Advanced Level Practice Education: UK Critical Care Pharmacists’ Opinions in 2015
Abstract
:1. Introduction
2. Methodology
3. Results
3.1. Response Rate
3.2. Pharmacist Demographics
| Afc Band | Frequency, n (%) |
|---|---|
| 6 | 1 (0.6%) |
| 7 | 26 (16%) |
| 8a | 106 (65%) |
| 8b | 26 (16%) |
| 8c | 4 (2.5%) |
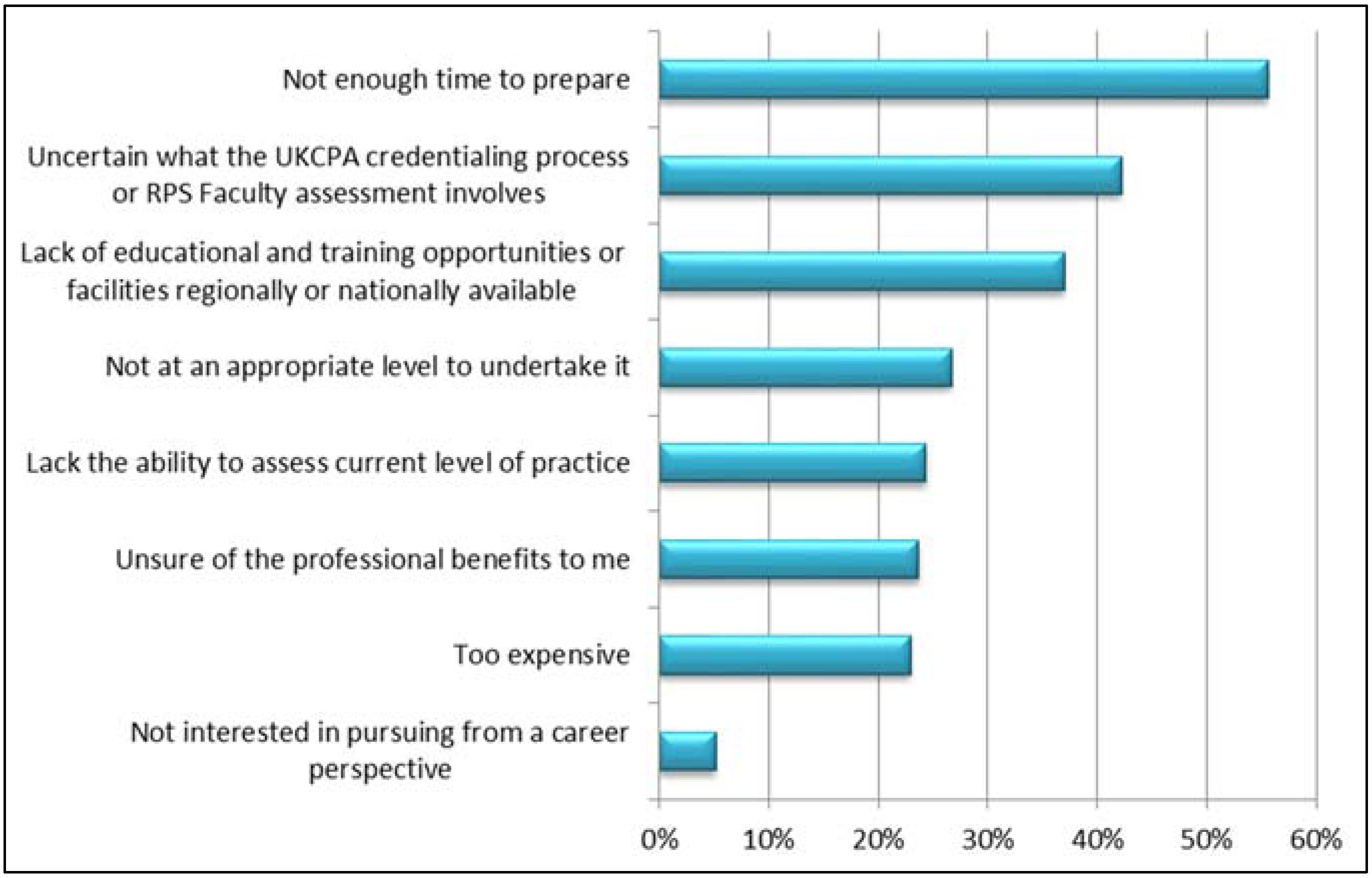
3.3. UKCPA Credentialing and RPS Faculty Accreditation
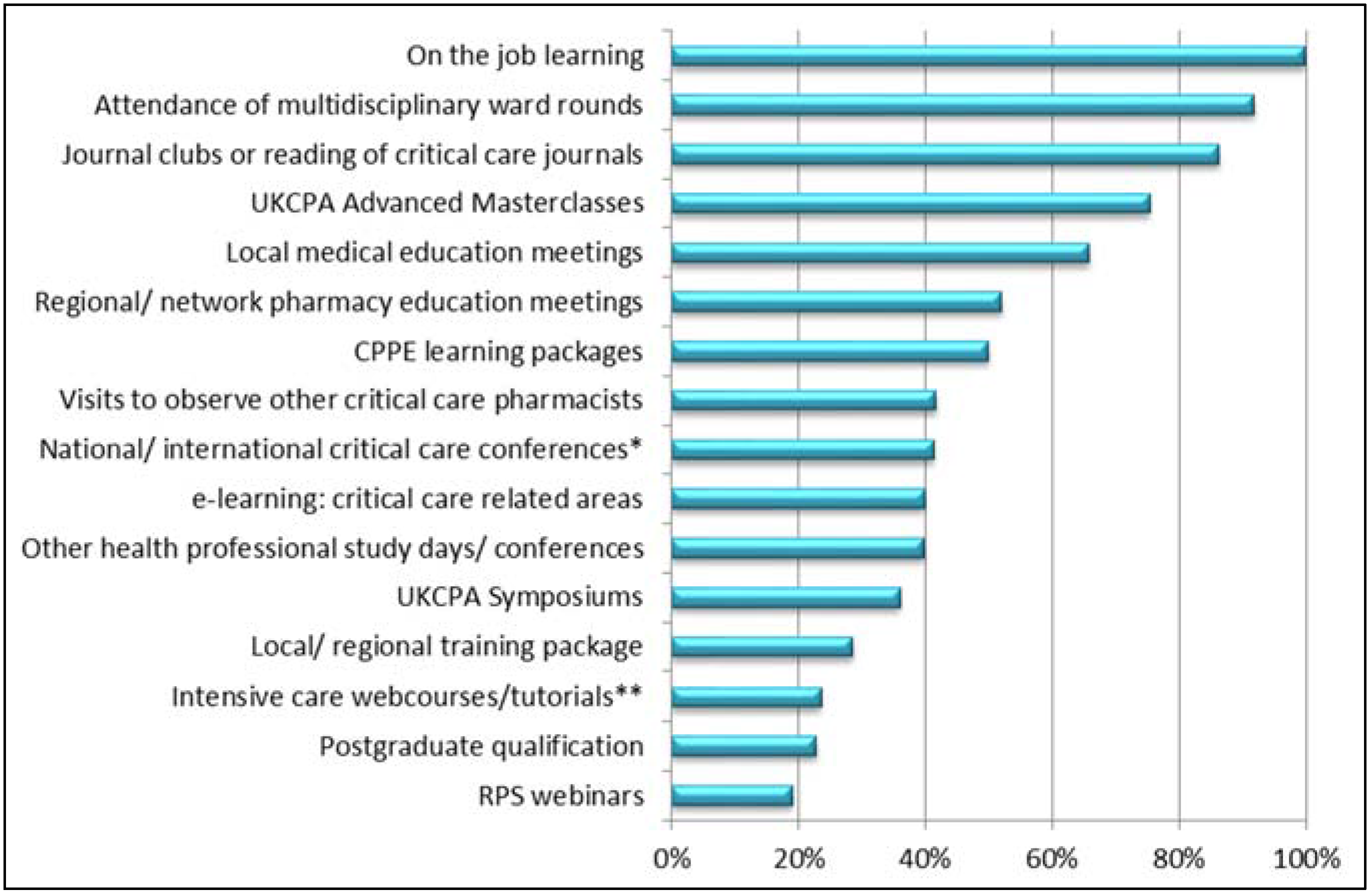
3.4. Educational Resources used for Preparation for Advanced Level Practice
3.5. National or Regional Training Programme for Advanced Level Practice
3.6. UKCPA CCG Masterclasses
| Benefits or Barriers of a Critical Care conference | Frequency n, (%) |
|---|---|
| Networking, e.g., discussing with peers, sharing best practice and providing advice (Benefit) | 110 (84%) |
| Potential for more topics to be included (Benefit) | 103 (79%) |
| Inclusion of different levels, e.g., beginners, foundation & advanced level (Benefit) | 98 (75%) |
| Potential of a more flexible format (ability to choose sessions of interest to attend) (Benefit) | 96 (73%) |
| Conference fees (Barrier) | 92 (70%) |
| Accommodation costs (Barrier) | 75 (57%) |
| Difficulty obtaining managers permission to attend due to increased number of days (Barrier) | 75 (57%) |
| Difficulty in more than one member of your team being able to attend (Barrier) | 69 (53%) |
| Ward cover would not be provided whilst away (Barrier) | 65 (50%) |
| No barriers to a critical care conference | 4 (3%) |
| No advantages to a critical care conference | 2 (2%) |
4. Discussion
Limitations
5. Conclusions
Author Contributions
Conflicts of Interest
Appendix A
| 1. Please indicate your UK country of practice. | ||||||
| ||||||
| 2. How many years of experience do you have working in critical care? | ||||||
| ||||||
| 3. Please indicate your posts AFC band: | ||||||
| ||||||
| 4. Do you work in a designated teaching hospital? | ||||||
| ||||||
5. Do you routinely work as part of a critical care pharmacy team?
