Burden and Trend of Macrosomia and Large-for-Gestational-Age Neonates Attributable to High Pre-Pregnancy Body Mass Index in China, 2013–2017: A Population-Based Retrospective Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Setting
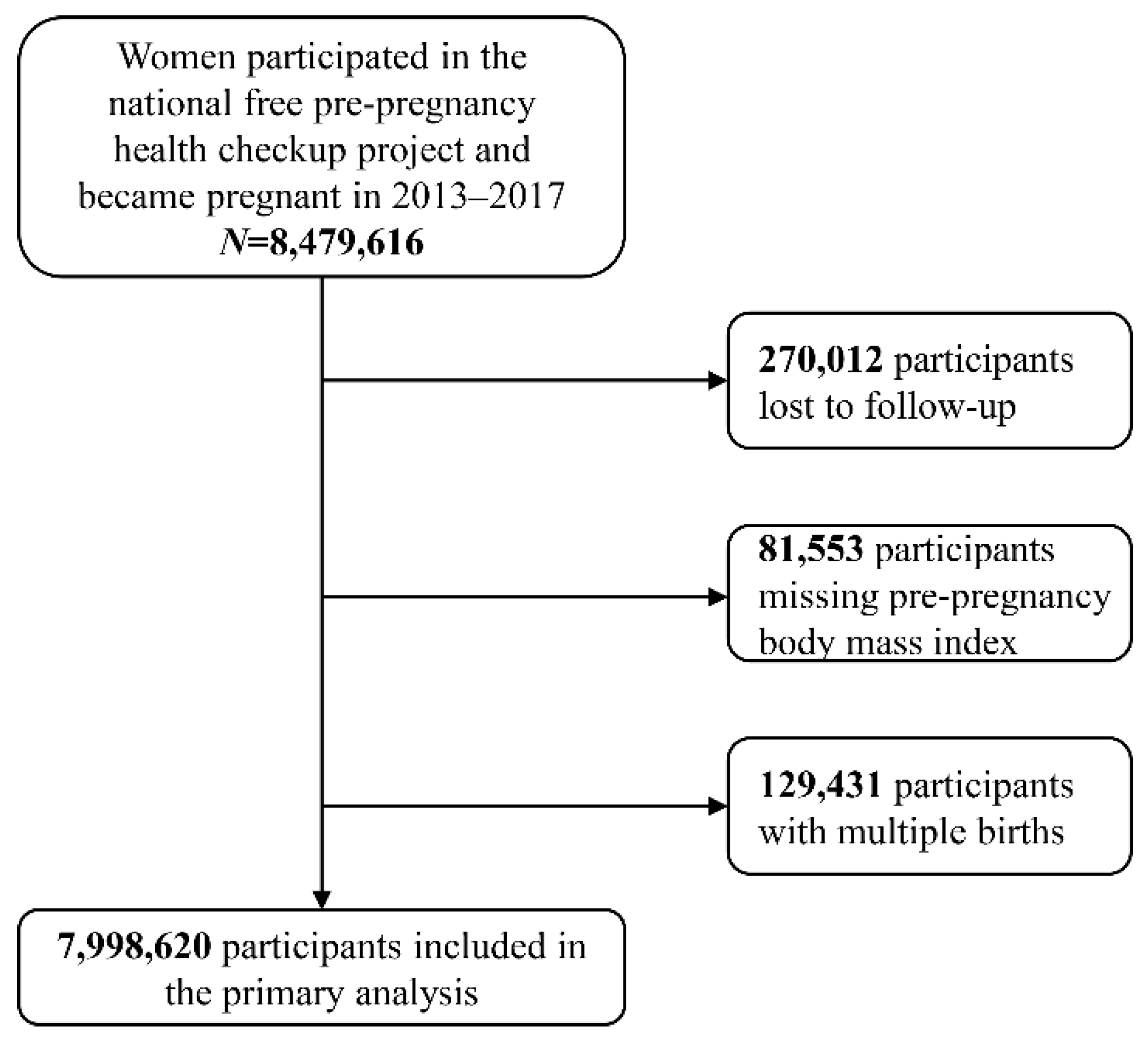
2.2. Study Population
2.3. Exposure and Outcomes
2.4. Covariates
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| LGA | Large-for-gestational-age |
| BMI | Body mass index |
| NFPCP | National Free Pre-Pregnancy Check-ups Project |
| WHO | World Health Organization |
| LMP | Last menstrual period |
| RR | Relative risk |
| CI | Confidence interval |
| PAF | Population attributable fraction |
| APC | Annual percent change |
| CCDRFS | China Chronic Disease and Risk Factors Surveillance |
References
- Viswanathan, S.; McNelis, K.; Makker, K.; Calhoun, D.; Woo, J.G.; Balagopal, B. Childhood obesity and adverse cardiometabolic risk in large for gestational age infants and potential early preventive strategies: A narrative review. Pediatr. Res. 2021, 92, 653–661. [Google Scholar] [CrossRef] [PubMed]
- Warrington, N.M.; Beaumont, R.N.; Horikoshi, M.; Day, F.R.; Helgeland, Ø.; Laurin, C.; Bacelis, J.; Peng, S.; Hao, K.; Feenstra, B.; et al. Maternal and fetal genetic effects on birth weight and their relevance to cardio-metabolic risk factors. Nat. Genet. 2019, 51, 804–814. [Google Scholar] [CrossRef]
- Pirkola, J.; Pouta, A.; Bloigu, A.; Hartikainen, A.-L.; Laitinen, J.; Järvelin, M.-R.; Vääräsmäki, M. Risks of overweight and abdominal obesity at age 16 years associated with prenatal exposures to maternal prepregnancy overweight and gestational diabetes mellitus. Diabetes Care 2010, 33, 1115–1121. [Google Scholar] [CrossRef] [Green Version]
- Koyanagi, A.; Zhang, J.; Dagvadorj, A.; Hirayama, F.; Shibuya, K.; Souza, J.P.; Gülmezoglu, A.M. Macrosomia in 23 developing countries: An analysis of a multicountry, facility-based, cross-sectional survey. Lancet 2013, 381, 476–483. [Google Scholar] [CrossRef] [PubMed]
