Depressive Symptoms among Patients with Heart Failure in Korea: An Integrative Review
Abstract
:1. Introduction
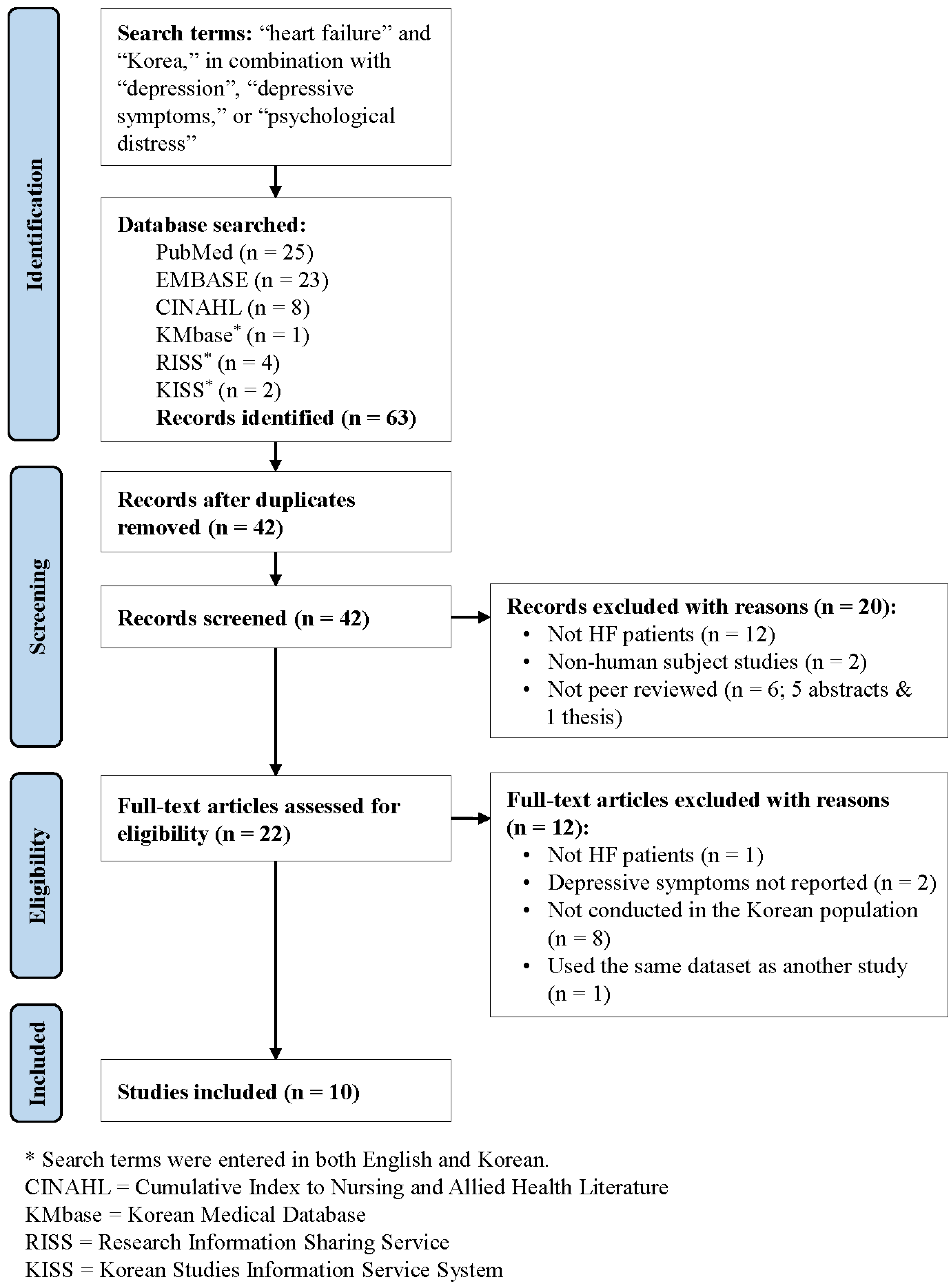
2. Methods
3. Results
3.1. Study Characteristics
3.2. Depressive Symptoms
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| HF | Heart failure |
| CINAHL | Cumulative Index to Nursing and Allied Health Literature |
| KMbase | Korean Medical Database |
| RISS | Research Information Sharing Service |
| KISS | Korean Studies Information Service System |
| NYHA | New York Heart Association |
| BDI | Beck Depression Inventory |
| CES-D | Center for Epidemiologic Studies Depression Scale |
| GDS-SF | Geriatric Depression Scale-Short Form |
| PHQ-9 | Patient Health Questionnaire |
References
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; Arnett, D.K.; Blaha, M.J.; Cushman, M.; Das, S.R.; de Ferranti, S.; Després, J.P.; Fullerton, H.J.; et al. Heart Disease and Stroke Statistics-2016 update: A report from the American Heart Association. Circulation 2016, 133, e38–e60. [Google Scholar] [CrossRef] [PubMed]
- Dickstein, K.; Cohen-Solal, A.; Filippatos, G.; McMurray, J.J.; Ponikowski, P.; Poole-Wilson, P.A.; Strömberg, A.; Veldhuisen, D.J.; Atar, D.; Hoes, A.W.; et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: The task force for the diagnosis and treatment of acute and chronic heart failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur. J. Heart Fail 2008, 10, 933–989. [Google Scholar] [PubMed]
- Heidenreich, P.A.; Trogdon, J.G.; Khavjou, O.A.; Butler, J.; Dracup, K.; Ezekowitz, M.D.; Finkelstein, E.A.; Hong, Y.; Johnston, S.C.; Khera, A.; et al. Forecasting the future of cardiovascular disease in the United States: A policy statement from the American Heart Association. Circulation 2011, 123, 933–944. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.-M. Medical Treatment of Acute Decompensated Heart Failure Syndrome. Korean J. Med. 2015, 88, 121–126. [Google Scholar] [CrossRef]
- Yancy, C.W.; Jessup, M.; Bozkurt, B.; Butler, J.; Casey, D.E., Jr.; Drazner, M.H.; Fonarow, G.C.; Geraci, S.A.; Horwich, T.; Januzzi, J.L.; et al. ACCF/AHA guideline for the management of heart failure: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2013, 62, e147–e239. [Google Scholar] [CrossRef] [PubMed]
- Rutledge, T.; Reis, V.A.; Linke, S.E.; Greenberg, B.H.; Mills, P.J. Depression in heart failure: A meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J. Am. Coll. Cardiol. 2006, 48, 1527–1537. [Google Scholar] [CrossRef] [PubMed]
