Effects of the Government Response and Community Mobility on the COVID-19 Pandemic in Southeast Asia
Abstract
:1. Introduction
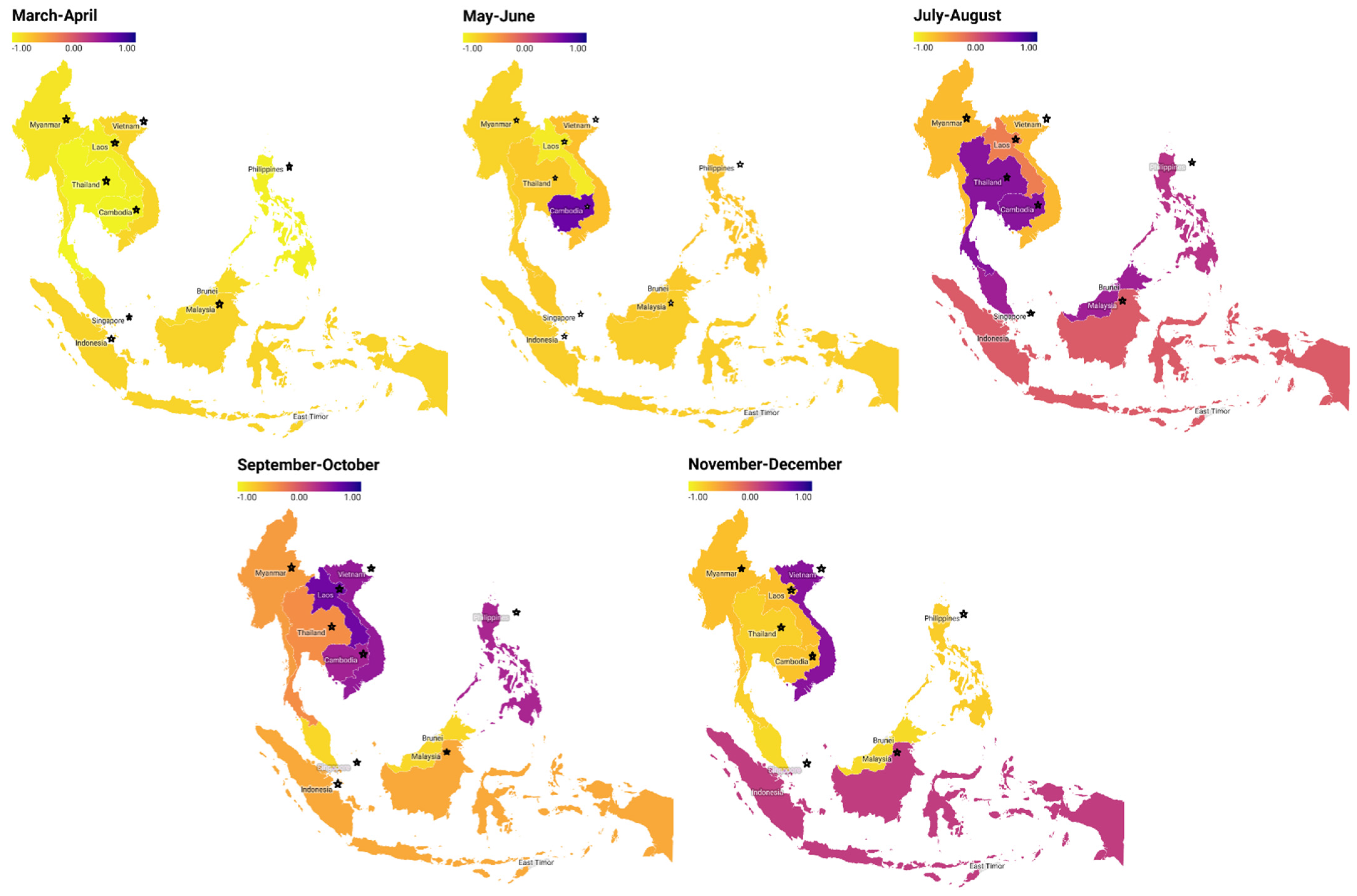
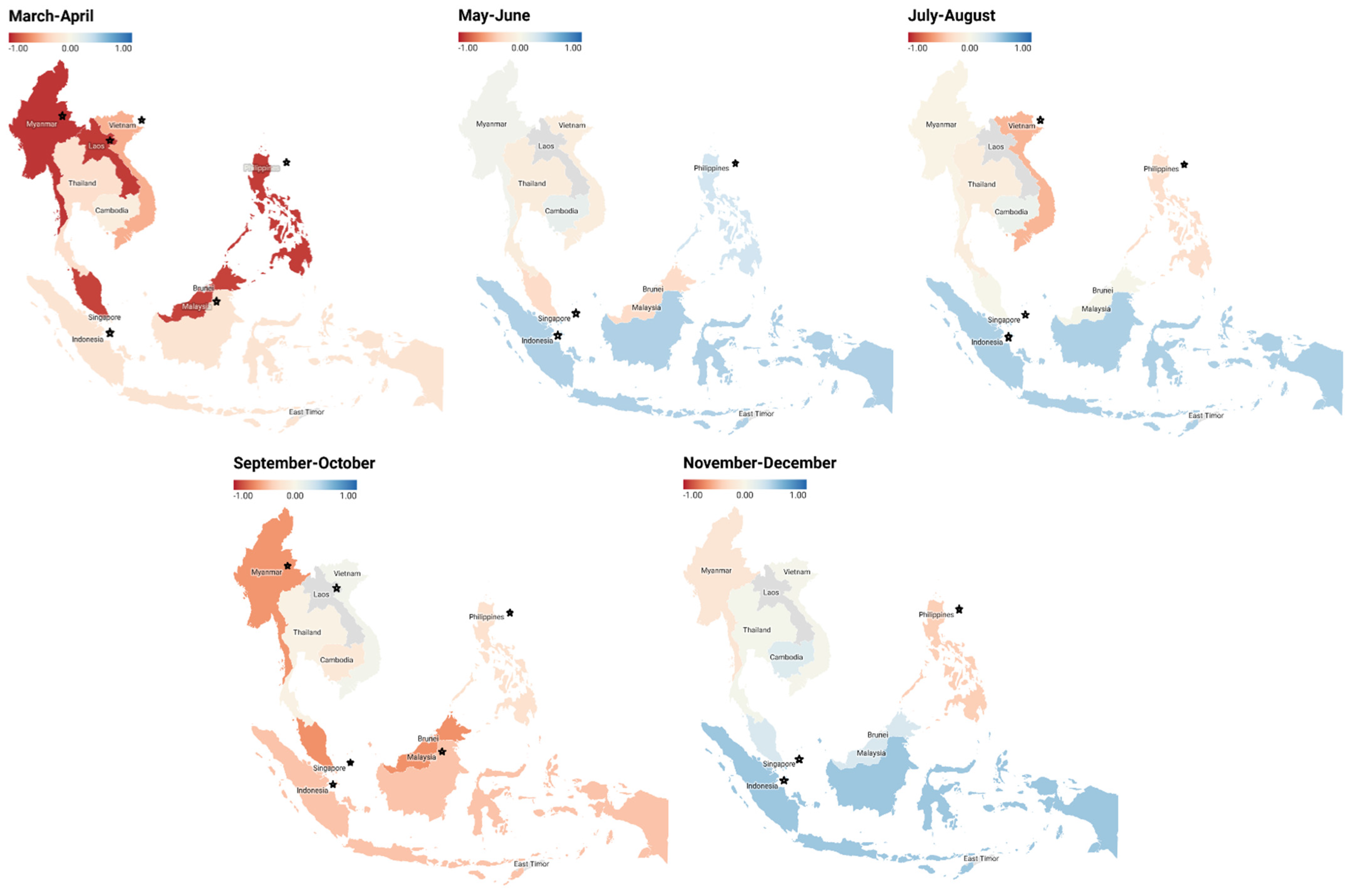
2. Materials and Methods
2.1. Data Sources and Study Framework
2.2. Variables
2.3. Data Analysis
2.4. Implementation of PLS-SEM
- indicator loadings ≥0.70;
- internal consistency reliability using Cronbach’s alpha and rho_A between 0.70 and 0.95, and composite reliability ≥0.70;
- convergent validity average variance extracted (AVE) ≥0.50;
- discriminant validity using Heterotrait-Monotrait (HTMT) ratio of correlations <0.90, cross loading, and Fornell–Larcker criterion;
- variance inflation factor (VIF) <5.
3. Results
4. Discussion
5. Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO WHO Timeline—COVID-19. Available online: https://www.who.int/news-room/detail/08-04-2020-who-timeline---covid-19 (accessed on 15 May 2020).
- Worldometer COVID-19 Coronavirus Pandemic. Available online: https://www.worldometers.info/coronavirus/ (accessed on 20 December 2020).