| ||||||
| 6. Have you previously undertaken either the UKCPA Critical Care Group credentialing process or the Royal Pharmaceutical Society Faculty assessment? | ||||||
| ||||||
| 7. What are the important barriers for not undertaking the UKCPA CCG credentialing or RPS Faculty assessment? Select all that apply; | ||||||
| Select | ||||||
| Do not believe I am currently at an appropriate level to undertake | ||||||
| Financial burden excessive | ||||||
| Lack ability to assess my current level of practice | ||||||
| Lack of educational and training opportunities/facilities regionally or nationally available for advanced level practice | ||||||
| Not enough time to prepare for | ||||||
| Not interested in pursuing from a career perspective | ||||||
| Uncertain what the UKCPA credentialing process or RPS Faculty assessment involves | ||||||
| Unsure of the professional benefits to me | ||||||
| Comments; | ||||||
| 8. What educational resources do you use to develop your advanced level practice? For those that you use, rate how useful you find them. Where 1 is not useful and 5 is very useful | ||||||
| 1 | 2 | 3 | 4 | 5 | Do Not Use | |
| Attendance of multidisciplinary ward rounds | ||||||
| CPPE learning packages | ||||||
| e-learning—critical care-related areas | ||||||
| ESICM/ AAGBI/ SCCM webcourses/tutorials (or equivalent), e.g., PACT/learnicu.org | ||||||
| Journal clubs (e.g., local or UKCPA CCG) or regular review and reading of critical care-related journals | ||||||
| Local medical education meetings (e.g., Postgraduate Medical Education) | ||||||
| Local pharmacy educational meetings | ||||||
| Local/ regional training package (Please state origin & level in the comments box) | ||||||
| National or international critical care-related conferences, e.g., ICS, ESICM, SCCM, ISICEM meetings | ||||||
| On the job learning | ||||||
| Other health professional study days/conferences (Please state organisation in comments box) | ||||||