- York, K.M.; Hassan, M.; Sheps, D.S. Psychobiology of depression/distress in congestive heart failure. Heart Fail Rev. 2009, 14, 35–50. [Google Scholar] [CrossRef] [PubMed]
- Joynt, K.E.; Whellan, D.J.; O’Connor, C.M. Why is depression bad for the failing heart? A review of the mechanistic relationship between depression and heart failure. J. Card. Fail 2004, 10, 258–271. [Google Scholar] [CrossRef] [PubMed]
- Hwang, B.; Moser, D.K.; Dracup, K. Knowledge is insufficient for self-care among heart failure patients with psychological distress. Health Psychol. 2014, 33, 588–596. [Google Scholar] [CrossRef] [PubMed]
- Hwang, B.; Moser, D.K.; Pelter, M.M.; Nesbitt, T.S.; Dracup, K. Changes in Depressive Symptoms and Mortality in Patients With Heart Failure: Effects of Cognitive-Affective and Somatic Symptoms. Psychosom. Med. 2015, 77, 798–807. [Google Scholar] [CrossRef] [PubMed]
- Tsai, J.L.; Chentsova-Dutton, Y. Understanding depression across cultures. In Handbook of depression, 3rd ed.; Gotlib, I.H., Hammen, C.L., Eds.; Guilford Press: New York, NY, USA, 2014; pp. 467–491. [Google Scholar]
- Whittemore, R.; Knafl, K. The integrative review: Updated methodology. J. Adv. Nurs. 2005, 52, 546–553. [Google Scholar] [CrossRef] [PubMed]
- Song, E.K. Adherence to the low-sodium diet plays a role in the interaction between depressive symptoms and prognosis in patients with heart failure. J. Cardiovasc. Nurs. 2009, 24, 299–305. [Google Scholar] [CrossRef] [PubMed]
- Song, E.K.; Lee, Y.; Moser, D.K.; Dekker, R.L.; Kang, S.M.; Lennie, T.A. The link of unintentional weight loss to cardiac event-free survival in patients with heart failure. J. Cardiovasc. Nurs. 2014, 29, 439–447. [Google Scholar] [CrossRef] [PubMed]
- Song, E.K.; Moser, D.K.; Dekker, R.L.; Lennie, T.A. The Impact of Body Mass Index on the Link between Depressive Symptoms and Health Outcome in Patients with Heart Failure. J. Cardiovasc. Nurs. 2015, 30, 529–536. [Google Scholar] [CrossRef] [PubMed]
- Song, E.K.; Moser, D.K.; Kang, S.M.; Lennie, T.A. Association of Depressive Symptoms and Micronutrient Deficiency with Cardiac Event-Free Survival in Patients with Heart Failure. J. Card. Fail 2015, 21, 945–951. [Google Scholar] [CrossRef] [PubMed]
- Chu, S.H.; Ko, I.S.; Lee, W.H.; Yoo, J.S.; Kang, S.M.; Jung, H.Y.; Kim, D.R.; Ahn, J.H.; Lee, Y.J. Factors affecting medication adherence in patients with chronic heart failure. J. Korean Biol. Nurs. Sci. 2012, 14, 193–202. [Google Scholar] [CrossRef]