- Rampal, L.; Seng, L.B.; Choolani, M.; Ganasegeran, K.; Pramanick, A.; Vallibhakara, S.A.O.; Tejativaddhana, P.; Wai, H.V.C. Battling Covid-19 Pandemic Waves in Six South-East Asian Countries: A Real-Time Consensus Review. Med. J. Malays. 2020, 75, 613–625. [Google Scholar]
- World Health Organization. Infection Prevention and Control of Epidemic-and Pandemic Prone Acute Respiratory Infections in Health Care; WHO: Geneva, Switzerland, 2014. [Google Scholar]
- Abubakar, A.; Malik, M.; Pebody, R.G.; Elkholy, A.A.; Khan, W.; Bellos, A.; Mala, P. Burden of Acute Respiratory Disease of Epidemic and Pandemic Potential in the Who Eastern Mediterranean Region: A Literature Review. East. Mediterr. Health J. 2016, 22, 513–526. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization Disease Outbreaks. Available online: https://www.who.int/emergencies/diseases/en/ (accessed on 20 December 2020).
- De Wit, E.; Van Doremalen, N.; Falzarano, D.; Munster, V.J. SARS and MERS: Recent Insights into Emerging Coronaviruses. Nat. Rev. Microbiol. 2016, 14, 523–534. [Google Scholar] [CrossRef] [PubMed]
- Mackay, I.M.; Arden, K.E. MERS Coronavirus: Diagnostics, Epidemiology and Transmission. Virol. J. 2015, 12, 222. [Google Scholar] [CrossRef] [Green Version]
- Al-Tawfiq, J.A.; Zumla, A.; Memish, Z.A. Travel Implications of Emerging Coronaviruses: SARS and MERS-CoV. Travel Med. Infect. Dis. 2014, 12, 422–428. [Google Scholar] [CrossRef]
- Lee, K.M.; Jung, K. Factors Influencing the Response to Infectious Diseases: Focusing on the Case of Sars and Mers in South Korea. Int. J. Environ. Res. Public Health 2019, 16, 1432. [Google Scholar] [CrossRef] [Green Version]
- Kim, K.H.; Tandi, T.E.; Choi, J.W.; Moon, J.M.; Kim, M.S. Middle East Respiratory Syndrome Coronavirus (MERS-CoV) Outbreak in South Korea, 2015: Epidemiology, Characteristics and Public Health Implications. J. Hosp. Infect. 2017, 95, 207–213. [Google Scholar] [CrossRef] [Green Version]
- Algaissi, A.A.; Alharbi, N.K.; Hassanain, M.; Hashem, A.M. Preparedness and Response to COVID-19 in Saudi Arabia: Building on MERS Experience. J. Infect. Public Health 2020, 13, 834–838. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention How to Protect Yourself & Others: COVID-19 (Coronavirus Disease). Available online: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html (accessed on 24 December 2020).
- Mcintosh, K. Coronavirus Disease 2019 (COVID-19): Epidemiology, Virology, and Prevention. Available online: https://www.uptodate.com/contents/coronavirus-disease-2019-covid-19-epidemiology-virology-and-prevention?topicRef=8357&source=related_link#H3874558060 (accessed on 24 December 2020).
- Güner, R.; Hasanoğlu, İ.; Aktaş, F. Covid-19: Prevention and Control Measures in Community. Turk. J. Med. Sci. 2020, 50, 571–577. [Google Scholar] [CrossRef]
- Zhu, D.; Mishra, S.R.; Han, X.; Santo, K. Social Distancing in Latin America during the COVID-19 Pandemic: An Analysis Using the Stringency Index and Google Community Mobility Reports. J. Travel Med. 2020, 27, taaa125. [Google Scholar] [CrossRef]
- Zhu, D.; Mishra, S.R.; Virani, S.S. A Way to Track Governments’ Response and People’s Mobility Changes in Response to COVID-19 Pandemic. J. Glob. Health 2020, 10, 020345. [Google Scholar] [CrossRef]
- Mendolia, S.; Stavrunova, O.; Yerokhin, O. Determinants of the Community Mobility during the COVID-19 Epidemic: The Role of Government Regulations and Information. J. Econ. Behav. Organ. 2021, 184, 199–231. [Google Scholar] [CrossRef]
- Husnayain, A.; Chuang, T.W.; Fuad, A.; Su, E.C.Y. High Variability in Model Performance of Google Relative Search Volumes in Spatially Clustered COVID-19 Areas of the USA. Int. J. Infect. Dis. 2021, 109, 269–278. [Google Scholar] [CrossRef]
- Hale, T.; Angrist, N.; Cameron-Blake, E.; Hallas, L.; Kira, B.; Majumdar, S.; Petherick, A.; Phillips, T.; Tatlow, H.; Webster, S. Oxford COVID-19 Government Response Tracker, Blavatnik School of Government. Available online: www.bsg.ox.ac.uk/covidtracker (accessed on 10 January 2021).