- Orskou, J.; Kesmodel, U.; Henriksen, T.B.; Secher, N.J. An increasing proportion of infants weigh more than 4000 grams at birth. Acta Obstet. Gynecol. Scand. 2001, 80, 931–936. [Google Scholar]
- Harvey, L.; van Elburg, R.; van der Beek, E.M. Macrosomia and large for gestational age in Asia: One size does not fit all. J. Obstet. Gynaecol. Res. 2021, 47, 1929–1945. [Google Scholar] [CrossRef] [PubMed]
- Henriksen, T. The macrosomic fetus: A challenge in current obstetrics. Acta Obstet. Gynecol. Scand. 2008, 87, 134–145. [Google Scholar] [CrossRef] [PubMed]
- Garmendia, M.L.; Casanello, P.; Flores, M.; Kusanovic, J.P.; Uauy, R. The effects of a combined intervention (docosahexaenoic acid supplementation and home-based dietary counseling) on metabolic control in obese and overweight pregnant women: The MIGHT study. Am. J. Obstet. Gynecol. 2021, 224, 526.e1–526.e25. [Google Scholar] [CrossRef]
- Poston, L.; Caleyachetty, R.; Cnattingius, S.; Corvalan, C.; Uauy, R.; Herring, S.; Gillman, M.W. Preconceptional and maternal obesity: Epidemiology and health consequences. Lancet Diabetes Endocrinol. 2016, 4, 1025–1036. [Google Scholar] [CrossRef]
- Bluher, M. Obesity: Global epidemiology and pathogenesis. Nat. Rev. Endocrinol. 2019, 15, 288–298. [Google Scholar] [CrossRef]
- Wang, L.; Zhou, B.; Zhao, Z.; Yang, L.; Zhang, M.; Jiang, Y.; Li, Y.; Zhou, M.; Wang, L.; Huang, Z.; et al. Body-mass index and obesity in urban and rural China: Findings from consecutive nationally representative surveys during 2004–2018. Lancet 2021, 398, 53–63. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Wang, Q.; Shen, H. [Design of the national free proception health examination project in China]. Zhonghua Yi Xue Za Zhi 2015, 95, 162–165. [Google Scholar] [PubMed]
- World Health Organization. Obesity and Overweight. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 9 June 2021).
