What Are the Ethical Issues Facing Global-Health Trainees Working Overseas? A Multi-Professional Qualitative Study
Abstract
:1. Introduction
2. Methods
2.1. Setting
2.2. Sample and Recruitment
2.3. Data Collection
2.4. Data Analysis
3. Results
3.1. Participants
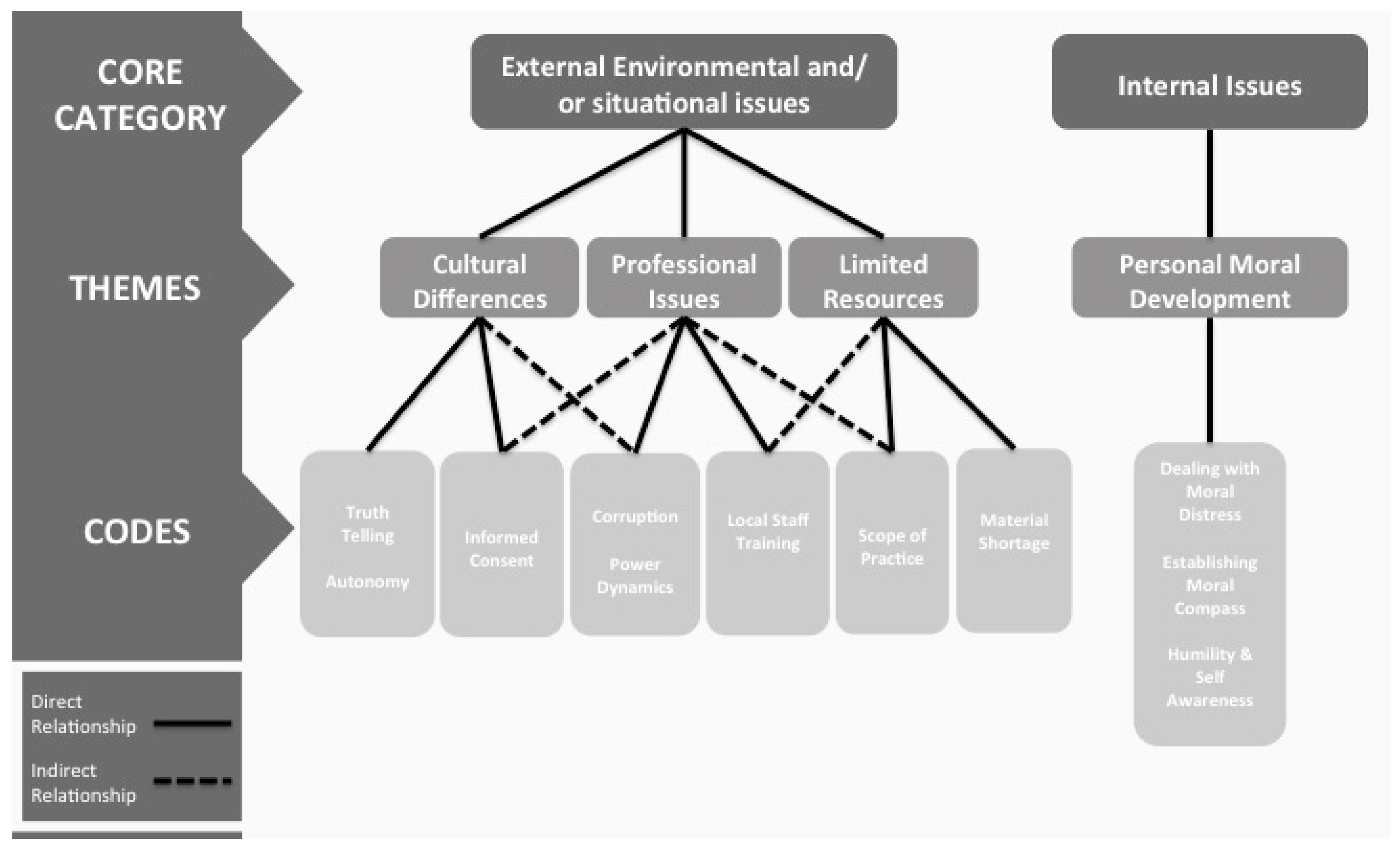
3.2. Key Ethical Themes and Topics
3.2.1. Theme 1: Cultural Differences (Codes Include Informed Consent, Truth-Telling, and Autonomy)
“[…] that the beneficent thing to do is to withhold that information if the family is saying, “No, he can’t handle this. […] In that case, culturally, beneficence outweighs autonomy in most scenarios.”.(Medicine Physician)
“…informed consent is a big issue… it goes back to what the cultural practice has dictated for so many years”.(Nursing)
“It’s important to respect whoever’s practice you are interacting with”.(Pharmacist)
“[Where I worked], if you ask the patient, they will say, ‘Absolutely not. You are telling me there’s a risk in the procedure? I don’t want it.’”.(Medicine Physician)
“Places where, for example, the word, autonomy, it’s like you can’t come up with a good translation for it. There’s just no word for it!”.(Anthropologist)
3.2.2. Theme 2: Professional Issues: (Codes Include Power Dynamics, Extent of Training of Local Staff, Perceived Corruption)
“[…] these were mostly physicians, and I was the only nurse there. […] So I said ‘I wonder if [the traditional vaccinations] would also facilitate HIV transmission.’ And somebody at the table said, ‘Okay, we’re going to make a policy that nobody can give traditional vaccinations!’”.(Nurse)
“The scope of practice is constantly changing in the global setting. […] Nurses in [resource limited country] now, are doing Cesarean sections, are the prescribers of anti-retroviral therapy” […].(Nurse)
“So many of the countries I’ve worked in have so few actual pharmacists, but they still have to have people to provide medicine. So you may be working with someone who you feel hasn’t gone through as much formal training as you might expect in the U.S.”.(Pharmacist)
“We had a similar situation there where we were going to collaborate with the department of public health to do the initial survey. They basically demanded a bribe, which was not small”.(Pharmacist)
“They basically wanted us to pay them a fee, which was quite a hefty fee, in order for us to utilize them as a site. And they were saying that fee was for the ethics committee”.(Pharmacist)
3.2.3. Theme 3: Limited Resources (Codes Include Scope of Practice, Material Shortage)
“We knew that likely this patient would die without a pericardiocentesis. […] Theoretically, we could have done it, and there was nowhere else to send the patient. But we decided that, because we had never done one, that we shouldn’t risk it. And the patient died overnight”.(Medicine Physician)