- Aktay, A.; Bavadekar, S.; Cossoul, G.; Davis, J.; Desfontaines, D.; Fabrikant, A.; Gabrilovich, E.; Gadepalli, K.; Gipson, B.; Guevara, M.; et al. Google COVID-19 Community Mobility Reports: Anonymization Process Description (Version 1.0). arXiv 2020, arXiv:2004.04145. [Google Scholar]
- Roser, M.; Ritchie, H.; Ortiz-Ospin, E.; Hasell, J. Coronavirus Pandemic (COVID-19). Available online: https://ourworldindata.org/coronavirus (accessed on 11 January 2021).
- Garson, G.D. Partial Least Squares: Regression & Structural Equation Models; Statistical Publishing Associates: Asheboro, NC, USA, 2016; ISBN 9781626380394. [Google Scholar]
- Hair, J., Jr.; Hult, G.T.; Ringle, C.; Sarstedt, M. A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM), 2nd ed.; SAGE Publication: Los Angeles, CA, USA, 2017; ISBN 9781483377445. [Google Scholar]
- Hair, J.F.; Risher, J.J.; Sarstedt, M.; Ringle, C.M. When to Use and How to Report the Results of PLS-SEM. Eur. Bus. Rev. 2019, 31, 2–24. [Google Scholar] [CrossRef]
- Hair, J.F.; Sarstedt, M.; Hopkins, L.; Kuppelwieser, V.G. Partial Least Squares Structural Equation Modeling (PLS-SEM): An Emerging Tool in Business Research. Eur. Bus. Rev. 2014, 26, 106–121. [Google Scholar] [CrossRef]
- Wetzels, M.; Odekerken-Schröder, G.; Van Oppen, C. Using PLS Path Modeling for Assessing Hierarchical Construct Models: Guidelines and Empirical Illustration. MIS Q. 2009, 33, 177–195. [Google Scholar] [CrossRef]
- Hu, L.; Bentler, P.M. Fit Indices in Covariance Structure Modeling: Sensitivity to Underparameterized Model Misspecification. Psychol. Methods 1998, 3, 424. [Google Scholar] [CrossRef]
- Haug, N.; Geyrhofer, L.; Londei, A.; Dervic, E.; Desvars-Larrive, A.; Loreto, V.; Pinior, B.; Thurner, S.; Klimek, P. Ranking the Effectiveness of Worldwide COVID-19 Government Interventions. Nat. Hum. Behav. 2020, 4, 1303–1312. [Google Scholar] [CrossRef]
- Pigott, D.M.; Data, O.C.; Group, W.; Plessis, L.; Faria, N.R.; Li, R. The Effect of Human Mobility and Control Measures on the COVID-19 Epidemic in China. Science 2020, 368, 493–497. [Google Scholar]
- Askitas, N.; Verheyden, B. Lockdown Strategies, Mobility Patterns and COVID-19. arXiv 2020, arXiv:2006.00531. [Google Scholar]
- Nouvellet, P.; Bhatia, S.; Cori, A.; Ainslie, K.E.C.; Baguelin, M.; Bhatt, S.; Boonyasiri, A.; Brazeau, N.F.; Cattarino, L.; Cooper, L.V.; et al. Reduction in Mobility and COVID-19 Transmission. Nat. Commun. 2021, 12, 1090. [Google Scholar] [CrossRef]
- Badr, H.S.; Du, H.; Marshall, M.; Dong, E.; Squire, M.M.; Gardner, L.M. Association between Mobility Patterns and COVID-19 Transmission in the USA: A Mathematical Modelling Study. Lancet Infect. Dis. 2020, 20, 1247–1254. [Google Scholar] [CrossRef]
- Linka, K.; Goriely, A.; Kuhl, E. Global and Local Mobility as a Barometer for COVID-19 Dynamics. Biomech. Model. Mechanobiol. 2021, 20, 651–669. [Google Scholar] [CrossRef]
- Chang, S.; Pierson, E.; Koh, P.W.; Gerardin, J.; Redbird, B.; Grusky, D.; Leskovec, J. Mobility Network Models of COVID-19 Explain Inequities and Inform Reopening. Nature 2021, 589, 82–87. [Google Scholar] [CrossRef]
