Preparing Cities for Future Pandemics: Unraveling the Influence of Urban and Housing Variables on COVID-19 Incidence in Santiago de Chile
Abstract
:1. Introduction
Motivation
2. Literature Review
2.1. Socioeconomic Status, Lifestyle, and Education
2.2. Urban Planning
2.3. Housing
2.4. Antecedents: Chile and COVID-19
3. Materials and Methods
3.1. Materials
3.2. Variable Selection Using GLS-Based Linear Regression
- (i)
- Initially, an approximation of the parameter is made from the OLS estimator of the term by raising each observation to the second power. So, ;
- (ii)
- The inverse of the square root of the estimator obtained in (i) is multiplied by each observed variable of the regression model, so as to re-estimate the model transformed by the OLS method.
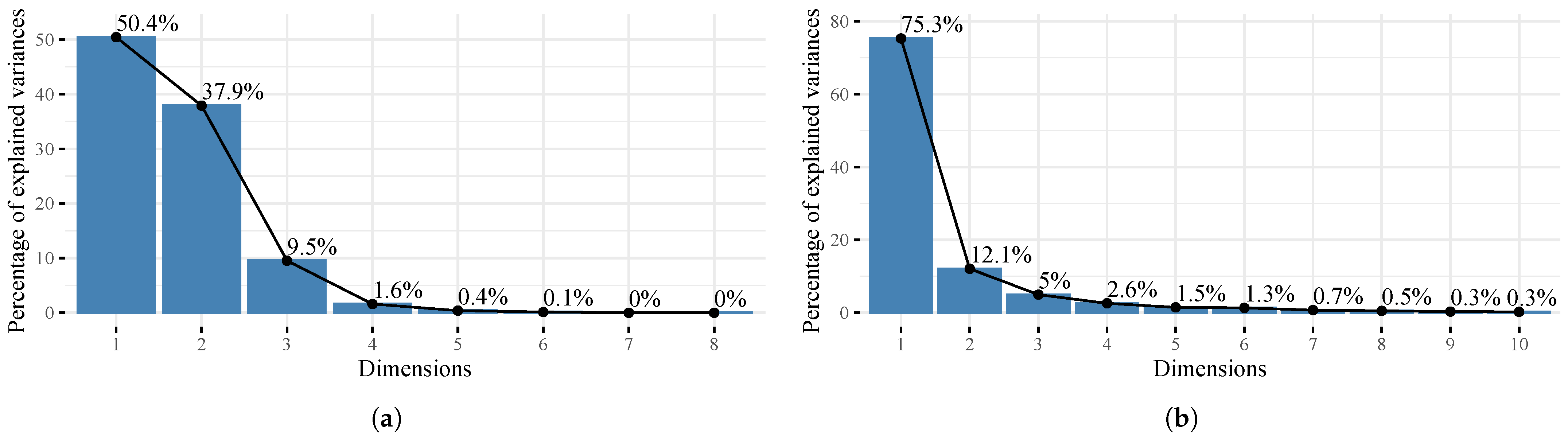
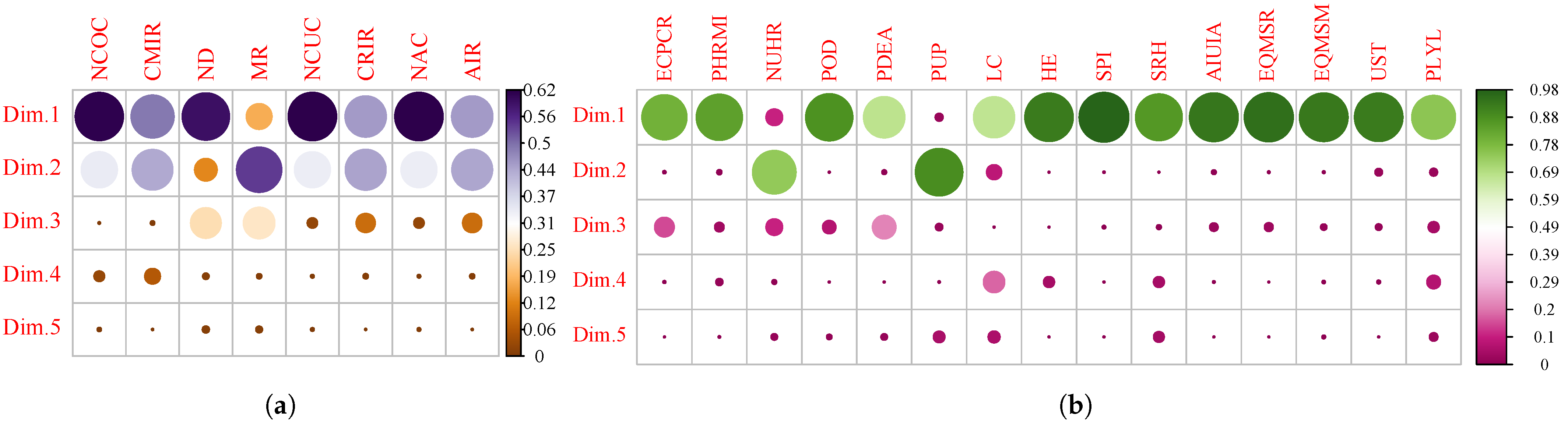
3.3. Principal Component Analysis
3.4. Implementation of the Methods
- 1.