- Delpapa, E.H.; Mueller-Heubach, E. Pregnancy outcome following ultrasound diagnosis of macrosomia. Obstet. Gynecol. 1991, 78, 340–343. [Google Scholar] [PubMed]
- McGrath, R.T.; Glastras, S.J.; Hocking, S.L.; Fulcher, G.R. Large-for-Gestational-Age Neonates in Type 1 Diabetes and Pregnancy: Contribution of Factors Beyond Hyperglycemia. Diabetes Care 2018, 41, 1821–1828. [Google Scholar] [CrossRef] [Green Version]
- China Statistical Yearbook 2016. Available online: http://www.stats.gov.cn/tjsj/ndsj/2016/indexeh.htm(accessed on 2016).
- China Business Network. Ranking of Cities’ Business Attractiveness in China 2020. Available online: https://www.yicai.com/brief/100648804.html (accessed on 29 May 2020).
- Rockhill, B.; Newman, B.; Weinberg, C. Use and misuse of population attributable fractions. Am. J. Public Health 1998, 88, 15–19. [Google Scholar] [CrossRef] [Green Version]
- Cheney, K.; Farber, R.; Barratt, A.L.; McGeechan, K.; de Vries, B.; Ogle, R.; Black, K. Population attributable fractions of perinatal outcomes for nulliparous women associated with overweight and obesity, 1990–2014. Med. J. Aust. 2018, 208, 119–125. [Google Scholar] [CrossRef]
- MacInnis, N.; Woolcott, C.G.; McDonald, S.; Kuhle, S. Population Attributable Risk Fractions of Maternal Overweight and Obesity for Adverse Perinatal Outcomes. Sci. Rep. 2016, 6, 22895. [Google Scholar] [CrossRef] [Green Version]
- Djelantik, A.A.A.M.J.; Kunst, A.E.; van der Wal, M.F.; Smit, H.A.; Vrijkotte, T.G.M. Contribution of overweight and obesity to the occurrence of adverse pregnancy outcomes in a multi-ethnic cohort: Population attributive fractions for Amsterdam. BJOG-Int. J. Obstet. Gynecol. 2012, 119, 283–290. [Google Scholar] [CrossRef]
- Sugimura, R.; Kohmura-Kobayashi, Y.; Narumi, M.; Furuta-Isomura, N.; Oda, T.; Tamura, N.; Uchida, T.; Suzuki, K.; Sugimura, M.; Kanayama, N.; et al. Comparison of three classification systems of Prepregnancy Body Mass Index with Perinatal Outcomes in Japanese Obese Pregnant Women: A retrospective study at a single center. Int. J. Med. Sci. 2020, 17, 2002–2012. [Google Scholar] [CrossRef]
- Choi, H.; Lim, J.Y.; Lim, N.K.; Ryu, H.M.; Kwak, D.W.; Chung, J.H.; Park, H.J.; Park, H.-Y. Impact of pre-pregnancy body mass index and gestational weight gain on the risk of maternal and infant pregnancy complications in Korean women. Int. J. Obes. 2022, 46, 59–67. [Google Scholar] [CrossRef]
- Choi, S.K.; Park, I.Y.; Shin, J.C. The effects of pre-pregnancy body mass index and gestational weight gain on perinatal outcomes in Korean women: A retrospective cohort study. Reprod. Biol. Endocrinol. 2011, 9, 6. [Google Scholar] [CrossRef] [PubMed]
- Lu, J.; Bi, Y.; Ning, G. Curbing the obesity epidemic in China. Lancet Diabetes Endocrinol. 2016, 4, 470–471. [Google Scholar] [CrossRef]