| Postgraduate qualification (e.g., MSc in critical care) | ||||||
| Regional or network-wide pharmacy educational meetings | ||||||
| Royal Pharmaceutical Society webinars | ||||||
| UKCPA Advanced Masterclasses | ||||||
| UKCPA Symposiums | ||||||
| Visits to other units to observe other critical care pharmacists practice | ||||||
| Others (Please state in comments box) | ||||||
| Comments; | ||||||
| 9. The current educational resources available are adequate for developing advanced level practice and for the preparation for the credentialing process. | ||||||
| ||||||
| 10. There is a need for National or regional training programmes for critical care advance level practice | ||||||
| ||||||
| 11. Have you ever attended a UKCPA critical care masterclass? | ||||||
| ||||||
| The UKCPA CCG is considering holding a critical care conference incorporating the material from the masterclass study days delivered over 2 consecutive days with a 3rd day for pre-registered candidates to undergo assessment for RPS Faculty accreditation. | ||||||
| 12. What benefits do you think a critical care conference would provide over the current system of beginner and advanced masterclasses study days? Select all that apply; | ||||||
| Select | ||||||
| Networking, e.g., discussing with peers, sharing best practice and providing advice | ||||||
| Potential for more topics to be included | ||||||
| Potential of a more flexible format (Ability to choose sessions of interest to attend) | ||||||
| Inclusion of different levels, e.g., beginners, foundation & advanced level | ||||||
| Other (Please state in comments box) | ||||||
| None | ||||||
| Comments; | ||||||
| 13. What barriers may prevent you from attending a critical care conference over the current masterclass study day system? Select all that apply; | ||||||
| Select | ||||||
| Conference fees | ||||||
| Accommodation costs | ||||||
| Ward cover would not be provided whilst away | ||||||
| Difficulty obtaining managers permission to attend due to increased number of study days | ||||||
