3073. [Google Scholar] [CrossRef] [Green Version]
- Cuello-Garcia, C.A.; Fiocchi, A.; Pawankar, R.; Yepes-Nuñez, J.J.; Morgano, G.P.; Zhang, Y.; Ahn, K.; Al-Hammadi, S.; Agarwal, A.; Gandhi, S.; et al. World Allergy Organization-McMaster University Guidelines for Allergic Disease Prevention (GLAD-P): Prebiotics. World Allergy Organ. J. 2016, 9, 10. [Google Scholar] [CrossRef]
- Osborn, D.A.; Sinn, J.K. Prebiotics in Infants for Prevention of Allergy. Cochrane Database Syst. Rev. 2013, 2013. [Google Scholar] [CrossRef] [PubMed]
- Closa-Monasterolo, R.; Gispert-Llaurado, M.; Luque, V.; Ferre, N.; Rubio-Torrents, C.; Zaragoza-Jordana, M.; Escribano, J. Safety and Efficacy of Inulin and Oligofructose Supplementation in Infant Formula: Results from a Randomized Clinical Trial. Clin. Nutr. 2013, 32, 918–927. [Google Scholar] [CrossRef] [PubMed]
- Costalos, C.; Kapiki, A.; Apostolou, M.; Papathoma, E. The Effect of a Prebiotic Supplemented Formula on Growth and Stool Microbiology of Term Infants. Early Hum. Dev. 2008, 84, 45–49. [Google Scholar] [CrossRef] [PubMed]
- Bruzzese, E.; Volpicelli, M.; Squeglia, V.; Bruzzese, D.; Salvini, F.; Bisceglia, M.; Lionetti, P.; Cinquetti, M.; Iacono, G.; Amarri, S.; et al. A Formula Containing Galacto- and Fructo-Oligosaccharides Prevents Intestinal and Extra-Intestinal Infections: An Observational Study. Clin. Nutr. 2009, 28, 156–161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Caporaso, J.G.; Lauber, C.L.; Walters, W.A.; Berg-Lyons, D.; Huntley, J.; Fierer, N.; Owens, S.M.; Betley, J.; Fraser, L.; Bauer, M.; et al. Ultra-High-Throughput Microbial Community Analysis on the Illumina HiSeq and MiSeq Platforms. ISME J. 2012, 6, 1621–1624. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bolyen, E.; Rideout, J.R.; Dillon, M.R.; Bokulich, N.A.; Abnet, C.C.; Al-Ghalith, G.A.; Alexander, H.; Alm, E.J.; Arumugam, M.; Asnicar, F.; et al. Reproducible, Interactive, Scalable and Extensible Microbiome Data Science Using QIIME 2. Nat. Biotechnol. 2019, 37, 852–857. [Google Scholar] [CrossRef] [PubMed]
- Callahan, B.J.; McMurdie, P.J.; Rosen, M.J.; Han, A.W.; Johnson, A.J.A.; Holmes, S.P. DADA2: High-Resolution Sample Inference from Illumina Amplicon Data. Nat. Methods 2016, 13, 581–583. [Google Scholar] [CrossRef] [Green Version]
- Callahan, B.J.; McMurdie, P.J.; Holmes, S.P. Exact Sequence Variants Should Replace Operational Taxonomic Units in Marker-Gene Data Analysis. ISME J. 2017, 11, 2639–2643. [Google Scholar] [CrossRef] [Green Version]
- Katoh, K.; Misawa, K.; Kuma, K.I.; Miyata, T. MAFFT: A Novel Method for Rapid Multiple Sequence Alignment Based on Fast Fourier Transform. Nucleic Acids Res. 2002, 30, 3059–3066. [Google Scholar] [CrossRef] [Green Version]
- Price, M.N.; Dehal, P.S.; Arkin, A.P. FastTree 2—Approximately Maximum-Likelihood Trees for Large Alignments. PLoS ONE 2010, 5, e9490. [Google Scholar] [CrossRef]
- Bokulich, N.A.; Kaehler, B.D.; Rideout, J.R.; Dillon, M.; Bolyen, E.; Knight, R.; Huttley, G.A.; Gregory Caporaso, J. Optimizing Taxonomic Classification of Marker-Gene Amplicon Sequences with QIIME 2’s Q2-Feature-Classifier Plugin. Microbiome 2018, 6, 90. [Google Scholar] [CrossRef] [PubMed]
- Quast, C.; Pruesse, E.; Yilmaz, P.; Gerken, J.; Schweer, T.; Yarza, P.; Peplies, J.; Glöckner, F.O. The SILVA Ribosomal RNA Gene Database Project: Improved Data Processing and Web-Based Tools. Nucleic Acids Res. 2013, 41, D590–D596. [Google Scholar] [CrossRef]