- Araujo Júnior, E.; Peixoto, A.B.; Zamarian, A.C.P.; Elito Júnior, J.; Tonni, G. Macrosomia. Best Pract. Res. Clin. Obstet. Gynaecol. 2017, 38, 83–96. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.; Chai, J.; Li, J.; Shang, X.; Pei, L.; Jiang, L.; Zhang, J.; Sun, P.; Dong, W.; Wang, Y.; et al. Incidence of Macrosomia in Rural Areas—Henan Province, China, 2013–2017. China CDC Wkly 2021, 3, 788–792. [Google Scholar] [CrossRef] [PubMed]
- McDonald, S.D.; Woolcott, C.; Chapinal, N.; Guo, Y.F.; Murphy, P.; Dzakpasu, S. Interprovincial variation in pre-pregnancy body mass index and gestational weight gain and their impact on neonatal birth weight with respect to small and large for gestational age. Can. J. Public Health 2018, 109, 527–538. [Google Scholar] [CrossRef]
- Gao, Y.; Zhou, H.; Singh, N.S.; Powell-Jackson, T.; Nash, S.; Yang, M.; Guo, S.; Fang, H.; Alvarez, M.M.; Liu, X.; et al. Progress and challenges in maternal health in western China: A Countdown to 2015 national case study. Lancet Glob. Health 2017, 5, e523–e536. [Google Scholar] [CrossRef] [Green Version]
- Guo, Y.; Bai, J.; Na, H. The history of China’s maternal and child health care development. Semin. Fetal Neonatal Med. 2015, 20, 309–314. [Google Scholar] [CrossRef]
- Zhang, H.; Liu, X.; Penn-Kekana, L.; Ronsmans, C. A systematic review of the profile and density of the maternal and child health workforce in China. Hum. Resour. Health 2021, 19, 125. [Google Scholar] [CrossRef]
- van der Windt, M.; van Zundert, S.K.M.; Schoenmakers, S.; Jansen, P.W.; van Rossem, L.; Steegers-Theunissen, R.P.M. Effective psychological therapies to improve lifestyle behaviors in (pre)pregnant women: A systematic review. Prev. Med. Rep. 2021, 24, 101631. [Google Scholar] [CrossRef]
- Dean, S.V.; Lassi, Z.S.; Imam, A.M.; Bhutta, Z.A. Preconception care: Nutritional risks and interventions. Reprod. Health 2014, 11 (Suppl. 3), S3. [Google Scholar] [CrossRef] [Green Version]
- Goldstein, R.F.; Abell, S.K.; Ranasinha, S.; Misso, M.; Boyle, J.A.; Black, M.H.; Li, N.; Hu, G.; Corrado, F.; Rode, L.; et al. Association of Gestational Weight Gain with Maternal and Infant Outcomes: A Systematic Review and Meta-analysis. JAMA 2017, 317, 2207–2225. [Google Scholar] [CrossRef] [PubMed]
- Maheshwari, A.; Pandey, S.; Amalraj Raja, E.; Shetty, A.; Hamilton, M.; Bhattacharya, S. Is frozen embryo transfer better for mothers and babies? Can cumulative meta-analysis provide a definitive answer? Hum. Reprod. Update 2018, 24, 35–58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ye, W.; Luo, C.; Huang, J.; Li, C.; Liu, Z.; Liu, F. Gestational diabetes mellitus and adverse pregnancy outcomes: Systematic review and meta-analysis. BMJ 2022, 377, e067946. [Google Scholar] [CrossRef]