- Gouglas, D.; Thanh Le, T.; Henderson, K.; Kaloudis, A.; Danielsen, T.; Hammersland, N.C.; Robinson, J.M.; Heaton, P.M.; Røttingen, J.A. Estimating the Cost of Vaccine Development against Epidemic Infectious Diseases: A Cost Minimisation Study. Lancet Glob. Health 2018, 6, e1386–e1396. [Google Scholar] [CrossRef] [Green Version]
- Hammerman, A.; Sergienko, R.; Friger, M.; Beckenstein, T.; Peretz, A.; Netzer, D.; Yaron, S.; Arbel, R. Effectiveness of the BNT162b2 Vaccine after Recovery from Covid-19. N. Engl. J. Med. 2022, 386, 1221–1229. [Google Scholar] [CrossRef]
- Bernal, J.L.; Andrews, N.; Gower, C.; Robertson, C.; Stowe, J.; Tessier, E.; Simmons, R.; Cottrell, S.; Roberts, R.; O’Doherty, M.; et al. Effectiveness of the Pfizer-BioNTech and Oxford-AstraZeneca Vaccines on Covid-19 Related Symptoms, Hospital Admissions, and Mortality in Older Adults in England: Test Negative Case-Control Study. BMJ 2021, 373, n1088. [Google Scholar] [CrossRef]
- Wright, B.J.; Tideman, S.; Diaz, G.A.; French, T.; Parsons, G.T.; Robicsek, A. Comparative Vaccine Effectiveness against Severe COVID-19 over Time in US Hospital Administrative Data: A Case-Control Study. Lancet Respir. Med. 2022, 10, 557–565. [Google Scholar] [CrossRef]
- Haldane, V.; De Foo, C.; Abdalla, S.M.; Jung, A.-S.; Tan, M.; Wu, S.; Chua, A.; Verma, M.; Shrestha, P.; Singh, S.; et al. Health Systems Resilience in Managing the COVID-19 Pandemic: Lessons from 28 Countries. Nat. Med. 2021, 27, 964–980. [Google Scholar] [CrossRef]
- Legido-Quigley, H.; Asgari, N.; Teo, Y.Y.; Leung, G.M.; Oshitani, H.; Fukuda, K.; Cook, A.R.; Hsu, L.Y.; Shibuya, K.; Heymann, D. Are High-Performing Health Systems Resilient against the COVID-19 Epidemic? Lancet 2020, 395, 848–850. [Google Scholar] [CrossRef]


| Evaluation Model | Mar–Apr | May–Jun | Jul–Aug | Sep–Oct | Nov–Dec |
|---|---|---|---|---|---|
| Cambodia | |||||
| Goodness of fit | 0.667 | 0.473 | 0.376 | 0.377 | 0.503 |
| SRMR | 0.071 | 0.050 | 0.080 | 0.000 | 0.072 |
| Q2 COVID-19 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Q2 community mobility | 0.562 | 0.455 | 0.489 | 1.000 | 0.546 |
| Q2 government response | 0.559 | 1.000 | 1.000 | 1.000 | 1.000 |
| R2 COVID-19 | 0.001 | 0.045 | 0.037 | 0.135 | 0.050 |
| R2 community mobility | 0.939 | 0.424 | 0.268 | 0.150 | 0.471 |
| Laos | |||||
| Goodness of fit | 0.685 | 0.878 | 0.242 | 0.575 | 0.624 |
| SRMR | 0.048 | 0.074 | 0.064 | 0.080 | 0.072 |
| Q2 COVID-19 | 1.000 | - | - | - | - |
| Q2 community mobility | 0.561 | 0.388 | 0.342 | 0.367 | 0.479 |
| Q2 government response | 0.603 | 1.000 | 1.000 | 1.000 | 1.000 |
| R2 COVID-19 | 0.117 | - | - | - | - |
| R2 community mobility | 0.868 | 0.844 | 0.064 | 0.394 | 0.440 |
| Myanmar | |||||
| Goodness of fit | 0.745 | 0.540 | 0.503 | 0.692 | 0.517 |
| SRMR | 0.061 | 0.052 | 0.078 | 0.080 | 0.058 |
| Q2 COVID-19 | 1.000 | 1.000 | 1.000 | 0.571 | 1.000 |
| Q2 community mobility | 0.481 | 0.422 | 0.316 | 0.537 | 0.441 |
| Q2 government response | 0.599 | 1.000 | 1.000 | 1.000 | 1.000 |
| R2 COVID-19 | 0.400 | 0.003 | 0.136 | 0.860 | 0.116 |