- Yilmaz, P.; Parfrey, L.W.; Yarza, P.; Gerken, J.; Pruesse, E.; Quast, C.; Schweer, T.; Peplies, J.; Ludwig, W.; Glöckner, F.O. The SILVA and “All-Species Living Tree Project (LTP)” Taxonomic Frameworks. Nucleic Acids Res. 2014, 42, D643–D648. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Glöckner, F.O.; Yilmaz, P.; Quast, C.; Gerken, J.; Beccati, A.; Ciuprina, A.; Bruns, G.; Yarza, P.; Peplies, J.; Westram, R.; et al. 25 Years of Serving the Community with Ribosomal RNA Gene Reference Databases and Tools. J. Biotechnol. 2017, 261, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Cui, Y.; Li, X.; Yao, M. Microeco: An R Package for Data Mining in Microbial Community Ecology. FEMS Microbiol. Ecol. 2021, 97, fiaa255. [Google Scholar] [CrossRef] [PubMed]
- Anderson, M.J. Permutational Multivariate Analysis of Variance (PERMANOVA). Wiley StatsRef Stat. Ref. Online 2017, 1–15. [Google Scholar] [CrossRef]
- Beck, D.; Foster, J.A. Machine Learning Techniques Accurately Classify Microbial Communities by Bacterial Vaginosis Characteristics. PLoS ONE 2014, 9, e87830. [Google Scholar] [CrossRef] [Green Version]
- Yatsunenko, T.; Rey, F.E.; Manary, M.J.; Trehan, I.; Dominguez-Bello, M.G.; Contreras, M.; Magris, M.; Hidalgo, G.; Baldassano, R.N.; Anokhin, A.P.; et al. Human Gut Microbiome Viewed across Age and Geography. Nature 2012, 486, 222–227. [Google Scholar] [CrossRef] [Green Version]
- Martinez-Taboada, F.; Redondo, J.I. The SIESTA (SEAAV Integrated Evaluation Sedation Tool for Anaesthesia) Project: Initial Development of a Multifactorial Sedation Assessment Tool for Dogs. PLoS ONE 2020, 15, e0230799. [Google Scholar] [CrossRef] [Green Version]
- Schram, M.E.; Spuls, P.I.; Leeflang, M.M.G.; Lindeboom, R.; Bos, J.D.; Schmitt, J. EASI, (Objective) SCORAD and POEM for Atopic Eczema: Responsiveness and Minimal Clinically Important Difference. Allergy 2012, 67, 99–106. [Google Scholar] [CrossRef]
- Reddel, S.; del Chierico, F.; Quagliariello, A.; Giancristoforo, S.; Vernocchi, P.; Russo, A.; Fiocchi, A.; Rossi, P.; Putignani, L.; el Hachem, M. Gut Microbiota Profile in Children Affected by Atopic Dermatitis and Evaluation of Intestinal Persistence of a Probiotic Mixture. Sci. Rep. 2019, 9, 4996. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miquel, S.; Martín, R.; Rossi, O.; Bermúdez-Humarán, L.G.; Chatel, J.M.; Sokol, H.; Thomas, M.; Wells, J.M.; Langella, P. Faecalibacterium Prausnitzii and Human Intestinal Health. Curr. Opin. Microbiol. 2013, 16, 255–261. [Google Scholar] [CrossRef] [PubMed]
- Reichardt, N.; Duncan, S.H.; Young, P.; Belenguer, A.; McWilliam Leitch, C.; Scott, K.P.; Flint, H.J.; Louis, P. Phylogenetic Distribution of Three Pathways for Propionate Production within the Human Gut Microbiota. ISME J. 2014, 8, 1323–1335. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shu, M.; Wang, Y.; Yu, J.; Kuo, S.; Coda, A.; Jiang, Y.; Gallo, R.L.; Huang, C.M. Fermentation of Propionibacterium Acnes, a Commensal Bacterium in the Human Skin Microbiome, as Skin Probiotics against Methicillin-Resistant Staphylococcus Aureus. PLoS ONE 2013, 8, e55380. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de Benedetto, A.; Rafaels, N.M.; McGirt, L.Y.; Ivanov, A.I.; Georas, S.N.; Cheadle, C.; Berger, A.E.; Zhang, K.; Vidyasagar, S.; Yoshida, T.; et al. Tight Junction Defects in Patients with Atopic Dermatitis. J. Allergy Clin. Immunol. 2011, 127, 773–786.e7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Macia, L.; Thorburn, A.N.; Binge, L.C.; Marino, E.; Rogers, K.E.; Maslowski, K.M.; Vieira, A.T.; Kranich, J.; Mackay, C.R. Microbial Influences on Epithelial Integrity and Immune Function as a Basis for Inflammatory Diseases. Immunol. Rev. 2012, 245, 164–176. [Google Scholar] [CrossRef]
