The Prevalence and Predictors of Low-Cost Generic Program Use in a Nationally Representative Uninsured Population
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Study Subjects and Design
2.3. Use of Low-Cost Generic Programs
2.4. Subject Characteristics
2.5. Data Analysis
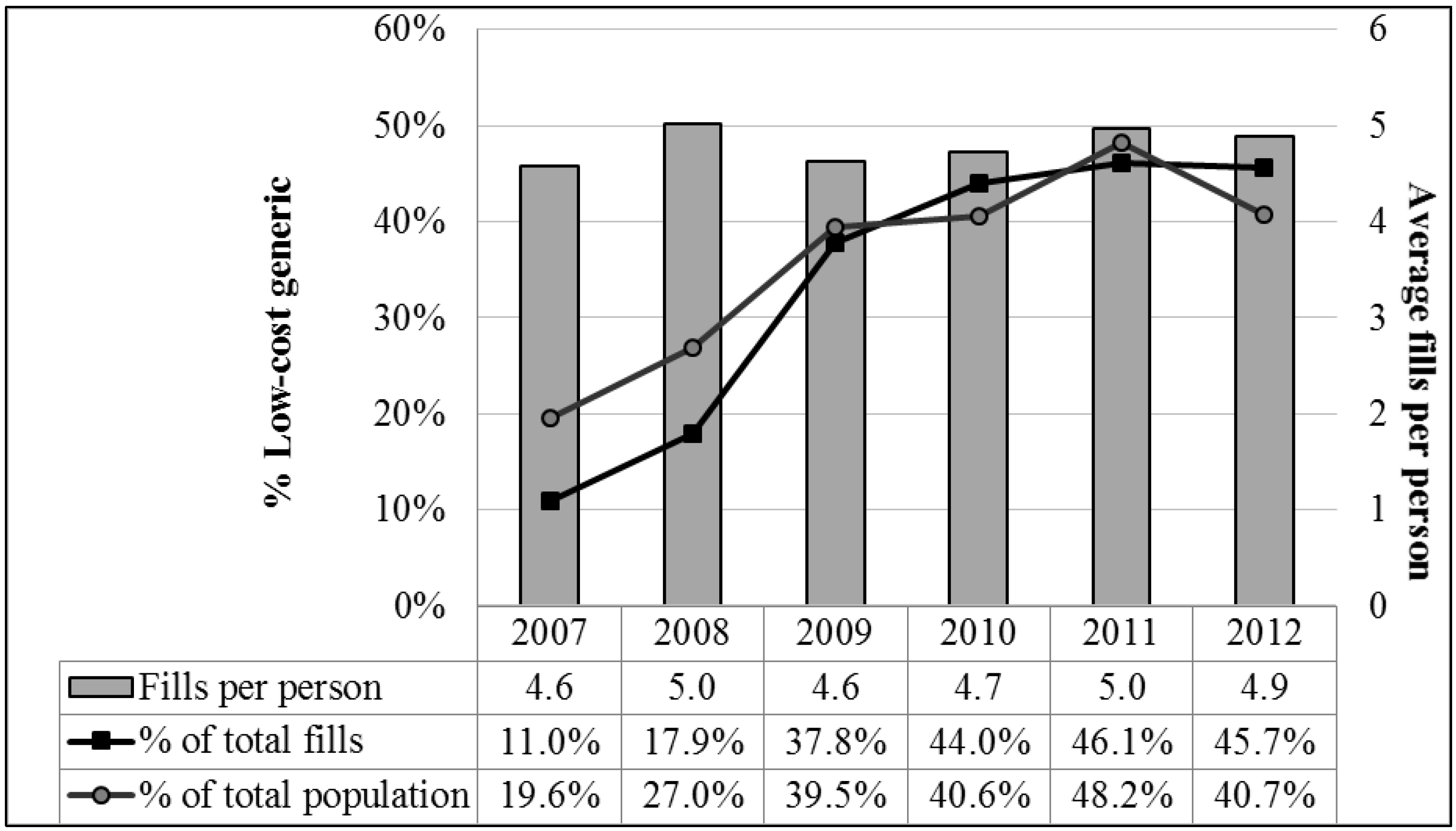
3. Results
3.1. Cohort Comparison
3.2. Predictors of LCGP Use
3.3. Medication Use
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| DOAJ | Directory of open access journals |
| FPL | Federal poverty limit |
| LCGP | Low-Cost generic program |
| LD | linear dichroism |
| MDPI | Multidisciplinary Digital Publishing Institute |
| MEPS | Medical Expenditure Panel Survey |
| MSA | Metropolitan Statistical Area |
| NDC | National Drug Code |
| TLA | Three letter acronym |
| U.S. | United States |
References
- Ayanian, J.Z.; Weissman, J.S.; Schneider, E.C.; Ginsburg, J.A.; Zaslavsky, A.M. Unmet health needs of uninsured adults in the United States. JAMA 2000, 284, 2061–2069. [Google Scholar] [CrossRef] [PubMed]
- Hadley, J. Sicker and poorer—The consequences of being uninsured: A review of the research on the relationship between health insurance, medical care use, health, work, and income. Med. Care Res. Rev. 2003, 60 (Suppl. S2), 3S–75S. [Google Scholar] [CrossRef] [PubMed]
- Baker, D.W.; Sudano, J.J.; Albert, J.M.; Borawski, E.A.; Dor, A. Lack of health insurance and decline in overall health in late middle age. N. Engl. J. Med. 2001, 345, 1106–1112. [Google Scholar] [CrossRef] [PubMed]
- Meyer, P.A.; Penman-Aguilar, A.; Campbell, V.A.; Graffunder, C.; O’Connor, A.E.; Yoon, P.W. Conclusion and future directions: CDC Health Disparities and Inequalities Report—United States, 2013. MMWR Surveill. Summ. 2013, 62 (Suppl. S3), 184–186. [Google Scholar]
- Sabik, L.M.; Dahman, B.A. Trends in care for uninsured adults and disparities in care by insurance status. Med. Care Res. Rev. 2012, 69, 215–230. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, D.A.; Hui, X.; Schneider, E.B.; Ali, M.T.; Canner, J.K.; Leeper, W.R.; Efron, D.T.; Haut, E.R.; Velopulos, C.G.; Pawlik, T.M.; et al. Worse outcomes among uninsured general surgery patients: Does the need for an emergency operation explain these disparities? Surgery 2014, 156, 345–351. [Google Scholar] [CrossRef] [PubMed]