- He, H.; Blum, R.W. Prevalence of unintended pregnancy and its associated factors among sexually active never-married youth in Shanghai. J. Paediatr. Child. Health 2013, 49, 912–918. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | 2013 (n = 1,724,140) | 2014 (n = 1,669,015) | 2015 (n = 1,611,623) | 2016 (n = 1,753,983) | 2017 (n = 1,239,859) | p |
|---|---|---|---|---|---|---|
| Maternal Age, years | <0.001 | |||||
| 20–24 | 657,608 (38.14) | 556,039 (33.32) | 482,719 (29.95) | 382,674 (21.82) | 268,003 (21.62) | |
| 25–29 | 770,482 (44.69) | 806,810 (48.34) | 822,139 (51.01) | 797,620 (45.47) | 568,804 (45.88) | |
| 30–34 | 233,108 (13.52) | 234,462 (14.05) | 231,734 (14.38) | 361,927 (20.63) | 273,983 (22.10) | |
| ≥35 | 62,942 (3.65) | 71,704 (4.30) | 75,031 (4.66) | 211,762 (12.07) | 129,069 (10.41) | |
| Paternal Age, years | <0.001 | |||||
| 20–24 | 382,952 (22.40) | 310,199 (18.72) | 260,441 (16.28) | 191,515 (11.01) | 139,167 (11.32) | |
| 25–29 | 836,016 (48.89) | 849,644 (51.28) | 847,755 (52.98) | 776,783 (44.65) | 551,839 (44.90) | |
| 30–34 | 353,500 (20.67) | 350,423 (21.15) | 346,579 (21.66) | 448,080 (25.76) | 338,981 (27.58) | |
| ≥35 | 137,437 (8.04) | 146,568 (8.85) | 145,423 (9.09) | 323,215 (18.58) | 199,136 (16.20) | |
| Missing | 382,952 (22.40) | 310,199 (18.72) | 260,441 (16.28) | 191,515 (11.01) | 139,167 (11.32) | |
| Higher Education | <0.001 | |||||
| No | 1,095,682 (63.55) | 1,017,974 (60.99) | 897,629 (55.70) | 955,085 (54.45) | 652,205 (52.60) | |
| Yes | 582,745 (33.80) | 601,619 (36.05) | 651,372 (40.42) | 721,426 (41.13) | 522,423 (42.14) | |
| Missing | 45,713 (2.65) | 49,422 (2.96) | 62,622 (3.89) | 77,472 (4.42) | 65,231 (5.26) | |
| Nationality | <0.001 | |||||
| Han | 1,578,694 (91.56) | 1,525,842 (91.42) | 1,473,028 (91.40) | 1,607,399 (91.64) | 1,128,913 (91.05) | |
| Minority | 122,942 (7.13) | 121,164 (7.26) | 115,491 (7.17) | 123,645 (7.05) | 91,925 (7.41) | |
| Missing | 22,504 (1.31) | 22,009 (1.32) | 23,104 (1.43) | 22,939 (1.31) | 19,021 (1.53) | |
| Household Registration | <0.001 | |||||
| Rural | 1,618,453 (93.87) | 1,544,734 (92.55) | 1,451,580 (90.07) | 1,537,184 (87.64) | 1,078,553 (86.99) | |
| Urban | 105,675 (6.13) | 124,274 (7.45) | 160,013 (9.93) | 216,293 (12.33) | 160,366 (12.93) | |
| Missing | 12 (0.00) | 7 (0.00) | 30 (0.00) | 506 (0.03) | 940 (0.08) | |
| Smoking | <0.001 | |||||
| No | 1,713,054 (99.36) | 1,659,213 (99.41) | 1,602,495 (99.43) | 1,743,897 (99.42) | 1,233,200 (99.46) | |
| Yes | 4342 (0.25) | 3221 (0.19) | 3087 (0.19) | 3408 (0.19) | 2738 (0.22) | |
| Missing | 6744 (0.39) | 6581 (0.39) | 6041 (0.37) | 6678 (0.38) | 3921 (0.32) | |
| Secondhand smoking, min/day | <0.001 | |||||
| No | 1,624,386 (94.21) | 1,597,278 (95.70) | 1,551,638 (96.28) | 1,689,288 (96.31) | 1,194,750 (96.36) | |
| 1–14 | 60,250 (3.49) | 42,586 (2.55) | 34,271 (2.13) | 37,916 (2.16) | 26,129 (2.11) | |
| ≥ 15 | 32,971 (1.91) | 22,311 (1.34) | 19,573 (1.21) | 20,042 (1.14) | 15,118 (1.22) | |