- Selection of variables using linear regression based on GLS:
- (a)
- A correlation coefficient greater than 60% ( adjusted > 0.60) is considered;
- (b)
- They are classified as exogenous variables if they are not statistically correlated with the residuals and do not present bias and endogeneity. Then:
- i.
- Two groups are obtained that are divided into those with correlation 0, and those whose correlation is significant;
- ii.
- Regressions correlated with the residual are discarded or, if necessary, corrected using GLS.
- (c)
- White’s heteroscedasticity test is applied to all variables to verify the contribution of each of the variables to variance, using the hypothesis test:
- i.
- there is no heteroscedasticity;
- ii.
- there is heteroscedasticity, because the variance is not constant.
- (d)
- The Bayesian information criterion (BIC) is used to select the best model (lowest BIC) from a finite set of possible M models, which can define the cause and effect variables applicable to the pandemic period.
- 2.
- Using PCA, a multivariate analysis was performed on the COVID-19 dataset. In addition, the dependence of the influential variables was studied, the correlations were identified, and clusters were determined by k-means (For the PCA and k-means, the library factoextra [27], implemented in the R software (R version 4.2.3, https://www.r-project.org/ (accessed on 30 March 2023)), was considered).
- 3.
4. Results
- 1.
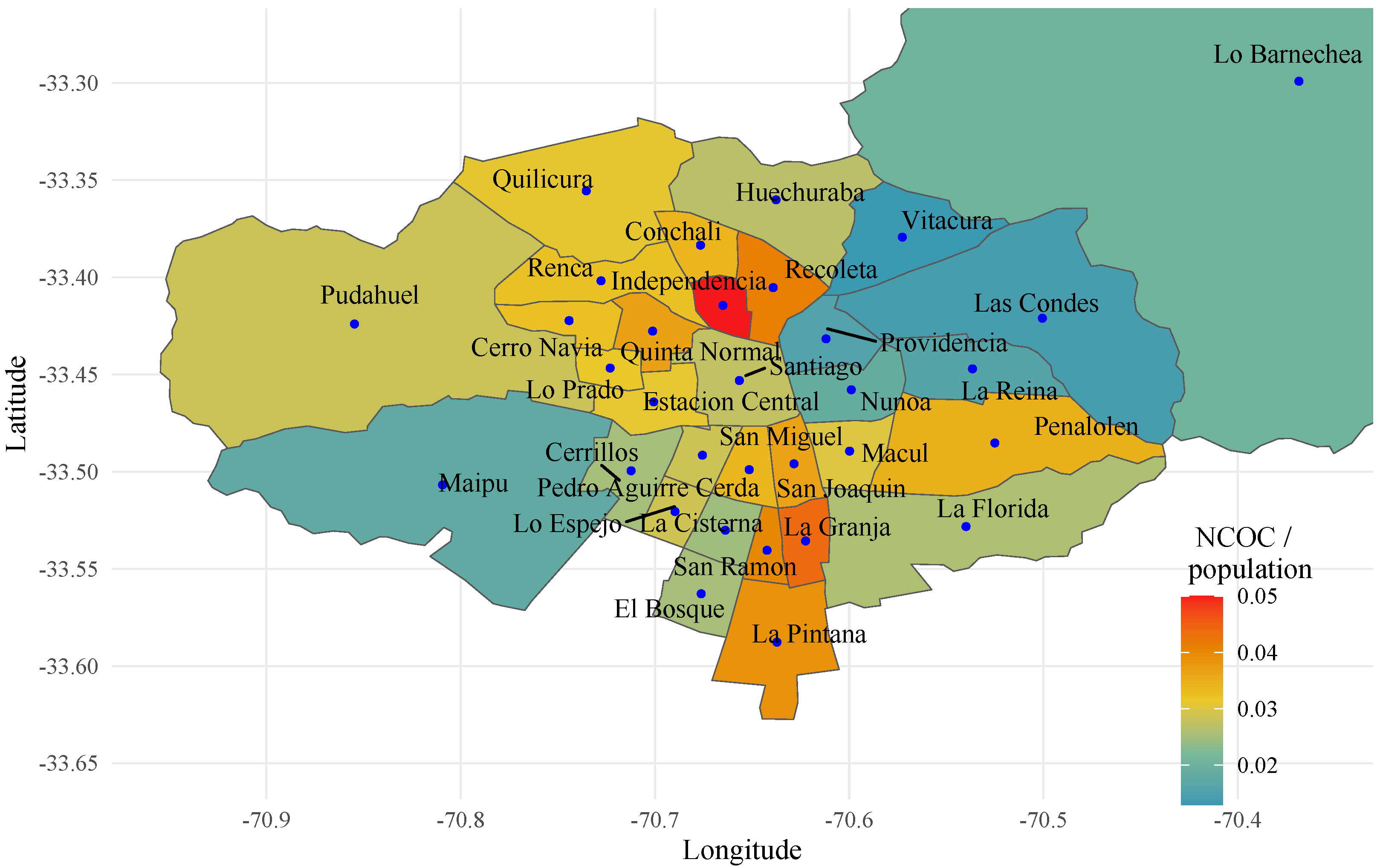
- Dependent variables: Number of Confirmed Cases (NCOC), Cumulative Incidence Rate (CMIR), Number of Deceased (ND), Mortality Rate (MR), Number of Current Cases (NCUC), Current Incidence Rate (CRIR), Number of Active Cases (NAC), Asset Incidence Rate (AIR).