| Difficulty in more than one member of your team being able to attend | ||||||
| Other (Please state in comments box) | ||||||
| None | ||||||
| Comments; | ||||||
| 14. Two different formats have been suggested for the critical care UKCPA conference. Please select the format you would prefer; | ||||||
| ||||||
| Comments; | ||||||
| 15. Would you be interested in attending a 3rd Day in which you were assessed for RPS Faculty accreditation? | ||||||
| ||||||
| 16. Where do you think the RPS Faculty assessment would be best placed in relation tothe conference? | ||||||
| ||||||
| 17. What would you be willing to pay for a UKCPA critical care conference fees/ day (if not fully or partially funded by your employer)? | ||||||
| ||||||
18. A UKCPA critical care conference run over 2 days would be a better way to provide critical care education over the current masterclass study days.
| ||||||
| 19. Would you be interested in attending a Critical Care UKCPA conference? | ||||||
| ||||||
References
- Young, K.; Farrell, J.; McKenzie, C.; Tomlin, M.; Borthwick, M.; Forrest, R.; Shulman, R.; Craig, M.; Offord, R.; Bourne, R.; et al. New Ways of Working—Adult Critical Care Specialist Pharmacy Practice; Department of Health and Clinical Pharmacy Association: London, UK, 2005. [Google Scholar]
- UKCPA. Critical Care Syllabus Foundation and Excellence Level. 2009. Available online: http://www.ukcpa.org.uk/docs/Critical%20Care%20Syllabus%202009.pdf (accessed on 6 October 2015).
- McKenzie, C.; Borthwick, M.; Thacker, M.; Shulman, R.; Offord, R.; Tomlin, M.; Bates, I.; McRobbie, D. Developing a process for credentialing advanced level practice in the pharmacy profession using a multi-source evaluation tool. Pharm. J. 2011, 286, 1–5. [Google Scholar]
- Royal Pharmaceutical Society (RPS). Advanced Level Framework. Available online: http://www.rpharms.com/faculty-documents/rps-advanced-pharmacy-framework-guide.pdf (accessed on 6 October 2015).