| Missing | 6533 (0.38) | 6840 (0.41) | 6141 (0.38) | 6737 (0.38) | 3862 (0.31) | |
| Alcohol Consumption | <0.001 | |||||
| No | 1,666,488 (96.66) | 1,615,724 (96.81) | 1,560,839 (96.85) | 1,698,200 (96.82) | 1,201,907 (96.94) | |
| Yes | 14,748 (0.86) | 10,486 (0.63) | 10,208 (0.63) | 11,117 (0.63) | 8575 (0.69) | |
| Missing | 42,904 (2.49) | 42,805 (2.56) | 40,576 (2.52) | 44,666 (2.55) | 29,377 (2.37) | |
| Parity | <0.001 | |||||
| Nulliparous | 1,215,682 (70.51) | 1,108,008 (66.39) | 1,045,340 (64.86) | 826,378 (47.11) | 610,468 (49.24) | |
| Parous | 502,904 (29.17) | 555,377 (33.28) | 561,148 (34.82) | 922,259 (52.58) | 626,471 (50.53) | |
| Missing | 5554 (0.32) | 5630 (0.34) | 5135 (0.32) | 5346 (0.30) | 2920 (0.24) | |
| Infant sex | ||||||
| Male | 865,840 (50.22) | 832,099 (49.86) | 801,885 (49.76) | 870,408 (49.62) | 636,012 (51.30) | |
| Female | 784,004 (45.47) | 765,036 (45.84) | 742,513 (46.07) | 810,032 (46.18) | 585,914 (47.26) | |
| Missing | 74,296 (4.31) | 71,800 (4.31) | 67,222 (4.17) | 73,543 (4.19) | 17,933 (1.45) | |
| GDP per Capita, CNY | <0.001 | |||||
| < 40,000 | 344,350 (19.97) | 333,020 (19.95) | 327,431 (20.32) | 386,462 (22.03) | 318,536 (25.69) | |
| 40,000- | 319,547 (18.53) | 283,217 (16.97) | 232,499 (14.43) | 290,782 (16.58) | 231,688 (18.69) | |
| 50,000- | 720,995 (41.82) | 708,109 (42.43) | 708,664 (43.97) | 695,313 (39.64) | 381,478 (30.77) | |
| 70,000- | 339,248 (19.68) | 344,669 (20.65) | 343,029 (21.28) | 381,426 (21.75) | 308,157 (24.85) | |
| Tier of City | <0.001 | |||||
| Tier I | 35,130 (2.04) | 30,359 (1.82) | 36,677 (2.28) | 56,102 (3.20) | 49,858 (4.02) | |
| New Tier I | 98,620 (5.72) | 89,916 (5.39) | 100,667 (6.25) | 116,104 (6.62) | 96,719 (7.80) | |
| Tier II | 140,210 (8.13) | 135,160 (8.10) | 134,108 (8.32) | 147,960 (8.44) | 112,844 (9.10) | |
| Tier III | 682,936 (39.61) | 670,257 (40.16) | 648,702 (40.25) | 689,582 (39.32) | 490,974 (39.60) | |
| Tier IV | 516,935 (29.98) | 512,303 (30.69) | 473,324 (29.37) | 504,166 (28.74) | 292,385 (23.58) | |
| Tier V | 250,309 (14.52) | 231,020 (13.84) | 218,145 (13.54) | 240,069 (13.69) | 197,079 (15.90) | |
| Region | <0.001 | |||||
| Northeast | 20,090 (1.17) | 16,195 (0.97) | 15,965 (0.99) | 17,251 (0.98) | 16,320 (1.32) | |
| North | 126,775 (7.35) | 99,636 (5.97) | 99,900 (6.20) | 107,196 (6.11) | 80,621 (6.50) | |
| Northwest | 100,965 (5.86) | 97,468 (5.84) | 97,497 (6.05) | 108,909 (6.21) | 111,583 (9.00) | |
| East | 425,148 (24.66) | 405,644 (24.30) | 373,960 (23.20) | 451,801 (25.76) | 339,895 (27.41) | |
| Central | 646,124 (37.48) | 652,856 (39.12) | 647,695 (40.19) | 618,365 (35.25) | 346,283 (27.93) | |
| South | 265,665 (15.41) | 256,281 (15.36) | 241,381 (14.98) | 280,430 (15.99) | 230,803 (18.62) | |
| Southwest | 139,373 (8.08) | 140,935 (8.44) | 135,225 (8.39) | 170,031 (9.69) | 114,354 (9.22) | |