| R2 community mobility | 0.783 | 0.614 | 0.413 | 0.195 | 0.445 |
| Singapore | |||||
| Goodness of fit | 0.860 | 0.815 | 0.221 | 0.493 | 0.584 |
| SRMR | 0.071 | 0.073 | 0.072 | 0.080 | 0.071 |
| Q2 COVID-19 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Q2 community mobility | 0.421 | 0.427 | 0.366 | 0.426 | 0.511 |
| Q2 government response | 0.544 | 1.000 | - | 1.000 | 1.000 |
| R2 COVID-19 | 0.779 | 0.593 | 0.058 | 0.360 | 0.355 |
| R2 community mobility | 0.832 | 0.869 | - | 0.173 | 0.377 |
| Vietnam | |||||
| Goodness of fit | 0.584 | 0.461 | 0.596 | 0.383 | 0.374 |
| SRMR | 0.080 | 0.071 | 0.074 | 0.042 | 0.080 |
| Q2 COVID-19 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Q2 community mobility | 0.456 | 0.524 | 0.643 | 0.597 | 0.594 |
| Q2 government response | 0.473 | 1.000 | 0.359 | 1.000 | 0.359 |
| R2 COVID-19 | 0.150 | 0.010 | 0.399 | 0.096 | 0.058 |
| R2 community mobility | 0.633 | 0.449 | 0.396 | 0.213 | 0.263 |
| Indonesia | |||||
| Goodness of fit | 0.783 | 0.757 | 0.311 | 0.490 | 0.549 |
| SRMR | 0.078 | 0.076 | 0.055 | 0.072 | 0.076 |
| Q2 COVID-19 | 0.443 | 0.359 | 1.000 | 1.000 | 0.500 |
| Q2 community mobility | 0.417 | 0.537 | 0.608 | 0.490 | 0.361 |
| Q2 government response | 0.567 | 1.000 | 1.000 | 1.000 | 1.000 |
| R2 COVID-19 | 0.792 | 0.760 | 0.203 | 0.253 | 0.663 |
| R2 community mobility | 0.617 | 0.558 | 0.001 | 0.278 | 0.035 |
| Malaysia | |||||
| Goodness of fit | 0.685 | 0.604 | 0.281 | 0.787 | 0.647 |
| SRMR | 0.080 | 0.080 | 0.078 | 0.080 | 0.073 |
| Q2 COVID-19 | 0.344 | 1.000 | 1.000 | 0.488 | 1.000 |
| Q2 community mobility | 1.000 | 0.465 | 0.395 | 0.538 | 0.435 |
| Q2 government response | 0.426 | 1.000 | 1.000 | 1.000 | 0.437 |
| R2 COVID-19 | 0.424 | 0.270 | 0.003 | 0.741 | 0.264 |
| R2 community mobility | 0.687 | 0.525 | 0.163 | 0.649 | 0.667 |
| Philippines | |||||
| Goodness of fit | 0.815 | 0.710 | 0.402 | 0.293 | 0.588 |
| SRMR | 0.065 | 0.060 | 0.064 | 0.078 | 0.080 |
| Q2 COVID-19 | 0.388 | 1.000 | 1.000 | 1.000 | 1.000 |
| Q2 community mobility | 1.000 | 0.522 | 0.479 | 0.291 | 0.458 |
| Q2 government response | 1.000 | 1.000 | 1.000 | 1.000 | 0.526 |
| R2 COVID-19 | 0.505 | 0.557 | 0.274 | 0.066 | 0.204 |
| R2 community mobility | 0.919 | 0.486 | 0.062 | 0.120 | 0.548 |
| Thailand | |||||
| Goodness of fit | 0.726 | 0.520 | 0.375 | 0.293 | 0.625 |
| SRMR | 0.046 | 0.053 | 0.074 | 0.061 | 0.067 |
| Q2 COVID-19 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Q2 community mobility | 0.508 | 0.602 | 0.350 | 0.343 | 0.342 |
| Q2 government response | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| R2 COVID-19 | 0.143 | 0.046 | 0.032 | 0.055 | 0.262 |
| R2 community mobility | 0.953 | 0.525 | 0.271 | 0.129 | 0.576 |
| Variables | Direct/Total/Indirect Effect (Standard Deviation) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Cambodia | Indonesia | Laos | Malaysia | Myanmar | Philippines | Singapore | Thailand | Vietnam | |
| March–April (n = 61) | |||||||||
| Community mobility -> COVID-19 cases | −0.109 (0.461) | −0.220 (0.066) ** | −0.922 (0.330) ** | −0.898 (0.209) *** | −0.937 (0.162) *** | −0.918 (0.293) ** | −0.058 (0.163) | −0.273 (0.530) | −0.515 (0.174) ** |