- 2.
- Independent variables: Electricity Consumption Per Capita Residential (ECPCR), Private Homes that Require Materiality Improvements (PHRMI), New Urban Housing Requirement (NUHR), Percentage of Overcrowded Dwellings (POD), Percentage of Dwellings with External Allegiance (PDEA), Park User Population (PUP), Number of households that live in the same house, with an independent budget (HSH), Labor Conditions (LC), Housing and Environment (HE), Social Priority Index (SPI), Social Register of Households (SRH), Average Income of Unemployment Insurance Affiliates (AIUIA), System for Measuring the Quality of Education, Reading (EQMSR), Education Quality Measurement System, Mathematics (EQMSM), University Selection Test (UST), Potential Life Years Lost (PLYL).
- Cluster 1: corresponds to the southeast, southwest, northwest, south, and central sectors which have a medium–low level of socioeconomic development and include the following communes: Macul, La Florida, Maipu, Cerrillos, Santiago, Huechuraba, Pudahuel, Quilicura, San Miguel, and La Cisterna.
- Cluster 2: incorporates the northwest, north, and south sectors that include the communes with the lowest level of socioeconomic development such as Cerro Navia, Lo Prado, Conchali, Independencia, Recoleta, El Bosque, Pedro Aguirre Cerda, San Joaquín, Lo Espejo, La Granja, San Ramon, La Pintana, Quinta Normal, and Renca.
- Cluster 3: located in the northeast, it contains the communes of greater socioeconomic development such as La Reina, Las Condes, Lo Barnechea, Ñuñoa, Providencia, and Vitacura.
- In the case of the communes of Cerrillos, Estacion Central, and Peñalolen, they are grouped into different clusters depending on the COVID-19 dimension (see Table 1).
5. Discussion
6. Conclusions
6.1. Implications for the Preparedness for Future Pandemics
6.2. Future Research Questions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AIR | Asset Incidence Rate |
| AIUIA | Average Income of Unemployment Insurance Affiliates |
| CMIR | Cumulative Incidence Rate |
| CRIR | Current Incidence Rate |
| ECPCR | Electricity Consumption Per Capita Residential |
| EQMSM | Education Quality Measurement System, Mathematics |
| EQMSR | System for Measuring the Quality of Education, Reading |
| GDP | Gross Domestic Product |
| GLS | Generalized Least Squares |
| HE | Housing and Environment |
| HSH | Number of households that live in the same house, with an independent budget |
| LC | Labor Conditions |
| LMIC | Low and Middle Income Countries |
| MR | Mortality Rate |
| NAC | Number of Active Cases |
| NCOC | Number of Confirmed Cases |
| NCUC | Number of Current Cases |
| ND | Number of Deceased |
| NUHR | New Urban Housing Requirement |
| OLS | Ordinary Least Squares |
| PCA | Principal Component Analysis |
| PDEA | Percentage of Dwellings with External Allegiance |
| PHRMI | Private Homes that Require Materiality Improvements |
| PLYL | Potential Life Years Lost |
| POD | Percentage of Overcrowded Dwellings |
| PUP | Park User Population |
| SES | Socioeconomic Status |
| SPI | Social Priority Index |
| SRH | Social Register of Households |
| UST | University Selection Test |
References
- Idrovo-Aguirre, B.J.; Contreras-Reyes, J.E. Monetary fiscal contributions to households and pension fund withdrawals during the COVID-19 pandemic: An approximation of their impact on construction labor supply in Chile. Soc. Sci. 2021, 10, 417. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, A.; Wang, J. Exploring the roles of high-speed train, air and coach services in the spread of COVID-19 in China. Transp. Policy 2020, 94, 34–42. [Google Scholar] [CrossRef]
- Coelho, M.T.P.; Rodrigues, J.F.M.; Medina, A.M.; Scalco, P.; Terribile, L.C.; Vilela, B.; Diniz-Filho, J.A.F.; Dobrovolski, R. Global expansion of COVID-19 pandemic is driven by population size and airport connections. PeerJ 2020, 8, e9708. [Google Scholar] [CrossRef]