| Year | High BMI (%) | Macrosomia (%) | LGA (%) | RR (95% CI) | |
|---|---|---|---|---|---|
| Macrosomia | LGA | ||||
| Total | 849,174 (10.62) | 336,701 (4.21) | 691,656 (8.65) | 1.40 (1.39–1.41) | 1.29 (1.29–1.30) |
| 2013 | 151,362 (8.78) | 82,613 (4.79) | 160,490 (9.31) | 1.34 (1.31–1.37) | 1.25 (1.23–1.27) |
| 2014 | 153,023 (9.17) | 74,088 (4.44) | 146,860 (8.80) | 1.37 (1.34–1.40) | 1.27 (1.25–1.29) |
| 2015 | 162,678 (10.09) | 67,672 (4.20) | 135,508 (8.41) | 1.41 (1.38–1.44) | 1.30 (1.28–1.32) |
| 2016 | 222,054 (12.66) | 71,112 (4.05) | 148,576 (8.47) | 1.46 (1.43–1.49) | 1.32 (1.31–1.34) |
| 2017 | 160,057 (12.91) | 41,216 (3.32) | 100,222 (8.08) | 1.54 (1.50–1.58) | 1.37 (1.35–1.39) |
| p trend | <0.05 | <0.01 | <0.05 | <0.01 | <0.01 |
| APC, % | 11.56 (5.36–18.13) | −7.89 [−12.40–(−3.15)] | −3.15 [−5.01–(−1.26)] | 3.51 (2.39–4.64) | 2.29 (1.74–2.84) |
| Year | Macrosomia | LGA | ||
|---|---|---|---|---|
| Crude PAF, % | Adjusted PAF, % | Crude PAF, % | Adjusted PAF, % | |
| Total | 4.76 (4.63–4.89) | 4.44 (4.33–4.54) | 3.87 (3.79–3.96) | 3.33 (3.26–3.40) |
| 2013 | 3.54 (3.31–3.77) | 3.16 (2.97–3.35) | 2.82 (2.66–2.98) | 2.35 (2.21–2.48) |
| 2014 | 4.10 (3.85–4.36) | 3.64 (3.43–3.84) | 3.31 (3.14–3.49) | 2.70 (2.55–2.84) |
| 2015 | 4.55 (4.27–4.83) | 4.32 (4.09–4.53) | 3.65 (3.46–3.84) | 3.20 (3.04–3.36) |
| 2016 | 6.41 (6.10–6.73) | 5.99 (5.74–6.23) | 5.00 (4.79–5.20) | 4.33 (4.15–4.50) |
| 2017 | 7.40 (6.98–7.83) | 7.11 (6.79–7.42) | 5.59 (5.34–5.85) | 5.00 (4.79–5.21) |
| p trend | < 0.01 | < 0.01 | < 0.01 | < 0.01 |
| APC, % | 21.19 (13.26–29.68) | 23.60 (16.76–30.85) | 19.49 (12.72–26.65) | 21.98 (16.14–28.11) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zeng, S.; Yang, Y.; Han, C.; Mu, R.; Deng, Y.; Lv, X.; Xie, W.; Huang, J.; Wu, S.; Zhang, Y.; et al. Burden and Trend of Macrosomia and Large-for-Gestational-Age Neonates Attributable to High Pre-Pregnancy Body Mass Index in China, 2013–2017: A Population-Based Retrospective Cohort Study. Healthcare 2023, 11, 331. https://doi.org/10.3390/healthcare11030331
Zeng S, Yang Y, Han C, Mu R, Deng Y, Lv X, Xie W, Huang J, Wu S, Zhang Y, et al. Burden and Trend of Macrosomia and Large-for-Gestational-Age Neonates Attributable to High Pre-Pregnancy Body Mass Index in China, 2013–2017: A Population-Based Retrospective Cohort Study. Healthcare. 2023; 11(3):331. https://doi.org/10.3390/healthcare11030331
Chicago/Turabian StyleZeng, Shuai, Ying Yang, Chunying Han, Rongwei Mu, Yuzhi Deng, Xinyi Lv, Wenlu Xie, Jiaxin Huang, Siyu Wu, Ya Zhang, and et al. 2023. "Burden and Trend of Macrosomia and Large-for-Gestational-Age Neonates Attributable to High Pre-Pregnancy Body Mass Index in China, 2013–2017: A Population-Based Retrospective Cohort Study" Healthcare 11, no. 3: 331. https://doi.org/10.3390/healthcare11030331