- Heisler, M.; Wagner, T.H.; Piette, J.D. Patient strategies to cope with high prescription medication costs: Who is cutting back on necessities, increasing debt, or underusing medications? J. Behav. Med. 2005, 28, 43–51. [Google Scholar] [CrossRef] [PubMed]
- Wagner, T.H.; Heisler, M.; Piette, J.D. Prescription drug co-payments and cost-related medication underuse. Health Econ. Policy Law 2008, 3, 51–67. [Google Scholar] [CrossRef] [PubMed]
- Felland, L.E.; Reschovsky, J.D. More nonelderly Americans face problems affording prescription drugs. Track Rep. 2009, 22, 1–4. [Google Scholar] [PubMed]
- Pelaez, S.; Lamontagne, A.J.; Collin, J.; Gauthier, A.; Grad, R.M.; Blais, L.; Lavoie, K.L.; Bacon, S.L.; Ernst, P.; Guay, L.; et al. Patients’ perspective of barriers and facilitators to taking long-term controller medication for asthma: A novel taxonomy. BMC Pulm. Med. 2015, 15. [Google Scholar] [CrossRef] [PubMed]
- Choudhry, N.K.; Shrank, W.H. Four-dollar generics—Increased accessibility, impaired quality assurance. N. Engl. J. Med. 2010, 363, 1885–1887. [Google Scholar] [CrossRef] [PubMed]
- Shrank, W.H.; Liberman, J.N.; Fischer, M.A.; Girdish, C.; Brennan, T.A.; Choudhry, N.K. Physician perceptions about generic drugs. Ann. Pharmacother. 2011, 45, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Czechowski, J.L.; Tjia, J.; Triller, D.M. Deeply discounted medications: Implications of generic prescription drug wars. J. Am. Pharm. Assoc. 2010, 50, 752–757. [Google Scholar] [CrossRef] [PubMed]
- Patel, H.K.; Dwibedi, N.D.; Omojasola, A.; Sansgiry, S.S. Impact of Generic Drug Discount Programs on Managed Care Organizations. Am. J. Pharm. Benefits 2011, 3, 45–53. [Google Scholar]
- Wal-Mart Stores, Inc. $4 Generics. Available online: http://i.walmartimages.com/i/if/hmp/fusion/customer_list.pdf (accessed on 15 January 2015).
- Walgreens Co. Value-Priced Medication List. Available online: http://www.walgreens.com/images/psc/VPG_List_Update_7-25-2014.pdf (accessed on 15 January 2015).