- Son, Y.J.; Song, Y.; Nam, S.; Shin, W.Y.; Lee, S.J.; Jin, D.K. Factors associated with health-related quality of life in elderly Korean patients with heart failure. J. Adv. Nurs. 2012, 27, 528–538. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Jang, J.H.; Lee, S.H.; Chun, K.J.; Kim, J.H. Self-Care Behavior and Depression in Patients with Heart Failure. J. Korean Acad. Fundam. Nurs. 2015, 22, 79–86. [Google Scholar] [CrossRef]
- Song, E.K.; Kim, C.J.; Yoo, I.Y.; Kim, G.Y.; Kim, J.H.; Ha, J.W. Factors influencing functional status in patients with heart failure. Taehan Kanho Hakhoe Chi 2006, 36, 853–862. [Google Scholar] [PubMed]
- Song, E.K.; Moser, D.K.; Lennie, T.A. Relationship of depressive symptoms to the impact of physical symptoms on functional status in women with heart failure. Am. J. Crit. Care 2009, 18, 348–356. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.-H.; Ahn, S.-H. Self-care compliance, family support, and depression in patients with congestive heart failure. J. Korean Acad. Funda Nurs. 2005, 12, 186–194. [Google Scholar]
- Johansson, P.; Lesman-Leegte, I.; Lundgren, J.; Hillege, H.L.; Hoes, A.; Sanderman, R.; van Veldhuisen, D.J.; Jaarsma, T. Time-course of depressive symptoms in patients with heart failure. J. Psychosom. Res. 2013, 74, 238–243. [Google Scholar] [CrossRef] [PubMed]
- Hare, D.L.; Toukhsati, S.R.; Johansson, P.; Jaarsma, T. Depression and cardiovascular disease: A clinical review. Eur. Heart J. 2014, 35, 1365–1372. [Google Scholar] [CrossRef] [PubMed]
- Williams, J.W., Jr.; Noel, P.H.; Cordes, J.A.; Ramirez, G.; Pignone, M. Is this patient clinically depressed? JAMA 2002, 287, 1160–1170. [Google Scholar] [CrossRef] [PubMed]
- Lichtman, J.H.; Bigger, J.T.; Blumenthal, J.A.; Frasure-Smith, N.; Kaufmann, P.G.; Lespérance, F.; Mark, D.B.; Sheps, D.S.; Taylor, C.B.; Froelicher, E.S. Depression and coronary heart disease: Recommendations for screening, referral, and treatment: A science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: Endorsed by the American Psychiatric Association. Circulation 2008, 118, 1768–1775. [Google Scholar] [PubMed]
- Choi, H.S.; Choi, J.H.; Park, K.H.; Joo, K.J.; Ga, H.; Ko, H.J.; Kim, S.R. Standardization of the Korean version of Patient Health Questionnaire-9 as a screening instrument for major depressive disorder. J. Korean Acad. Fam. Med. 2007, 28, 114–119. [Google Scholar]
- Park, S.C.; Oh, H.S.; Oh, D.H.; Jung, S.A.; Na, K.S.; Lee, H.Y.; Kang, R.H.; Choi, Y.K.; Lee, M.S.; Park, Y.C. Evidence-based, non-pharmacological treatment guideline for depression in Korea. J. Korean Med. Sci. 2014, 29, 12–22. [Google Scholar] [CrossRef] [PubMed]
