Effects of Real-Time Feedback Methods on Static Balance Training in Stroke Patients: A Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
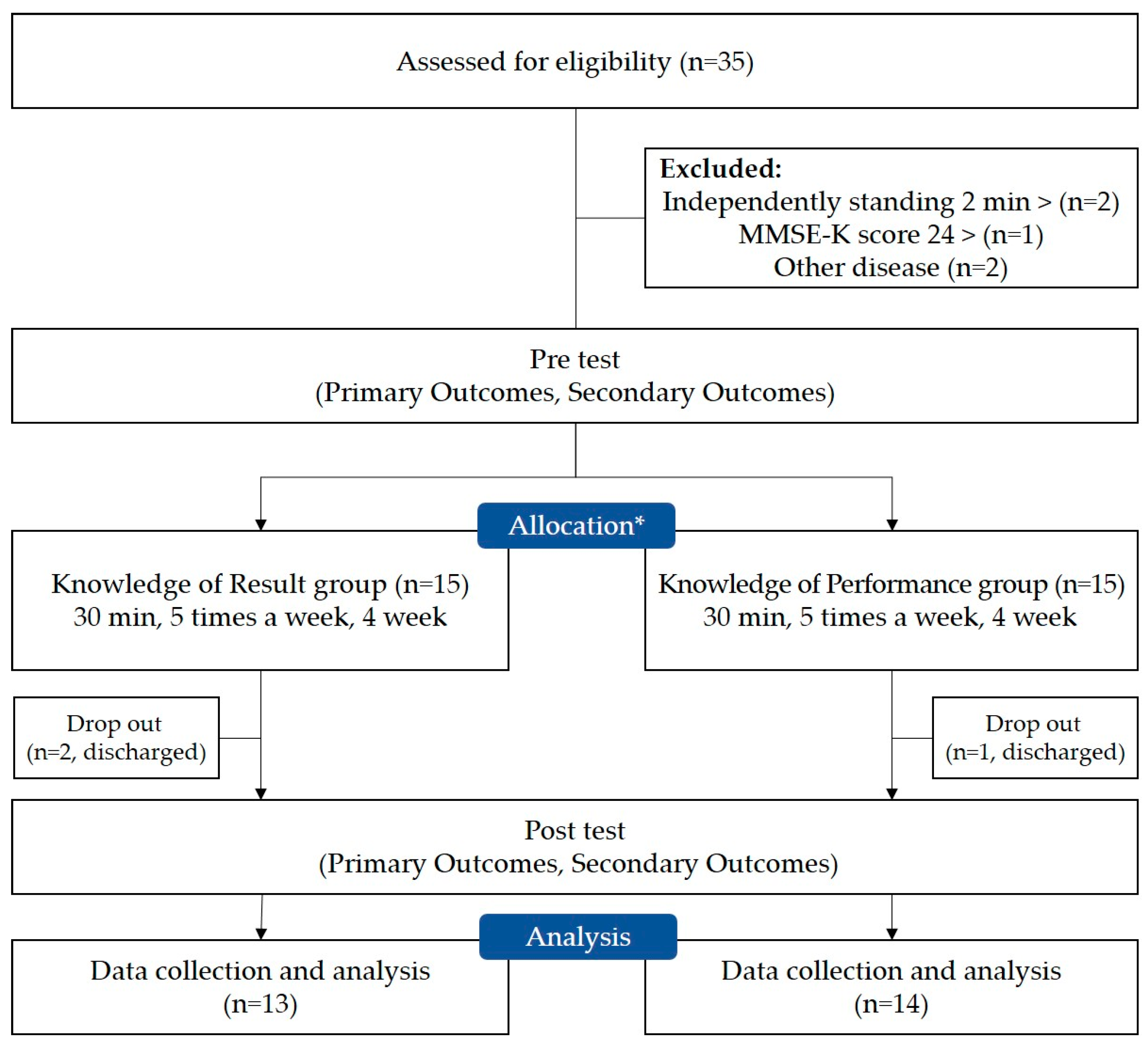
2.1. Study Design
2.2. Participants
2.3. Outcome Measures
2.3.1. Primary Outcomes (Kinematic Data)
2.3.2. Secondary Outcomes (Clinical Data)
2.4. Interventions
2.5. Statistical Analysis
3. Results
3.1. General Characteristic of the Subjects
3.2. Primary Outcome Measures
3.3. Secondary Outcome Measures
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Garay-Sánchez, A.; Suarez-Serrano, C.; Ferrando-Margelí, M.; Jimenez-Rejano, J.J.; Marcén-Román, Y. Effects of Immersive and Non-Immersive Virtual Reality on the Static and Dynamic Balance of Stroke Patients: A Systematic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 4473. [Google Scholar] [CrossRef]
- Hyun, S.-J.; Lee, J.; Lee, B.-H. The Effects of Sit-to-Stand Training Combined with Real-Time Visual Feedback on Strength, Balance, Gait Ability, and Quality of Life in Patients with Stroke: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2021, 18, 12229. [Google Scholar] [CrossRef] [PubMed]
- Gordt, K.; Gerhardy, T.; Najafi, B.; Schwenk, M. Effects of Wearable Sensor-Based Balance and Gait Training on Balance, Gait, and Functional Performance in Healthy and Patient Populations: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Gerontology 2017, 64, 74–89. [Google Scholar] [CrossRef] [PubMed]
- Jang, S.H.; Lee, J.-H. Impact of sensory integration training on balance among stroke patients: Sensory integration training on balance among stroke patients. Open Med. 2016, 11, 330–335. [Google Scholar] [CrossRef]
- Campfens, S.F.; Zandvliet, S.B.; Meskers, C.G.M.; Schouten, A.C.; van Putten, M.J.A.M.; van der Kooij, H. Poor motor function is associated with reduced sensory processing after stroke. Exp. Brain Res. 2015, 233, 1339–1349. [Google Scholar] [CrossRef]
- Freburger, J.K.; Li, D.; Johnson, A.M.; Fraher, E.P. Physical and Occupational Therapy From the Acute to Community Setting After Stroke: Predictors of Use, Continuity of Care, and Timeliness of Care. Arch. Phys. Med. Rehabil. 2018, 99, 1077–1089. [Google Scholar] [CrossRef] [PubMed]
- Li, S. Spasticity, Motor Recovery, and Neural Plasticity after Stroke. Front. Neurol. 2017, 8, 120. [Google Scholar] [CrossRef] [PubMed]