- Rucker, N.L. $4 generics: How low, how broad, and why patient engagement is priceless. J. Am. Pharm. Assoc. 2010, 50, 761–763. [Google Scholar] [CrossRef] [PubMed]
- C.S. Mott Children’s Hospital: National Poll on Children’s Health. Nearly 70 Million Americans Using Discount Generic Rx Programs. 2008. Available online: http://mottnpch.org/reports-surveys/nearly-70-million-americans-using-discount-generic-rx-programs.pdf (accessed on 15 January 2015).
- Quan, H.; Sundararajan, V.; Halfon, P.; Fong, A.; Burnand, B.; Luthi, J.C.; Saunders, L.D.; Beck, C.A.; Feasby, T.E.; Ghali, W.A. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med. Care 2005, 43, 1130–1139. [Google Scholar] [CrossRef] [PubMed]
- Pauly, N.J.; Talbert, J.C.; Brown, J.D. The Prevalence and Predictors of Low-Cost Generic Program Use in the Pediatric Population. Drugs Real World Outcomes 2015, 2, 411–419. [Google Scholar] [CrossRef] [PubMed]
- SAS, version 9.4; statistical software; SAS Institute Inc.: Cary, NC, USA, 2013.
- Pauly, N.J.; Brown, J.D. Prevalence of Low-Cost Generic Program Use in a Nationally Representative Cohort of Privately Insured Adults. J. Manag. Care Spec. Pharm. 2015, 21, 1162–1170. [Google Scholar] [CrossRef] [PubMed]
- Freeman, J.D.; Kadiyala, S.; Bell, J.F.; Martin, D.P. The causal effect of health insurance on utilization and outcomes in adults: A systematic review of US studies. Med. Care 2008, 46, 1023–1032. [Google Scholar] [CrossRef] [PubMed]
- Baicker, K.; Chernew, M.E.; Robbins, J.A. The spillover effects of Medicare managed care: Medicare Advantage and hospital utilization. J. Health Econ. 2013, 32, 1289–1300. [Google Scholar] [CrossRef] [PubMed]
- McWilliams, J.M.; Meara, E.; Zaslavsky, A.M.; Ayanian, J.Z. Use of health services by previously uninsured Medicare beneficiaries. N. Engl. J. Med. 2007, 357, 143–153. [Google Scholar] [CrossRef] [PubMed]
- Lauffenburger, J.C.; Balasubramanian, A.; Farley, J.F.; Critchlow, C.W.; O’Malley, C.D.; Roth, M.T.; Pate, V.; Brookhart, M.A. Completeness of prescription information in US commercial claims databases. Pharmacoepidemiol. Drug Saf. 2013, 22, 899–906. [Google Scholar] [CrossRef] [PubMed]
| LCGP Users | Non-Users | |||||||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | |
| (Weighted) | (Weighted) | (Weighted) | (Weighted) | |||||
| Overall Sample: N = 2535 | ||||||||
| 1023 | 40.4 | 3,321,071 | 39.9 | 1512 | 59.6 | 5,006,619 | 60.1 | |
| Age * | ||||||||
| 0–17 | 55 | 5.4 | 197,217 | 5.9 | 130 | 8.6 | 468,222 | 9.4 |
| 18–34 | 308 | 30.1 | 1,097,996 | 33.1 | 597 | 39.5 | 2,060,812 | 41.2 |
| 35–54 | 465 | 45.5 | 1,461,488 | 44 | 637 | 42.1 | 1,955,761 | 39.1 |
| 55–64 | 180 | 17.6 | 531,079 | 16.0 | 144 | 9.5 | 509,644 | 10.2 |
| 65+ | 15 | 1.5 | 33,290 | 1.0 | 4 | 0.3 | 12,180 | 0.2 |
| Sex * | ||||||||
| Male | 413 | 40.4 | 1,473,855 | 44.4 | 753 | 49.8 | 2,766,344 | 55.3 |
| Female | 610 | 59.6 | 1,847,216 | 55.6 | 759 | 50.2 | 2,240,275 | 44.7 |