- Paliy, O.; Rajakaruna, S. Development of Microbiota—Is the Process Continuing Through Adolescence? Compr. Gut Microb. 2022, 59–68. [Google Scholar] [CrossRef]
- Holmes, Z.C.; Silverman, J.D.; Dressman, H.K.; Wei, Z.; Dallow, E.P.; Armstrong, S.C.; Seed, P.C.; Rawls, J.F.; David, L.A. Short-Chain Fatty Acid Production by Gut Microbiota from Children with Obesity Differs According to Prebiotic Choice and Bacterial Community Composition. mBio 2020, 11, 1–15. [Google Scholar] [CrossRef]
- Zhou, W.; Zhang, D.; Li, Z.; Jiang, H.; Li, J.; Ren, R.; Gao, X.; Li, J.; Wang, X.; Wang, W.; et al. The Fecal Microbiota of Patients with Pancreatic Ductal Adenocarcinoma and Autoimmune Pancreatitis Characterized by Metagenomic Sequencing. J. Transl. Med. 2021, 19, 215. [Google Scholar] [CrossRef]
- Han, Y.; Gong, Z.; Sun, G.; Xu, J.; Qi, C.; Sun, W.; Jiang, H.; Cao, P.; Ju, H. Dysbiosis of Gut Microbiota in Patients With Acute Myocardial Infarction. Front. Microbiol. 2021, 12, 1489. [Google Scholar] [CrossRef]
- Louca, P.; Nogal, A.; Wells, P.M.; Asnicar, F.; Wolf, J.; Steves, C.J.; Spector, T.D.; Segata, N.; Berry, S.E.; Valdes, A.M.; et al. Gut Microbiome Diversity and Composition Is Associated with Hypertension in Women. J. Hypertens. 2021, 39, 1810–1816. [Google Scholar] [CrossRef] [PubMed]
- Seo, B.; Jeon, K.; Baek, I.; Lee, Y.M.; Baek, K.; Ko, G.P. Faecalibacillus Intestinalis Gen. Nov., Sp. Nov. and Faecalibacillus Faecis Sp. Nov., Isolated from Human Faeces. Int. J. Syst. Evol. Microbiol. 2019, 69, 2120–2128. [Google Scholar] [CrossRef]
- Singh, H.; Torralba, M.G.; Moncera, K.J.; DiLello, L.; Petrini, J.; Nelson, K.E.; Pieper, R. Gastro-Intestinal and Oral Microbiome Signatures Associated with Healthy Aging. Geroscience 2019, 41, 907–921. [Google Scholar] [CrossRef]
- JDDW 2014 Abstracts: The Relationship between Fusicatenibacter Saccharivorans and Inflammatory Bowel Disease. Available online: https://www.jddw.jp/jddw2014/abstracts-eng/abst/60011.html (accessed on 3 November 2022).
- Plaut, A.G.; Qiu, J. IgA-Specific Metalloendopeptidase. Handb. Proteolytic Enzymes 2013, 1, 1243–1248. [Google Scholar] [CrossRef]
- Natividad, J.M.; Lamas, B.; Pham, H.P.; Michel, M.L.; Rainteau, D.; Bridonneau, C.; da Costa, G.; van Hylckama Vlieg, J.; Sovran, B.; Chamignon, C.; et al. Bilophila Wadsworthia Aggravates High Fat Diet Induced Metabolic Dysfunctions in Mice. Nat. Commun. 2018, 9, 2802. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, R.; Sun, X.; Liu, X.; Yang, Y.; Li, Z. Autoimmune Diseases in China. Adv. Immunol. 2019, 144, 173–216. [Google Scholar] [CrossRef] [PubMed]
- Douzandeh-Mobarrez, B.; Kariminik, A. Gut Microbiota and IL-17A: Physiological and Pathological Responses. Probiotics Antimicrob. Proteins 2019, 11, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Greenacre, M.; Martínez-Álvaro, M.; Blasco, A. Compositional Data Analysis of Microbiome and Any-Omics Datasets: A Validation of the Additive Logratio Transformation. Front. Microbiol. 2021, 12, 727398. [Google Scholar] [CrossRef]
- Wang, Y.; Hou, J.; Chi-Ching Tsui, J.; Wang, L.; Zhou, J.; Kei Chan, U.; Jun Yi Lo, C.; Ling Kella Siu, P.; King Fan Loo, S.; Kwok Wing Tsui, S.; et al. Unique Gut Microbiome Signatures among Adult Patients with Moderate to Severe Atopic Dermatitis in Southern Chinese. bioRxiv 2022. [Google Scholar] [CrossRef]