- Hugues, A.; Di Marco, J.; Janiaud, P.; Xue, Y.; Pires, J.; Khademi, H.; Cucherat, M.; Bonan, I.; Gueyffier, F.; Rode, G. Efficiency of physical therapy on postural imbalance after stroke: Study protocol for a systematic review and meta-analysis. BMJ Open 2017, 7, e013348. [Google Scholar] [CrossRef]
- Hussein, Z.A.; Salem, I.A.; Ali, M.S. Effect of simultaneous proprioceptive-visual feedback on gait of children with spastic diplegic cerebral palsy. J. Musculoskelet. Neuronal Interact. 2019, 19, 500–506. [Google Scholar]
- Lakhani, B.; Mansfield, A. Visual feedback of the centre of gravity to optimize standing balance. Gait Posture 2015, 41, 499–503. [Google Scholar] [CrossRef]
- Bishop, J.C.; Kelly, L.E.; Hull, M. Knowledge of performance feedback among boys with ADHD. Res. Dev. Disabil. 2018, 74, 31–40. [Google Scholar] [CrossRef] [PubMed]
- Oppici, L.; Dix, A.; Narciss, S. When is knowledge of performance (KP) superior to knowledge of results (KR) in promoting motor skill learning? A systematic review. Int. Rev. Sport Exerc. Psychol. 2021, 1–25. [Google Scholar] [CrossRef]
- Komiya, M.; Maeda, N.; Narahara, T.; Suzuki, Y.; Fukui, K.; Tsutsumi, S.; Yoshimi, M.; Ishibashi, N.; Shirakawa, T.; Urabe, Y. Effect of 6-Week Balance Exercise by Real-Time Postural Feedback System on Walking Ability for Patients with Chronic Stroke: A Pilot Single-Blind Randomized Controlled Trial. Brain Sci. 2021, 11, 1493. [Google Scholar] [CrossRef] [PubMed]
- Bae, S.; Lee, J.; Lee, B.-H. Effect of an EMG–FES Interface on Ankle Joint Training Combined with Real-Time Feedback on Balance and Gait in Patients with Stroke Hemiparesis. Healthcare 2020, 8, 292. [Google Scholar] [CrossRef] [PubMed]
- Shim, D.; Park, D.; Yoo, B.; Choi, J.; Hong, J.; Choi, T.Y.; Park, E.S.; Rha, D. Evaluation of sitting and standing postural balance in cerebral palsy by center-of-pressure measurement using force plates: Comparison with clinical measurements. Gait Posture 2022, 92, 110–115. [Google Scholar] [CrossRef] [PubMed]
- Karasu, A.; Batur, E.; Karataş, G. Effectiveness of Wii-based rehabilitation in stroke: A randomized controlled study. J. Rehabil. Med. 2018, 50, 406–412. [Google Scholar] [CrossRef] [PubMed]
- Chen, B.; Liu, P.; Xiao, F.; Liu, Z.; Wang, Y. Review of the Upright Balance Assessment Based on the Force Plate. Int. J. Environ. Res. Public Health 2021, 18, 2696. [Google Scholar] [CrossRef] [PubMed]