| Government response -> COVID-19 cases | −0.097 (0.438) | 0.707 (0.059) *** | −0.792 (0.381) * | −0.330 (0.201) | −0.372 (0.155) * | −0.219 (0.299) | 0.829 (0.148) *** | 0.107 (0.519) | −0.638 (0.143) *** |
| Government response -> Community mobility | −0.969 (0.009) *** | −0.785 (0.049) *** | −0.932 (0.014) *** | −0.829 (0.022) *** | −0.885 (0.017) *** | −0.959 (0.012) *** | −0.912 (0.020) *** | −0.976 (0.006) *** | −0.795 (0.037) *** |
| Government response -> COVID-19 cases † | 0.009 (0.053) | 0.880 (0.019) *** | 0.067 (0.122) | 0.415 (0.077) *** | 0.458 (0.050) *** | 0.661 (0.055) | 0.882 (0.023) *** | 0.373 (0.090) *** | −0.228 (0.118) |
| Government response -> Community mobility -> COVID-19 cases ‡ | 0.106 (0.448) | 0.173 (0.052) ** | 0.859 (0.311) ** | 0.745 (0.189) *** | 0.830 (0.151) *** | 0.880 (0.282) ** | 0.053 (0.150) | 0.266 (0.520) | 0.410 (0.139) ** |
| May–June (n = 61) | |||||||||
| Community mobility -> COVID-19 cases | 0.147 (0.127) | 0.447 (0.074) *** | - | −0.309 (0.237) | 0.071 (0.135) | 0.327 (0.150) * | −0.672 (0.227) ** | −0.122 (0.259) | −0.109 (0.153) |
| Government response -> COVID-19 cases | 0.084 (0.105) | −0.485 (0.073) *** | - | 0.251 (0.175) | 0.022 (0.163) | −0.481 (0.146) ** | 0.104 (0.232) | 0.110 (0.227) | −0.015 (0.142) |
| Government response -> Community mobility | 0.651 (0.064) *** | −0.747 (0.033) *** | −0.919 (0.014) *** | −0.725 (0.044) *** | −0.783 (0.056) *** | −0.697 (0.047) *** | −0.932 (0.042) *** | −0.725 (0.048) *** | −0.670 (0.051) *** |
| Government response -> COVID-19 cases † | 0.180 (0.054) ** | −0.820 (0.028) *** | - | 0.475 (0.064) *** | −0.033 (0.120) | −0.708 (0.056) *** | 0.731 (0.042) *** | 0.198 (0.101) * | 0.058 (0.143) |
| Government response -> Community mobility -> COVID-19 cases ‡ | 0.096 (0.084) | −0.334 (0.055) *** | - | 0.224 (0.175) | −0.056 (0.106) | −0.228 (0.113) * | 0.627 (0.241) ** | 0.088 (0.191) | 0.073 (0.104) |
| July–August (n = 62) | |||||||||
| Community mobility -> COVID-19 cases | 0.096 (0.131) | 0.449 (0.065) *** | - | 0.016 (0.205) | −0.040 (0.189) | −0.286 (0.104) ** | −0.241 (0.106) * | −0.106 (0.130) | −0.488 (0.106) *** |
| Government response -> COVID-19 cases | −0.224 (0.105) * | 0.045 (0.118) | - | −0.058 (0.177) | 0.341 (0.145) * | −0.373 (0.153) * | - | 0.209 (0.138) | 0.199 (0.102) |
| Government response -> Community mobility | 0.518 (0.087) *** | −0.025 (0.110) | −0.252 (0.124) * | 0.404 (0.181) * | −0.643 (0.053) *** | 0.250 (0.100) * | - | 0.520 (0.073) *** | −0.629 (0.050) *** |
| Government response -> COVID-19 cases † | −0.174 (0.118) | 0.034 (0.133) | - | −0.052 (0.137) | 0.367 (0.074) *** | −0.445 (0.147) ** | - | 0.154 (0.133) | 0.506 (0.063) *** |
| Government response -> Community mobility -> COVID-19 cases ‡ | 0.050 (0.072) | −0.011 (0.052) | - | 0.006 (0.100) | 0.026 (0.125) | −0.071 (0.034) * | - | −0.055 (0.073) | 0.307 (0.077) *** |
| September–October (n = 61) | |||||||||