- Lecrubier, Y. Physical components of depression and psychomotor retardation. J. Clin. Psychiatry 2006, 67 (Suppl. 6), 23–26. [Google Scholar] [PubMed]
| Study | Sample Size (N) | Data Collection Period | Patient Characteristics | Patient Recruitment Setting | Assessment of Depressive Symptoms | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age (Mean ± SD) | Female (%) | NYHA Class III or IV (%) | Measure | Score (Mean ± SD) | Cut-Off Score Used | Clinically Depressed (%) | ||||
| Chu et al., 2012 [17] | 133 | October 2010–February 2011 | 61.4 ± 13.6 | 26.3 | 10.0 | Out-patient | PHQ-9 | 4.1 ± 4.4 | ≥5 | 36.8 |
| Lee, H. et al., 2015 [19] | 169 | April 2012–September 2013 | 62.9 ± 8.7 | 19.5 | 9.5 | Out-patient | CES-D | 15.8 ± 10.0 | ≥16 | 43.2 |
| Lee, S. et al., 2005 [22] | 105 | May 2004–January 2005 | Not reported (≥65 years 73.3%) | 51.4 | 11.4 (No class IV) | Out-patient | CES-D | Mean = 30.18 SD = not reported | Not used | Not reported |
| Son et al., 2012 [18] | 134 | February 2010–May 2010 | 67.8 ± 8.8 | 63.4 | 26.1 (No class IV) | Out-patient | GDS-SF | 6.9 ± 3.8 | ≥5 | 67.9 |
| Song, 2009 [13] | 254 | September 2005–December 2006 | 62 ± 14 | 42.9 | 52.4 | Out-patient | BDI | 17.9 ± 9.6 | ≥16 | 48.4 |
| Song et al., 2006 [20] | 260 | September 2005–December 2005 | 62.2 ± 13.1 | 41.9 | 66.2 | In-patient | BDI | 18.3 ± 10.1 | Not used | Not reported |
| Song et al., 2009 [21] | 231 | Not reported | 63 ± 13 | 42.4 | Not reported | In-patient | BDI | Not reported | ≥17 | 44.6 |
| Song et al., 2014 [14] | 243 | Not reported | 61 ± 14 | 39.1 | 46.9 | In-patient | BDI | 14.7 ± 9.5 | ≥17 | 36.6 |
| Song et al., 2015 [15] | 297 | September 2011–December 2012 | 64.4 ± 9.8 | 28.3 | 51.2 | Out-patient | PHQ-9 | 6.0 ± 5.5 | ≥10 | 23.6 |
| Song et al., 2015 [16] | 232 | March 2012–March 2013 | 66 ± 8 | 33.6 | 45.2 | Out-patient | PHQ-9 | 6.9 ± 5.7 | ≥10 | 31.0 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hwang, B.; Choi, H. Depressive Symptoms among Patients with Heart Failure in Korea: An Integrative Review. Healthcare 2016, 4, 52. https://doi.org/10.3390/healthcare4030052
Hwang B, Choi H. Depressive Symptoms among Patients with Heart Failure in Korea: An Integrative Review. Healthcare. 2016; 4(3):52. https://doi.org/10.3390/healthcare4030052
Chicago/Turabian StyleHwang, Boyoung, and Heeseung Choi. 2016. "Depressive Symptoms among Patients with Heart Failure in Korea: An Integrative Review" Healthcare 4, no. 3: 52. https://doi.org/10.3390/healthcare4030052