- Sokadjo, Y.M.; Atchadé, M.N. The influence of passenger air traffic on the spread of COVID-19 in the world. Transp. Res. Interdiscip. Perspect. 2020, 8, 100213. [Google Scholar] [CrossRef] [PubMed]
- Hamidi, S.; Sabouri, S.; Ewing, R. Does Density Aggravate the COVID-19 Pandemic?: Early Findings and Lessons for Planners. J. Am. Plan. Assoc. 2020, 86, 495–509. [Google Scholar] [CrossRef]
- Pereira, R.J.; do Nascimento, G.N.L.; Gratão, L.H.A.; Pimenta, R.S. The risk of COVID-19 transmission in favelas and slums in Brazil. Public Health 2020, 183, 42. [Google Scholar] [CrossRef]
- Bottan, N.; Hoffmann, B.; Vera-Cossio, D. The unequal impact of the coronavirus pandemic: Evidence from seventeen developing countries. PLoS ONE 2020, 15, e0239797. [Google Scholar] [CrossRef]
- Power, E.R.; Rogers, D.; Kadi, J. Public housing and COVID-19: Contestation, challenge and change. Int. J. Hous. Policy 2020, 20, 313–319. [Google Scholar] [CrossRef]
- Gurney, C.M. Dangerous liaisons? Applying the social harm perspective to the social inequality, housing and health trifecta during the Covid-19 pandemic. Int. J. Hous. Policy 2021, 23, 232–259. [Google Scholar] [CrossRef]
- Béland, D.; He, A.J.; Ramesh, M. COVID-19, crisis responses, and public policies: From the persistence of inequalities to the importance of policy design. Policy Soc. 2022, 41, 187–198. [Google Scholar] [CrossRef]
- Blundell, R.; Costa Dias, M.; Joyce, R.; Xu, X. COVID-19 and Inequalities. Fisc. Stud. 2020, 41, 291–319. [Google Scholar] [CrossRef]
- Idrovo-Aguirre, B.J.; Lozano, F.J.; Contreras-Reyes, J.E. Prosperity or Real Estate Bubble? Exuberance probability index of the Real Price of Housing in Chile. Int. J. Financ. Stud. 2021, 9, 51. [Google Scholar] [CrossRef]
- Núñez, A.; Sreeganga, S.D.; Ramaprasad, A. Access to Healthcare during COVID-19. Int. J. Environ. Res. Public Health 2021, 18, 2980. [Google Scholar] [CrossRef] [PubMed]
- Horne, R.; Willand, N.; Dorignon, L.; Middha, B. Housing inequalities and resilience: The lived experience of COVID-19. Int. J. Hous. Policy 2021, 23, 313–337. [Google Scholar] [CrossRef]
- Quapper, D.D. Excess deaths due to the COVID-19 pandemic in Chile. Rev. Med. Chil. 2021, 149, 1525–1531. [Google Scholar] [CrossRef] [PubMed]
- Bavel, J.J.V.; Baicker, K.; Boggio, P.S.; Capraro, V.; Cichocka, A.; Cikara, M.; Crockett, M.J.; Crum, A.J.; Douglas, K.M.; Druckman, J.N.; et al. Using social and behavioural science to support COVID-19 pandemic response. Nat. Hum. Behav. 2020, 4, 460–471. [Google Scholar] [CrossRef]
- Aragona, M.; Barbato, A.; Cavani, A.; Costanzo, G.; Mirisola, C. Negative impacts of COVID-19 lockdown on mental health service access and follow-up adherence for immigrants and individuals in socio-economic difficulties. Public Health 2020, 186, 52–56. [Google Scholar] [CrossRef] [PubMed]
- Chávez, D.; Contreras-Reyes, J.E.; Idrovo-Aguirre, B.J. A Threshold GARCH Model for Chilean Economic Uncertainty. J. Risk Financ. Manag. 2023, 16, 20. [Google Scholar] [CrossRef]
- Poppe, A. Impact of the Healthcare System, Macro Indicator, General Mandatory Quarantine, and Mask Obligation on COVID-19 Cases and Death in Six Latin American Countries: An Interrupted Time Series Study. Front. Public Health 2020, 8, 607832. [Google Scholar] [CrossRef]
- Micah, A.E.; Cogswell, I.E.; Cunningham, B.; Ezoe, S.; Harle, A.C.; Maddison, E.R.; McCracken, D.; Nomura, S.; Simpson, K.E.; Stutzman, H.N.; et al. Tracking development assistance for health and for COVID-19: A review of development assistance, government, out-of-pocket, and other private spending on health for 204 countries and territories, 1990–2050. Lancet 2021, 398, 1317–1343. [Google Scholar] [CrossRef]
- Mendoza, J. Government’s Health Expenditure in Chile 2020; Statista: Hamburg, Germany, 2021; p. 1104665. [Google Scholar]
- Oshinubi, K.; Rachdi, M.; Demongeot, J. Modeling of COVID-19 Pandemic vis-à-vis Some Socio-Economic Factors. Front. Appl. Math. Stat. 2022, 7, 1–25. [Google Scholar] [CrossRef]