- Faculty of Intensive Care Medicine. Core Standards for Intensive Care Units. Available online: https://www.ficm.ac.uk/news-events/core-standards-intensive-care-units (accessed on 6 October 2015).
- Borthwick, M.; (Chair of UKCPA, Consultant Pharmacist, Pharmacy department, John Radcliffe Hospital, England). Personal communication, October 2015.
- Flatten, H.; Moreno, R.P.; Putensen, C.; Rhodes, A. Organisation and Management of Intensive Care; European Society of Intensive Care Medicine: Brussels, Belgium, 2010. [Google Scholar]
- The American College of Clinical Pharmacy (ACCP). White Paper. A Vision of Pharmacy’s Future Roles, Responsibilities, and Manpower Needs in the United States. Pharmacotherapy 2000, 20, 991–1022. [Google Scholar]
- Midlands Critical Care Networks. Band 7 Pharmacist Training Pack. Available online: https://www.midlandscriticalcarenetworks.nhs.uk/band-7-pharmacist-training-pack-and-log (accessed on 6 October 2015).
- Shulman, R.; McKenzie, C.A.; Landa, J.; Bourne, R.S.; Jones, A.; Borthwick, M.; Tomlin, M.; Jani, Y.H.; West, D.; Bates, I.; et al. Pharmacist’s review and outcomes: Treatment-enhancing contributions tallied, evaluated, and documented (PROTECTED-UK). J. Crit. Care 2015, 30, 808–813. [Google Scholar] [CrossRef] [PubMed]
- Billett, S. Toward a workplace pedagogy: Guidance, participation, and engagement. Adult Educ. Q. 2002, 53, 27–43. [Google Scholar] [CrossRef]
- Datta, S.T.; Davies, S.J. Training for the Future NHS: Training junior doctors in the United Kingdom within the 48-hour European working time directive. Med. Educ. 2014, 14, S12–S17. [Google Scholar] [CrossRef] [PubMed]
- Ward, M.; Gruppen, L.; Regehr, G. Measuring Self-assessment: Current State of the Art. Adv. Health Sci. Educ. 2002, 7, 63–80. [Google Scholar] [CrossRef]
- Costa, M.; Schulman, R.; Bates, I. A credentialing process for advanced level pharmacists: Participant feedback. Pharm. J. 2012, 288, 689–689. [Google Scholar]
- Childs, S.; Blenkinsopp, E.; Hall, A.; Walton, G. Effective e-learning for health professionals and students—Barriers and their solutions. A systematic review of the literature—Findings from the HeXL project. Health Inf. Libr. J. 2005, 22 (Suppl. 2), 20–32. [Google Scholar] [CrossRef] [PubMed]
- Dawes, D.; Handscomb, A. A pilot study to assess the case for e-learning in the NHS. J. Res. Nurs. 2002, 7, 428–443. [Google Scholar]
- 1The UKCPA CCG Expert Practice Development Group is comprised of UK pharmacists working at advanced or consultant-level practice in critical care pharmacy who lead the development of pharmacy practice and research in this specialty.
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Warin, R.E.; Bourne, R.S.; Borthwick, M.; Barton, G.; Bates, I. Advanced Level Practice Education: UK Critical Care Pharmacists’ Opinions in 2015. Pharmacy 2016, 4, 6. https://doi.org/10.3390/pharmacy4010006
Warin RE, Bourne RS, Borthwick M, Barton G, Bates I. Advanced Level Practice Education: UK Critical Care Pharmacists’ Opinions in 2015. Pharmacy. 2016; 4(1):6. https://doi.org/10.3390/pharmacy4010006
Chicago/Turabian StyleWarin, Ruth E., Richard S. Bourne, Mark Borthwick, Greg Barton, and Ian Bates. 2016. "Advanced Level Practice Education: UK Critical Care Pharmacists’ Opinions in 2015" Pharmacy 4, no. 1: 6. https://doi.org/10.3390/pharmacy4010006