| Race | ||||||||
| White | 333 | 32.6 | 1,762,453 | 53.1 | 485 | 32.1 | 2,589,120 | 51.7 |
| Hispanic | 441 | 43.1 | 919,879 | 27.7 | 668 | 44.2 | 1,468,093 | 29.3 |
| Black | 187 | 18.3 | 429,532 | 12.9 | 252 | 16.7 | 659,446 | 13.2 |
| Asian | 38 | 3.7 | 118,957 | 3.6 | 59 | 3.9 | 157,624 | 3.1 |
| Other | 24 | 2.3 | 90,249 | 2.7 | 48 | 3.6 | 132,337 | 2.6 |
| Region | ||||||||
| Northeast | 70 | 6.8 | 270,591 | 8.1 | 153 | 10.1 | 568,708 | 11.4 |
| Midwest | 161 | 15.7 | 598,921 | 18.0 | 224 | 14.8 | 840,617 | 16.8 |
| South | 540 | 52.8 | 1,614,540 | 48.6 | 726 | 48 | 2,375,859 | 47.5 |
| West | 252 | 24.6 | 837,018 | 25.2 | 409 | 27.1 | 1,221,435 | 24.4 |
| Income Category | ||||||||
| <100% of FPL | 305 | 29.8 | 930,090 | 28.0 | 461 | 30.5 | 1,322,446 | 26.4 |
| 100% to 125% of FPL | 86 | 8.4 | 230,157 | 6.9 | 151 | 10 | 400,395 | 8.0 |
| 125% to 200% of FPL | 252 | 24.6 | 728,102 | 21.9 | 365 | 24.1 | 1,117,602 | 22.3 |
| 200% to 400% of FPL | 274 | 26.8 | 900,861 | 27.1 | 387 | 25.6 | 1,396,285 | 27.9 |
| >400% of FPL | 106 | 10.4 | 531,861 | 16.0 | 148 | 9.8 | 769,891 | 15.4 |
| MSA | ||||||||
| Rural | 153 | 15 | 587,178 | 17.7 | 227 | 15 | 885,641 | 17.7 |
| Urban | 870 | 85 | 2,733,892 | 82.3 | 1,285 | 85 | 4,120,978 | 82.3 |
| Marital Status | ||||||||
| Not Married | 563 | 55 | 2,023,346 | 60.9 | 909 | 60.1 | 3,210,180 | 64.1 |
| Married | 460 | 45 | 1,297,725 | 39.1 | 603 | 39.9 | 1,796,439 | 35.9 |
| Employment | ||||||||
| Unemployed | 366 | 35.8 | 1,144,601 | 34.5 | 547 | 36.2 | 1,680,822 | 33.6 |
| Employed | 657 | 64.2 | 2,176,469 | 65.5 | 965 | 63.8 | 3,325,797 | 66.4 |
| Education | ||||||||
| Less than High School | 345 | 33.7 | 824,719 | 24.8 | 520 | 34.4 | 1,330,469 | 26.6 |
| High School or Equivalent | 481 | 47 | 1,721,585 | 51.8 | 668 | 44.2 | 2,402,929 | 48.0 |
| Some College | 197 | 19.3 | 774,767 | 23.3 | 324 | 21.4 | 1,273,222 | 25.4 |
| MEPS Panel (years) * | ||||||||
| 12 (2007–2008) | 109 | 10.7 | 469,931 | 14.1 | 320 | 21.2 | 1,401,201 | 28 |
| 13 (2008–2009) | 243 | 23.8 | 773,787 | 23.3 | 385 | 25.5 | 1,062,261 | 21.2 |
| 14 (2009–2010) | 199 | 19.5 | 614,551 | 18.5 | 292 | 19.3 | 967,636 | 19.3 |
| 15 (2010–2011) | 210 | 20.5 | 743,519 | 22.4 | 208 | 13.8 | 707,594 | 14.1 |
| 16 (2011–2012) | 262 | 25.6 | 719,283 | 21.7 | 307 | 20.3 | 867,927 | 17.3 |
| Delays In Getting Necessary Medications | ||||||||
| No Delays | 919 | 89.8 | 2,918,531 | 87.9 | 1421 | 94 | 4,638,638 | 92.7 |
| Delays | 104 | 10.2 | 402,539 | 12.1 | 91 | 6 | 367,981 | 7.3 |
| CCI * | ||||||||
| 0–1 | 856 | 83.7 | 2,884,043 | 86.8 | 1425 | 94.2 | 4,736,873 | 94.6 |
| 2–4 | 160 | 15.6 | 424,906 | 12.8 | 65 | 4.3 | 214,697 | 4.3 |
| 5+ | 5 | 0.5 | 9106 | 0.3 | 4 | 0.3 | 9640 | 0.2 |
| Missing | 2 | 0.2 | 3016 | 0.1 | 18 | 1.2 | 45,409 | 0.9 |
| Total Number of Medication Fills * | ||||||||
| Median (IQR) | 5 (2–16) | 4.9 (1.7–16.6) | 2 (1–4) | 1.3 (1–3.5) | ||||