“The scope of practice is constantly changing in the global setting. So the scope of practice for nurses is constantly changing”.(Nursing)
“So in a limited-resource environment, even though it is something that can be reversed as easily as getting blood, [it] is sometimes delayed and people die because there is no blood or they’re trying to save it for a different case”.(Pharmacist)
“I didn’t even know how to practice in that setting. There are no supplies. There are no blood pressure cuffs. There are no gloves. I couldn’t walk in there and do anything at the hospital”.(Nursing)
“When I was on the wards in [host site] in January, there were a number of [U.S. Medical School] medical students and residents there and they all had on facemasks and they were the only ones on the ward. None of the other staff were wearing masks. And I was standing there with two medical students from somewhere else and thinking to ourselves, what should we do? …The wards are filled with HIV/TB patients, who are coughing”.(Medicine Physician)
3.2.4. Theme 4: Personal Moral Development: (Codes Include Dealing with Moral Distress, Establishing a Moral Compass, Humility and Self-Awareness)
“That’s what we’re not trained to deal with either: how that’s going to impact us emotionally and what’s our role in all that?”.(Nurse)
“It may not be sustainable once we walk out the door, so do we save the person’s life at that moment or do we just continue to try and train people there about how to care for people? It’s upsetting”.(Nurse)
“I think that the long-term consequences of that, mental health and other consequences for our students in particular, are really bad”.(Medicine Physician)
“If you consistently have moral distress even though you are doing the things that all the principles tell you […] part of what happens in ethical practice is figuring out what resonates with who you are as a human being. […] The idea is that you eventually develop this compass of practice.”.(Medicine Physician)
“…what makes you a great medical student in the States often makes you slightly obnoxious abroad. Try to have humility and awareness”.(Medicine Physician)
“The trainees that I work with are mainly integrated in the programs and they’re getting certain skills, and they know they are going to work in the field long term. So I think they feel a little less distressed because they feel a little empowered.”.(Medicine Physician)
4. Discussion
5. Conclusions
Acknowledgments
Author Contribution
Conflicts of Interest
References
- Battat, R.; Seidman, G.; Chadi, N.; Chanda, M.Y.; Nehme, J.; Hulme, J.; Li, A.; Faridi, N.; Brewer, T.F. Global health competencies and approaches in medical education: A literature review. BMC Med. Educ. 2010. [Google Scholar] [CrossRef] [PubMed]