- Gagliardi, A.; Totino, V.; Cacciotti, F.; Iebba, V.; Neroni, B.; Bonfiglio, G.; Trancassini, M.; Passariello, C.; Pantanella, F.; Schippa, S. Rebuilding the Gut Microbiota Ecosystem. Int. J. Environ. Res. Public Health 2018, 15, 1679. [Google Scholar] [CrossRef]
- McFarland, L.V. Use of Probiotics to Correct Dysbiosis of Normal Microbiota Following Disease or Disruptive Events: A Systematic Review. BMJ Open 2014, 4, e005047. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Singh, T.P.; Natraj, B.H. Next-Generation Probiotics: A Promising Approach towards Designing Personalized Medicine. Crit Rev. Microbiol. 2021, 47, 479–498. [Google Scholar] [CrossRef] [PubMed]
- Zmora, N.; Zilberman-Schapira, G.; Suez, J.; Mor, U.; Dori-Bachash, M.; Bashiardes, S.; Kotler, E.; Zur, M.; Regev-Lehavi, D.; Brik, R.B.Z.; et al. Personalized Gut Mucosal Colonization Resistance to Empiric Probiotics Is Associated with Unique Host and Microbiome Features. Cell 2018, 174, 1388–1405.e21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vemuri, R.; Shankar, E.M.; Chieppa, M.; Eri, R.; Kavanagh, K. Beyond Just Bacteria: Functional Biomes in the Gut Ecosystem Including Virome, Mycobiome, Archaeome and Helminths. Microorganisms 2020, 8, 483. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guzzo, G.L.; Andrews, J.M.; Weyrich, L.S. The Neglected Gut Microbiome: Fungi, Protozoa, and Bacteriophages in Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2022, 28, 1112–1122. [Google Scholar] [CrossRef] [PubMed]


| Patients (No.) | ||||||
|---|---|---|---|---|---|---|
| Variable | Overall (n = 41) | Mild AD (n = 17) | Severe AD (n = 24) | p Value | ||
| Characteristics | ||||||
| Sex, No. (%) | 0.5737 | |||||
| Male | 16 (39.0) | 8 (47.1) | 8 (33.3) | |||
| Female | 25 (61.0) | 9 (52.9) | 16 (66.6) | |||
| Age, mean (SD) [range], y | 47.0 (15.6) [18–73] | 47.6 (15.5) [26–66] | 46.6 (16.0) [18–73] | 0.8633 | ||
| Weight, mean (SD), kg | 59.9 (11.1) | 62.5 (11.1) | 58.0 (10.9) | 0.1414 | ||
| BMI, mean (SD) † | 22.5 (3.3) | 23.1 (3.3) | 22.1 (3.3) | 0.3898 | ||
| EASI, mean (SD) | 17.7 (7.0) | 10.7 (2.1) | 22.7 (4.5) | <0.001 | ||
| Presence of Comorbidity | ||||||
| Allergy ever, No. (%) | ||||||
| Food allergy | 3 (7.3) | 1 (5.9) | 2 (8.3) | >0.999 | ||
| Others | 14 (34.2) | 5 (29.4) | 9 (37.5) | 0.7417 | ||
| GI, No. (%) | ||||||
| Constipation | 14 (34.2) | 6 (35.3) | 8 (33.3) | >0.999 | ||
| Diarrhea | 6 (14.6) | 4 (23.5) | 2 (8.3) | 0.2118 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Y.; Choy, C.T.; Lin, Y.; Wang, L.; Hou, J.; Tsui, J.C.C.; Zhou, J.; Wong, C.H.; Yim, T.K.; Tsui, W.K.; et al. Effect of a Novel E3 Probiotics Formula on the Gut Microbiome in Atopic Dermatitis Patients: A Pilot Study. Biomedicines 2022, 10, 2904. https://doi.org/10.3390/biomedicines10112904
Wang Y, Choy CT, Lin Y, Wang L, Hou J, Tsui JCC, Zhou J, Wong CH, Yim TK, Tsui WK, et al. Effect of a Novel E3 Probiotics Formula on the Gut Microbiome in Atopic Dermatitis Patients: A Pilot Study. Biomedicines. 2022; 10(11):2904. https://doi.org/10.3390/biomedicines10112904
Chicago/Turabian StyleWang, Yiwei, Chi Tung Choy, Yufeng Lin, Lin Wang, Jinpao Hou, Joseph Chi Ching Tsui, Junwei Zhou, Chi Ho Wong, Tai Ki Yim, Wai Kai Tsui, and et al. 2022. "Effect of a Novel E3 Probiotics Formula on the Gut Microbiome in Atopic Dermatitis Patients: A Pilot Study" Biomedicines 10, no. 11: 2904. https://doi.org/10.3390/biomedicines10112904