| Unique Medications Used * | ||||||||
| Median (IQR) | 3 (2–5) | 2.1 (1.1–4.2) | 1 (1–2) | 1 (1–1.8) | ||||
| Characteristic | Adjusted Odds Ratio | 95% Wald Confidence Limits | |
|---|---|---|---|
| Age | Lower | Upper | |
| 0–17 | Ref. | Ref. | Ref. |
| 18–34 | 1.12 | 0.63 | 2.00 |
| 35–54 | 1.20 | 0.65 | 2.22 |
| 55–64 | 1.50 | 0.75 | 2.97 |
| 65+ | 4.02 | 0.69 | 23.25 |
| Gender | |||
| Male | Ref. | Ref. | Ref. |
| Female | 1.24 | 0.99 | 1.56 |
| Marital Status | |||
| Not Married | Ref. | Ref. | Ref. |
| Married | 1.00 | 0.79 | 1.27 |
| Employment | |||
| Unemployed | Ref. | Ref. | Ref. |
| Employed | 0.98 | 0.75 | 1.28 |
| Education | |||
| Less than High School | Ref. | Ref. | Ref. |
| High School or Equivalent | 1.12 | 0.85 | 1.46 |
| Some College | 1.08 | 0.75 | 1.56 |
| Income Category | |||
| <100% of FPL | Ref. | Ref. | Ref. |
| 100% to 125% of FPL | 0.79 | 0.50 | 1.24 |
| 125% to 200% of FPL | 0.96 | 0.73 | 1.28 |
| 200% to 400% of FPL | 1.02 | 0.76 | 1.37 |
| >400% of FPL | 1.05 | 0.69 | 1.59 |
| Race | |||
| White | Ref. | Ref. | Ref. |
| Hispanic | 1.18 | 0.89 | 1.56 |
| Black | 0.93 | 0.67 | 1.30 |
| Asian | 1.36 | 0.76 | 2.44 |
| Other | 1.18 | 0.63 | 2.19 |
| MSA | |||
| Rural | Ref. | Ref. | Ref. |
| Urban | 1.11 | 0.80 | 1.53 |
| Region | |||
| Northeast | Ref. | Ref. | Ref. |
| Midwest | 1.31 | 0.88 | 1.93 |
| South | 1.27 | 0.88 | 1.83 |
| West | 1.16 | 0.79 | 1.71 |
| Panel Number (years of panel) | |||
| 12 (2007–2008) | Ref. | Ref. | Ref. |
| 13 (2008–2009) | 2.33 | 1.62 | 3.36 |
| 14 (2009–2010) | 2.31 | 1.63 | 3.29 |
| 15 (2010–2011) | 4.02 | 2.75 | 5.87 |
| 16 (2011–2012) | 2.78 | 1.92 | 4.01 |
| Delays in Getting Necessary Medications | |||
| No Delays | Ref. | Ref. | Ref. |
| Delays | 1.06 | 0.71 | 1.58 |
| CCI | |||
| 0–1 | Ref. | Ref. | Ref. |
| 2–4 | 1.49 | 0.94 | 2.37 |
| 5+ | 0.72 | 0.16 | 3.18 |
| Number of Unique Meds | 1.43 | 1.27 | 1.62 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brown, J.D.; Pauly, N.J.; Talbert, J.C. The Prevalence and Predictors of Low-Cost Generic Program Use in a Nationally Representative Uninsured Population. Pharmacy 2016, 4, 14. https://doi.org/10.3390/pharmacy4010014
Brown JD, Pauly NJ, Talbert JC. The Prevalence and Predictors of Low-Cost Generic Program Use in a Nationally Representative Uninsured Population. Pharmacy. 2016; 4(1):14. https://doi.org/10.3390/pharmacy4010014
Chicago/Turabian StyleBrown, Joshua D., Nathan J. Pauly, and Jeffery C. Talbert. 2016. "The Prevalence and Predictors of Low-Cost Generic Program Use in a Nationally Representative Uninsured Population" Pharmacy 4, no. 1: 14. https://doi.org/10.3390/pharmacy4010014
APA StyleBrown, J. D., Pauly, N. J., & Talbert, J. C. (2016). The Prevalence and Predictors of Low-Cost Generic Program Use in a Nationally Representative Uninsured Population. Pharmacy, 4(1), 14. https://doi.org/10.3390/pharmacy4010014