- Drain, P.K.; Holmes, K.K.; Skeff, K.M.; Hall, T.L.; Gardner, P. Global health training and international clinical rotations during residency: Current status, needs and opportunities. Acad. Med. 2009, 84, 320–325. [Google Scholar] [CrossRef] [PubMed]
- Provenzano, A.M.; Graber, L.K.; Elansary, M.; Khoshnood, K.; Rastegar, A.; Barry, M. Short term global health research projects by U.S. medical students: Ethical challenges and partnerships. Am. J. Trop. Med. Hyg. 2010, 83, 211–214. [Google Scholar] [CrossRef] [PubMed]
- Callister, L.C.; Cox, A.H. Opening our hearts and minds: The meaning of international clinical nursing electives in the personal and professional lives of nurses. Nurs. Health Sci. 2006, 8, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Brook, S.; Robertson, D.; Makuwaza, T.; Hodges, B. Canadian residents teaching and learning psychiatry in Ethiopia. Acad. Psychiatry 2010, 34, 433–437. [Google Scholar] [CrossRef] [PubMed]
- Elit, L.; Hunt, M.; Redwood-Campbell, L.; Ranford, J.; Adelson, N.; Schwartz, L. Ethical issues encountered by medical students during international health electives. Med. Educ. 2011, 45, 704–711. [Google Scholar] [CrossRef] [PubMed]
- Abedini, N.C.; Gruppen, L.D.; Kolars, J.C.; Kumagai, A.K. Understanding the effects of short term international service-learning tips on medical students. Acad. Med. 2012, 87, 820–828. [Google Scholar] [CrossRef] [PubMed]
- Izadnegahdar, R.; Correia, S.; Ohata, B.; Kuile, S.; Vaillancourt, S.; Saba, N.; Brewer, T.F. Global health in Canadian practices and opportunities. Acad. Med. 2008, 83, 192–198. [Google Scholar] [CrossRef] [PubMed]
- Crump, J.A.; Sugarman, J.; Working Group on Ethics Guidelines for Global Health Training (WEIGHT). Ethics and best practice guidelines for training experiences in global health. Am. J. Trop. Med. Hyg. 2010, 83, 1178–1182. [Google Scholar] [CrossRef] [PubMed]
- Lahey, T. A proposed medical school curriculum to help students recognize and resolve ethical issues of global health outreach work. Acad. Med. 2012, 87, 210–215. [Google Scholar] [CrossRef] [PubMed]
- Pinto, A.D.; Upshur, R.E. Global health ethics for students. Dev. World Bioeth. 2009, 9, 1–10. [Google Scholar] [CrossRef] [PubMed]
- John Hopkins Berman Institute of Bioethics & Stanford Center for Innovation in Global Health. Ethical challenges in short-term global health training. Available online: http://ethicsandglobalhealth.org/index.shtml (accessed on 23 June 2016).
- Stanford Center for Innovation in Global Health. Ethical challenges in short-term global health training. Available online: http://globalhealth.stanford.edu/education/cigh-sponsored-courses/ethical-challenges.html (accessed on 23 June 2016).