- Comunian, S.; Dongo, D.; Milani, C.; Palestini, P. Air Pollution and COVID-19: The Role of Particulate Matter in the Spread and Increase of COVID-19’s Morbidity and Mortality. Int. J. Environ. Res. Public Health 2020, 17, 4487. [Google Scholar] [CrossRef]
- Demongeot, J.; Oshinubi, K.; Rachdi, M.; Seligmann, H. Geoclimatic, demographic and socio-economic determinants of the Covid-19 prevalence. EGU Gen. Assem. 2021, 2021, 7976. [Google Scholar] [CrossRef]
- University of Geneva; E T H Zürich-EPFL. COVID-19 Daily Epidemic Forecasting; University of Geneva: Geneva, Switzerland, 2022. [Google Scholar]
- Mena, G.E.; Martinez, P.P.; Mahmud, A.S.; Marquet, P.A.; Buckee, C.O.; Santillana, M. Socioeconomic status determines COVID-19 incidence and related mortality in Santiago, Chile. Science 2021, 372, eabg5298. [Google Scholar] [CrossRef] [PubMed]
- Kassambara, A.; Mundt, F. Package ‘factoextra’: Extract and Visualize the Results of Multivariate Data Analyses, Version 1.0.7; R Foundation: Vienna, Austria, 2020. [Google Scholar]
- Ahmed, J.; Jaman, M.H.; Saha, G.; Ghosh, P. Effect of environmental and socio-economic factors on the spreading of COVID-19 at 70 cities/provinces. Heliyon 2021, 7, e06979. [Google Scholar] [CrossRef]
- Baser, O. Population density index and its use for distribution of Covid-19: A case study using Turkish data. Health Policy 2021, 125, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Cifuentes-Faura, J. COVID-19 Mortality Rate and Its Incidence in Latin America: Dependence on Demographic and Economic Variables. Int. J. Environ. Res. Public Health 2021, 18, 6900. [Google Scholar] [CrossRef] [PubMed]
- Canatay, A.; Emegwa, T.J.; Hossain Talukder, M.F. Critical country-level determinants of death rate during Covid-19 pandemic. Int. J. Disaster Risk Reduct. 2021, 64, 102507. [Google Scholar] [CrossRef]
- Sharma, A.K.; Gupta, R.; Baig, V.N.; Singh, V.T.; Chakraborty, S.; Sunda, J.P.; Dhakar, P.; Sharma, S.P.; Panwar, R.B.; Katoch, V.M. Educational status and COVID-19 related outcomes in India: Hospital-based cross-sectional study. BMJ Open 2022, 12, e055403. [Google Scholar] [CrossRef]
- Sharifi, A.; Khavarian-Garmsir, A.R. The COVID-19 pandemic: Impacts on cities and major lessons for urban planning, design, and management. Sci. Total Environ. 2020, 749, 142391. [Google Scholar] [CrossRef]
- Paul, A.; Englert, P.; Varga, M. Socio-economic disparities and COVID-19 in the USA. J. Phys. Complex. 2021, 2, 35017. [Google Scholar] [CrossRef]
- Bhadra, A.; Mukherjee, A.; Sarkar, K. Impact of population density on Covid-19 infected and mortality rate in India. Model. Earth Syst. Environ. 2021, 7, 623–629. [Google Scholar] [CrossRef]
- Rogers, D.; Power, E. Housing policy and the COVID-19 pandemic: The importance of housing research during this health emergency. Int. J. Hous. Policy 2020, 20, 177–183. [Google Scholar] [CrossRef]
- Hu, M.; Roberts, J.D.; Azevedo, G.P.; Milner, D. The role of built and social environmental factors in Covid-19 transmission: A look at America’s capital city. Sustain. Cities Soc. 2021, 65, 102580. [Google Scholar] [CrossRef]
- Molina-Betancur, J.C.; Martínez-Herrera, E.; Pericàs, J.M.; Benach, J. Coronavirus disease 2019 and slums in the Global South: Lessons from Medellín (Colombia). Glob. Health Promot. 2020, 28, 65–69. [Google Scholar] [CrossRef]
- Gordon, S.B.; Bruce, N.G.; Grigg, J.; Hibberd, P.L.; Kurmi, O.P.; Lam, K.b.H.; Mortimer, K.; Asante, K.P.; Balakrishnan, K.; Balmes, J.; et al. Respiratory risks from household air pollution in low and middle income countries. Lancet Respir. Med. 2014, 2, 823–860. [Google Scholar] [CrossRef] [Green Version]
- Neves Souza, F.; Awoniyi, A.M.; Palma, F.A.G.; Begon, M.; Costa, F. Increased Rat Sightings in Urban Slums During the COVID-19 Pandemic and the Risk for Rat-Borne Zoonoses. Vector Borne Zoonotic Dis. 2020, 21, 1–2. [Google Scholar] [CrossRef]