- Hill, M.W.; Roberts, M.; Price, M.J.; Kay, A.D. Association between knee extensor and ankle plantarflexor muscle thickness and echo intensity with postural sway, mobility and physical function in older adults. Exp. Gerontol. 2021, 150, 111385. [Google Scholar] [CrossRef] [PubMed]
- Jung, H.; Park, J.; Shim, J.; Kim, M.; Hwang, M.; Kim, S. Reliability Test of Korean Version of Berg Balance Scale. Ann. Rehabil. Med. 2006, 30, 611–618. [Google Scholar]
- Yang, H.; Lee, C.; Lin, R.; Hsu, M.; Chen, C.; Lin, J.; Lo, S.K. Effect of biofeedback cycling training on functional recovery and walking ability of lower extremity in patients with stroke. Kaohsiung J. Med. Sci. 2013, 30, 35–42. [Google Scholar] [CrossRef]
- An, S.; Lee, J. Reliability and Validity of the Postural Assessment Scale for Stroke in Chronic Stroke Patients. J. Korean Soc. Phys. Ther. 2009, 21, 9–17. [Google Scholar]
- Ko, J.; You, Y. Reliability and Responsiveness of the Korean Version of the Trunk Impairment Scale for Stroke Patients. J. Korean Soc. Phys. Ther. 2015, 27, 175–182. [Google Scholar] [CrossRef]
- Jang, S.; Cho, S.; Ou, S.; Lee, E.; Baik, H. The Validity and Reliability of Korean Fall Efficacy Scale (FES) and Activities-specific Balance Confidence Scale (ABC). J. Korean Geriatr. Soc. 2003, 7, 255–268. [Google Scholar]
- Pignolo, L.; Basta, G.; Carozzo, S.; Bilotta, M.; Todaro, M.R.; Serra, S.; Ciancarelli, I.; Tonin, P.; Cerasa, A. A body-weight-supported visual feedback system for gait recovering in stroke patients: A randomized controlled study. Gait Posture 2020, 82, 287–293. [Google Scholar] [CrossRef]
- Shin, D.C.; Song, C.H. Smartphone-Based Visual Feedback Trunk Control Training Using a Gyroscope and Mirroring Technology for Stroke Patients. Am. J. Phys. Med. Rehabil. 2016, 95, 319–329. [Google Scholar] [CrossRef] [PubMed]
- Cheng, P.-T.; Wang, C.-M.; Chung, C.-Y.; Chen, C.-L. Effects of visual feedback rhythmic weight-shift training on hemiplegic stroke patients. Clin. Rehabil. 2004, 18, 747–753. [Google Scholar] [CrossRef] [PubMed]
- Kilby, M.C.; Molenaar, P.C.M.; Slobounov, S.M.; Newell, K.M. Real-time visual feedback of COM and COP motion properties differentially modifies postural control structures. Exp. Brain Res. 2016, 235, 109–120. [Google Scholar] [CrossRef] [PubMed]