- Addo-Atuah, J.; Dutta, A.; Kovera, C. A global health elective course for PharmD Curriculum. Am. J. Pharm. Educ. 2014, 78. [Google Scholar] [CrossRef] [PubMed]
- Butteris, S.M.; Gladding, S.P.; Eppich, W.; Hagen, S.A.; Pitt, M.B.; Sugar Investigators. Simulation use for global away rotations (SUGAR): Preparing residents for emotional challenges abroad—A multicenter study. Acad. Pediatr. 2014, 14, 533–541. [Google Scholar] [CrossRef] [PubMed]
- Elansary, M.; Kallem, S.; Peluso, M.; Thomas, J.; Rabin, T. Global health clinical ethics. MedEdPORTAL Publications 2015. [Google Scholar] [CrossRef]
- Goodman, L.A. Snowball sampling. Ann. Math. Statist. 1961, 32, 148–170. [Google Scholar] [CrossRef]
- Abdul-Quader, A.S.; Heckathorn, D.D.; McKnight, C.; Bramson, H.; Nemeth, C.; Sabin, K.; Gallagher, K.; Des Jarlais, D.C. Effectiveness of a responder driven sampling for recruiting drug users in New York City: Findings from a pilot study. J. Urban Health 2006, 83, 459–476. [Google Scholar] [CrossRef] [PubMed]
- Strauss, A.; Corbin, J. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory; SAGE Publications: Thousand Oaks, CA, USA, 2008. [Google Scholar]
- Price, J. Coding: Open coding. In Encyclopedia of Case Study Research; Mills, A., Durepos, G., Wiebe, E., Eds.; SAGE Publications: Thousand Oaks, CA, USA, 2010; pp. 156–158. [Google Scholar]
- Wicks, D. Coding: Axial coding. In Encyclopedia of Case Study Research; Mills, A., Durepos, G., Wiebe, E., Eds.; SAGE Publications: Thousand Oaks, CA, USA, 2010; pp. 154–156. [Google Scholar]
- Bradley, E.H.; Curry, L.A.; Devers, K.J. Qualitative data analysis for health services research: Developing taxonomy, themes and theory. Health Serv. Res. 2007, 42, 1758–1772. [Google Scholar] [CrossRef] [PubMed]
- Jameton, A. Nursing Practice: The Ethical Issues; Prentice-Hall: Englewood Cliffs, NJ, USA, 1984. [Google Scholar]
- Elansary, M.; Graber, L.K.; Provenzano, A.M.; Barry, M.; Khoshnood, K.; Rastegar, A. Ethical dilemmas in global clinical electives. Available online: http://www.ghjournal.org/ethical-dilemmas-in-global-clinical-electives/ (accessed on 23 June 2016).
- DeCamp, M.; Rodriguez, J.; Hecht, S.; Barry, M.; Sugarman, J. An ethics curriculum for short-term global health trainees. Globalization Health 2013. [Google Scholar] [CrossRef] [PubMed]
- Radstone, S.J.J. Practising on the poor? Healthcare workers beliefs about the role of medical students during their electives. J. Med. Ethics 2005, 31, 109–110. [Google Scholar] [CrossRef] [PubMed]
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Harrison, J.D.; Logar, T.; Le, P.; Glass, M. What Are the Ethical Issues Facing Global-Health Trainees Working Overseas? A Multi-Professional Qualitative Study. Healthcare 2016, 4, 43. https://doi.org/10.3390/healthcare4030043
Harrison JD, Logar T, Le P, Glass M. What Are the Ethical Issues Facing Global-Health Trainees Working Overseas? A Multi-Professional Qualitative Study. Healthcare. 2016; 4(3):43. https://doi.org/10.3390/healthcare4030043
Chicago/Turabian StyleHarrison, James D., Tea Logar, Phuoc Le, and Marcia Glass. 2016. "What Are the Ethical Issues Facing Global-Health Trainees Working Overseas? A Multi-Professional Qualitative Study" Healthcare 4, no. 3: 43. https://doi.org/10.3390/healthcare4030043
APA StyleHarrison, J. D., Logar, T., Le, P., & Glass, M. (2016). What Are the Ethical Issues Facing Global-Health Trainees Working Overseas? A Multi-Professional Qualitative Study. Healthcare, 4(3), 43. https://doi.org/10.3390/healthcare4030043