- Leal Filho, W.; Lütz, J.M.; Sattler, D.N.; Nunn, P.D. Coronavirus: COVID-19 Transmission in Pacific Small Island Developing States. Int. J. Environ. Res. Public Health 2020, 17, 5409. [Google Scholar] [CrossRef] [PubMed]
- Buja, A.; Paganini, M.; Cocchio, S.; Scioni, M.; Rebba, V.; Baldo, V. Demographic and socio-economic factors, and healthcare resource indicators associated with the rapid spread of COVID-19 in Northern Italy: An ecological study. PLoS ONE 2021, 15, e0244535. [Google Scholar] [CrossRef]
- Gargiulo, C.; Gaglione, F.; Guida, C.; Papa, R.; Zucaro, F.; Carpentieri, G. The role of the urban settlement system in the spread of Covid-19 pandemic. The Italian case. TeMA-J. Land Use Mobil. Environ. 2020, 2020, 189–212. [Google Scholar] [CrossRef]
- Mathieu, E.; Ritchie, H.; Ortiz-Ospina, E.; Roser, M.; Hasell, J.; Appel, C.; Giattino, C.; Rodés-Guirao, L. A global database of COVID-19 vaccinations. Nat. Hum. Behav. 2021, 5, 947–953. [Google Scholar] [CrossRef]
- Ministerio de Salud, Gobierno de Chile. #Seguimos Cuidándonos: Conozca Toda la Información del Plan Nacional de Vacunación de Nuestro país, Con Los Vacunatorios Disponibles y la Calendarización Semanal de Vacuna; Technical report; Gobierno de Chile: Santiago, Chile, 2022. [Google Scholar]
- Gil, M.; Undurraga, E.A. COVID-19 Has Exposed How ‘The Other Half’ (Still) Lives. Bull. Lat. Am. Res. 2020, 39, 28–34. [Google Scholar] [CrossRef]
- Rocha, R.; Atun, R.; Massuda, A.; Rache, B.; Spinola, P.; Nunes, L.; Lago, M.; Castro, M.C. Effect of socioeconomic inequalities and vulnerabilities on health-system preparedness and response to COVID-19 in Brazil: A comprehensive analysis. Lancet Glob. Health 2021, 9, e782–e792. [Google Scholar] [CrossRef]
- Upadhyayula, S.M.; Mutheneni, S.R.; Kadiri, M.R.; Kumaraswamy, S.; Nagalla, B. A Cohort Study of Lymphatic Filariasis on Socio Economic Conditions in Andhra Pradesh, India. PLoS ONE 2012, 7, e33779. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kutner, M.H.; Nachtsheim, C.J.; Neter, J.; Li, W. Applied Linear Statistical Models, 5th ed.; Operations and Decision Sciences; McGraw-Hill/Irwin: New York, NY, USA, 2005; p. 1396. [Google Scholar]
- Ringnér, M. What is principal component analysis? Nat. Biotechnol. 2008, 26, 303–304. [Google Scholar] [CrossRef]
- Bennett, M. All things equal? Heterogeneity in policy effectiveness against COVID-19 spread in chile. World Dev. 2021, 137, 105208. [Google Scholar] [CrossRef] [PubMed]
- Gozzi, N.; Tizzoni, M.; Chinazzi, M.; Ferres, L.; Vespignani, A.; Perra, N. Estimating the effect of social inequalities on the mitigation of COVID-19 across communities in Santiago de Chile. Nat. Commun. 2021, 12, 2429. [Google Scholar] [CrossRef]
- Manjón, J.V.; Coupé, P.; Concha, L.; Buades, A.; Collins, D.L.; Robles, M. Diffusion Weighted Image Denoising Using Overcomplete Local PCA. PLoS ONE 2013, 8, e73021. [Google Scholar] [CrossRef] [Green Version]
- Lai, S.; Zhou, Y.; Yuan, Y. Associations between Community Cohesion and Subjective Wellbeing of the Elderly in Guangzhou, China—A Cross-Sectional Study Based on the Structural Equation Model. Int. J. Environ. Res. Public Health 2021, 18, 953. [Google Scholar] [CrossRef]
- Kakebeeke, T.H.; Chaouch, A.; Caflisch, J.; Knaier, E.; Rousson, V.; Jenni, O.G. Impact of body mass index and socio-economic status on motor development in children and adolescents. Eur. J. Pediatr. 2021, 180, 1777–1787. [Google Scholar] [CrossRef] [PubMed]
- Velásquez-Burgos, R. Citizenship education policies and immigration in Chile. A dispositive analysis. Policy Futur. Educ. 2022, 20, 893–906. [Google Scholar] [CrossRef]
- Feddersen Martínez, M. La persistencia del paradigma de seguridad en la regulación de los impedimentos de ingreso en la legislación migratoria chilena. Oñati Socio-Legal Series 2022, 12, 287–327. [Google Scholar] [CrossRef]
- INE. Estadísticas: Demografía y Vitales: Proyecciones de Población. 2021. Available online: https://www.ine.cl/estadisticas/sociales/demografia-y-vitales/proyecciones-de-poblacion (accessed on 30 June 2021).