- Deutsch, J.E.; Brettler, A.; Smith, C.; Welsh, J.; John, R.; Guarrera-Bowlby, P.; Kafri, M. Nintendo Wii Sports and Wii Fit Game Analysis, Validation, and Application to Stroke Rehabilitation. Top. Stroke Rehabil. 2011, 18, 701–719. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, K.; Krauskopf, T.; Lauck, T.B.; Klein, L.; Mueller, M.; Herget, G.W.; Von Tscharner, V.; Stutzig, N.; Stieglitz, T.; Pasluosta, C. Influence of Augmented Visual Feedback on Balance Control in Unilateral Transfemoral Amputees. Front. Neurosci. 2021, 15, 727527. [Google Scholar] [CrossRef]
- Pellegrino, L.; Giannoni, P.; Marinelli, L.; Casadio, M. Effects of continuous visual feedback during sitting balance training in chronic stroke survivors. J. NeuroEng. Rehabil. 2017, 14, 107. [Google Scholar] [CrossRef]
- In, T.; Lee, K.; Song, C. Virtual Reality Reflection Therapy Improves Balance and Gait in Patients with Chronic Stroke: Randomized Controlled Trials. Med. Sci. Monit. 2016, 22, 4046–4053. [Google Scholar] [CrossRef] [PubMed]
- Sousa, C.O.; Barela, J.A.; Prado-Medeiros, C.L.; Salvini, T.F.; Barela, A.M. Gait training with partial body weight support during overground walking for individuals with chronic stroke: A pilot study. J. NeuroEng. Rehabil. 2011, 8, 48. [Google Scholar] [CrossRef] [PubMed]
- Hornby, T.G.; Reisman, D.S.; Ward, I.G.; Scheets, P.L.; Miller, A.; Haddad, D.; Fox, E.J.; Fritz, N.E.; Hawkins, K.; Henderson, C.E.; et al. Clinical Practice Guideline to Improve Locomotor Function Following Chronic Stroke, Incomplete Spinal Cord Injury, and Brain Injury. J. Neurol. Phys. Ther. 2020, 44, 49–100. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.J.; Yoon, S.; Kang, J.J.; Kim, J.; Kim, J.M.; Han, J.Y. Efficacy and Safety of Caregiver-Mediated Exercise in Post-stroke Rehabilitation. Ann. Rehabil. Med. 2018, 42, 406–415. [Google Scholar] [CrossRef]

| Variable | KR Group (n = 13) | KP Group (n = 14) | p |
|---|---|---|---|
| Sex (male/female) | 9/4 | 9/5 | 0.785 a |
| Paretic side (left/right) | 7/6 | 8/6 | 0.863 a |
| Type (infarction/hemorrhages) | 9/4 | 5/9 | 0.082 a |
| Disease duration (months) | 24.92 ± 14.86 | 19.35 ± 15.27 | 0.347 b |
| Age (years) | 64.53 ± 12.35 | 63.14 ± 12.08 | 0.769 b |
| Height (cm) | 168.62 ± 8.84 | 164.29 ± 8.88 | 0.217 b |
| Body mass (kg) | 68.69 ± 7.88 | 65.86 ± 10.95 | 0.451 b |
| Variable | State | Group | Pre | Post | Time | Group × Time |