| Community mobility -> COVID-19 cases | −0.173 (0.098) | −0.431 (0.128) ** | - | −0.640 (0.116) *** | −0.620 (0.052) *** | −0.250 (0.112) * | −0.293 (0.097) ** | −0.059 (0.150) | 0.053 (0.168) |
| Government response -> COVID-19 cases | 0.398 (0.081) *** | 0.116 (0.141) | - | 0.257 (0.125) * | 0.468 (0.054) *** | −0.020 (0.135) | −0.416 (0.085) *** | 0.207 (0.096) * | −0.331 (0.121) ** |
| Government response -> Community mobility | 0.387 (0.117) ** | −0.527 (0.056) *** | 0.628 (0.055) *** | −0.805 (0.036) *** | −0.442 (0.082) *** | 0.347 (0.096) *** | 0.416 (0.096) *** | −0.359 (0.125) ** | 0.462 (0.088) *** |
| Government response -> COVID-19 cases † | 0.331 (0.072) *** | 0.344 (0.107) ** | - | 0.773 (0.041) *** | 0.742 (0.052) *** | −0.107 (0.125) | −0.538 (0.073) *** | 0.228 (0.101) * | −0.306 (0.082) *** |
| Government response -> Community mobility -> COVID-19 cases‡ | −0.067 (0.052) | 0.228 (0.074) ** | - | 0.515 (0.102) *** | 0.274 (0.048) *** | −0.086 (0.046) | −0.122 (0.041) ** | 0.021 (0.062) | 0.025 (0.079) |
| November–December (n = 61) | |||||||||
| Community mobility -> COVID-19 cases | 0.232 (0.434) | 0.504 (0.069) *** | - | 0.270 (0.227) | −0.206 (0.178) | −0.385 (0.181) * | 0.292 (0.119) * | 0.043 (0.132) | 0.037 (0.152) |
| Government response -> COVID-19 cases | 0.308 (0.331) | 0.552 (0.067) *** | - | −0.269 (0.215) | 0.167 (0.168) | 0.084 (0.164) | 0.369 (0.162) * | 0.544 (0.184) ** | −0.258 (0.159) |
| Government response -> Community mobility | −0.687 (0.079) *** | 0.188 (0.099) | −0.664 (0.064) *** | −0.817 (0.025) *** | −0.667 (0.053) *** | −0.740 (0.036) *** | 0.614 (0.099) *** | −0.759 (0.063) *** | 0.513 (0.062) *** |
| Government response -> COVID-19 cases † | 0.149 (0.101) | 0.646 (0.069) *** | - | −0.490 (0.099) *** | 0.305 (0.115) ** | 0.370 (0.104) *** | 0.549 (0.145) *** | 0.512 (0.157) ** | −0.239 (0.144) |
| Government response -> Community mobility -> COVID-19 cases ‡ | −0.159 (0.301) | 0.095 (0.049) | - | −0.221 (0.186) | 0.138 (0.122) | 0.285 (0.133) * | 0.180 (0.078) * | −0.033 (0.102) | 0.019 (0.080) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Widyasari, V.; Lee, C.B.; Lin, K.-H.; Husnayain, A.; Su, E.C.-Y.; Wang, J.-Y. Effects of the Government Response and Community Mobility on the COVID-19 Pandemic in Southeast Asia. Healthcare 2022, 10, 2003. https://doi.org/10.3390/healthcare10102003
Widyasari V, Lee CB, Lin K-H, Husnayain A, Su EC-Y, Wang J-Y. Effects of the Government Response and Community Mobility on the COVID-19 Pandemic in Southeast Asia. Healthcare. 2022; 10(10):2003. https://doi.org/10.3390/healthcare10102003
Chicago/Turabian StyleWidyasari, Vita, Chiachi Bonnie Lee, Kuan-Han Lin, Atina Husnayain, Emily Chia-Yu Su, and Jiun-Yi Wang. 2022. "Effects of the Government Response and Community Mobility on the COVID-19 Pandemic in Southeast Asia" Healthcare 10, no. 10: 2003. https://doi.org/10.3390/healthcare10102003
APA StyleWidyasari, V., Lee, C. B., Lin, K.-H., Husnayain, A., Su, E. C.-Y., & Wang, J.-Y. (2022). Effects of the Government Response and Community Mobility on the COVID-19 Pandemic in Southeast Asia. Healthcare, 10(10), 2003. https://doi.org/10.3390/healthcare10102003