- Jara-Labarthé, V.; Cisneros Puebla, C.A. Migrants in Chile: Social crisis and the pandemic (or sailing over troubled water…). Qual. Soc. Work 2021, 20, 284–288. [Google Scholar] [CrossRef] [PubMed]
- Peñafiel, E. Estadísticas: Demografía y vitales: Demografía: Población extranjera residente en Chile llegó a 1.482.390 personas en 2021, un 1.5% más que en 2020. 2022. Available online: https://www.ine.gob.cl/estadisticas/sociales/demografia-y-vitales/demografia-y-migracion/2022/10/12/población-extranjera-residente-en-chile-llegó-a-1.482.390-personas-en-2021-un-1-5-más-que-en-2020#:~:text=Deltotaldepersonasextranjeras,del50%25dela (accessed on 8 May 2023).
- Slater, S.J.; Christiana, R.W.; Gustat, J. Recommendations for Keeping Parks and Green Space Accessible for Mental and Physical Health During COVID-19 and Other Pandemics. Prev. Chronic Dis. 2020, 17, E59. [Google Scholar] [CrossRef] [PubMed]
- Rainisch, G.; Undurraga, E.; Chowell, G. A dynamic modeling tool for estimating healthcare demand from the COVID19 epidemic and evaluating population-wide interventions. Int. J. Infect. Dis. 2020, 96, 376–383. [Google Scholar] [CrossRef] [PubMed]
- Torero Cullen, M. COVID-19 and the Risk to Food Supply Chains: How to Respond; Number March; FAO: Rome, Italy, 2020; p. 7. [Google Scholar] [CrossRef]
- OECD. Supporting People and Companies to Deal with the COVID-19 Virus: Options for an Immediate Employment and Social-Policy Response; OECD Publishing: Paris, France, 2020; p. 15. [Google Scholar]
- Ćirić, J.; Ćirić, A. The Impact of the COVID-19 Pandemic on Digital Library Usage: A Public Library Case Study. J. Web Librariansh. 2021, 15, 53–68. [Google Scholar] [CrossRef]
- Comisión Económica para América Latina y el Caribe (CEPAL). Sectores y Empresas Frente al COVID-19: Emergencia y Reactivación; Number 4 in Informe Especial COVID-19; Naciones Unidas: Santiago, Chile, 2020; p. 24. [Google Scholar]