|---|---|---|---|---|---|---|
| F (p) | F (p) | |||||
| Sway Length (cm) | EO | KR | 387.28 ± 91.62 | 320.33 ± 97.91 | 54.614 (0.000) * | 5.398 (0.029) * |
| KP | 402.71 ± 45.86 | 367.78 ± 75.87 | ||||
| EC | KR | 433.82 ± 113.66 | 395.60 ± 112.04 | 52.323 (0.000) * | 1.444 (0.241) | |
| KP | 443.66 ± 81.42 | 410.92 ± 80.26 | ||||
| Sway Velocity (cm/s) | EO | KR | 6.35 ± 0.54 | 5.97 ± 0.41 | 40.735 (0.000) * | 0.108 (0.745) |
| KP | 6.73 ± 0.62 | 6.33 ± 0.50 | ||||
| EC | KR | 7.25 ± 0.64 | 6.90 ± 0.63 | 57.357 (0.000) * | 0.065 (0.801) | |
| KP | 6.76 ± 0.74 | 6.44 ± 0.63 | ||||
| Area 95% (cm2) | EO | KR | 4.10 ± 1.09 | 2.92 ± 1.14 | 113.023 (0.000) * | 7.106 (0.013) * |
| KP | 3.38 ± 1.15 | 2.67 ± 1.11 | ||||
| EC | KR | 6.51 ± 1.63 | 5.28 ± 1.65 | 62.656 (0.000) * | 0.589 (0.450) | |
| KP | 6.70 ± 2.79 | 5.69 ± 2.44 |
| Variable | Group | Pre | Post | Time | Group × Time |
|---|---|---|---|---|---|
| F (p) | F (p) | ||||
| BBS (score) | KR | 31.84 ± 9.40 | 38.07 ± 10.59 | 83.037 (0.000) * | 0.559 (0.462) |
| KP | 32.14 ± 10.60 | 37.42 ± 10.29 | |||
| FMA-LE (score) | KR | 19.23 ± 7.81 | 29.92 ± 10.51 | 37.101 (0.000) * | 4.100 (0.054) |
| KP | 27.50 ± 8.02 | 32.85 ± 7.99 | |||
| PASS (score) | KR | 26.23 ± 7.40 | 29.46 ± 6.23 | 27.821 (0.000) * | 1.772 (0.195) |
| KP | 28.00 ± 6.73 | 29.92 ± 6.39 | |||
| TIS (score) | KR | 15.76 ± 2.65 | 18.92 ± 2.59 | 62.510 (0.000) * | 0.152 (0.700) |
| KP | 16.21 ± 4.04 | 19.07 ± 3.07 | |||
| FES (score) | KR | 58.00 ± 22.20 | 63.84 ± 21.10 | 79.329 (0.000) * | 0.575 (0.455) |
| KP | 63.00 ± 19.93 | 67.92 ± 20.95 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwon, I.-H.; Shin, W.-S.; Choi, K.-S.; Lee, M.-S. Effects of Real-Time Feedback Methods on Static Balance Training in Stroke Patients: A Randomized Controlled Trial. Healthcare 2024, 12, 767. https://doi.org/10.3390/healthcare12070767
Kwon I-H, Shin W-S, Choi K-S, Lee M-S. Effects of Real-Time Feedback Methods on Static Balance Training in Stroke Patients: A Randomized Controlled Trial. Healthcare. 2024; 12(7):767. https://doi.org/10.3390/healthcare12070767
Chicago/Turabian StyleKwon, Il-Ho, Won-Seob Shin, Kyu-Seong Choi, and Myung-Sun Lee. 2024. "Effects of Real-Time Feedback Methods on Static Balance Training in Stroke Patients: A Randomized Controlled Trial" Healthcare 12, no. 7: 767. https://doi.org/10.3390/healthcare12070767