- Aguilera, B.; Cabrera, T.; Duarte, J.; García, N.; Hernández, A.; Pérez, J.; Sasmay, A.; Signorini, V.; Talbot-Wright, H. COVID-19: Evolución, Efectos y Políticas Adoptadas en Chile y el Mundo; Number 28 in Estudios de Finanzas Públicas; Dirección de Presupuestos del Ministerio de Hacienda: Santiago, Chile, 2022; p. 71. [Google Scholar]
- Comisión Económica para América Latina y el Caribe (CEPAL). La Paradoja de la Recuperación en América Latina y el Caribe: Crecimiento con Persistentes Problemas Estructurales: Desigualdad, Pobreza, Poca Inversión y Baja Productividad; Number 11 in Informe Especial COVID-19; Naciones Unidas: Santiago, Chile, 2021; p. 42. [Google Scholar]
- Regional Office for the Americas of the World Health Organization. Lista de Verificación para Gestionar los Riesgos y los Efectos de COVID-19; Organización Panamericana de la Salud: Washington, DC, USA, 2020; p. 19. [Google Scholar]
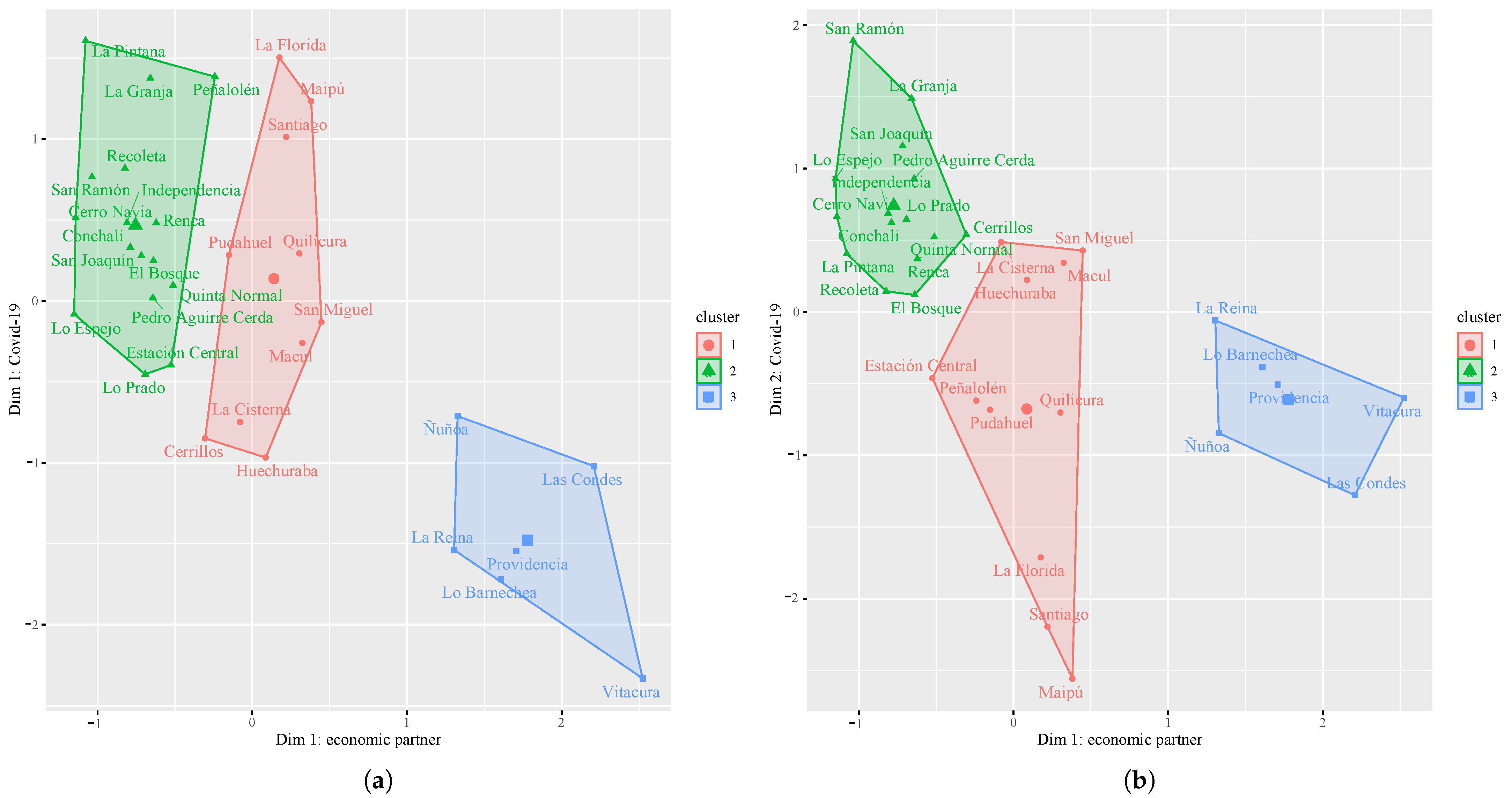
| Commune | Dim 1: COVID-19; Cluster | Dim 2: COVID-19; Cluster |
|---|---|---|
| Cerrillos | 1 | 2 |
| Estación Central | 2 | 1 |
| Peñalolen | 2 | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuschel, K.; Carrasco, R.; Idrovo-Aguirre, B.J.; Duran, C.; Contreras-Reyes, J.E. Preparing Cities for Future Pandemics: Unraveling the Influence of Urban and Housing Variables on COVID-19 Incidence in Santiago de Chile. Healthcare 2023, 11, 2259. https://doi.org/10.3390/healthcare11162259
Kuschel K, Carrasco R, Idrovo-Aguirre BJ, Duran C, Contreras-Reyes JE. Preparing Cities for Future Pandemics: Unraveling the Influence of Urban and Housing Variables on COVID-19 Incidence in Santiago de Chile. Healthcare. 2023; 11(16):2259. https://doi.org/10.3390/healthcare11162259
Chicago/Turabian StyleKuschel, Katherina, Raúl Carrasco, Byron J. Idrovo-Aguirre, Claudia Duran, and Javier E. Contreras-Reyes. 2023. "Preparing Cities for Future Pandemics: Unraveling the Influence of Urban and Housing Variables on COVID-19 Incidence in Santiago de Chile" Healthcare 11, no. 16: 2259. https://doi.org/10.3390/healthcare11162259








