Closing the Integration Gap: A Pilot for Incorporating Foundational Sciences, DEI-Decision Making, Empathy, and Communication for Congestive Heart Failure and Arrhythmia Management by Pharmacy Students
Abstract
:1. Introduction
2. Materials and Methods
2.1. Need for ICS
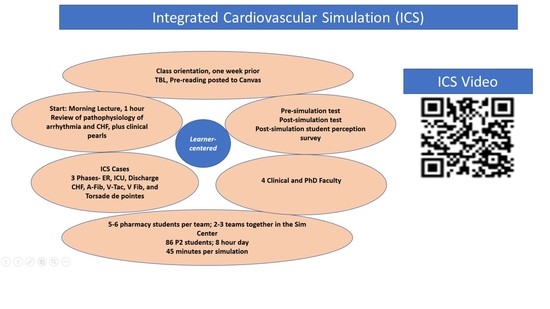
2.2. Curricular Design
2.3. Grounding ICS in Educational Theory
2.4. Case Based Learning: ACLS Patient Cases Play-Acted through Simulated Hospital Stages
2.5. Workflow and Activity Implementation
2.6. Designing the Two Patient Cases
2.6.1. Patient Cases’ Differences and Similarities and Study Plan
2.6.2. Session Planning
2.6.3. Student-to-Faculty Ratio
2.7. Quizzes, Survey Administration, Data Collection, and Statistical Analysis
3. Results
3.1. Content-Based Pre-and-Post Tests
3.2. Student Perception
3.3. Evaluating the Longer-Term Impact of ICS
4. Discussion
4.1. Framing and Contextualizing ICS
4.2. Closing the Literature Gap: Comparison of ICS with Cardiovascular Teaching Simulations
4.3. Resources for Implementation
4.4. Transferability to Other Programs
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Flexner, A. Medical Education in the United States and Canada; Science and Health Publications, Inc.: Washington, DC, USA, 1910. [Google Scholar]
- Kulasegaram, K.; Manzone, J.C.; Ku, C.; Skye, A.; Wadey, V.; Woods, N.N. Cause and effect: Testing a mechanism and method for the cognitive integration of basic science. Acad. Med. 2015, 90, S63–S69. [Google Scholar] [CrossRef] [PubMed]
- Knowles, M.S. Self-Directed Learning: A Guide for Learners and Teachers; Follett Publishing Company: Chicago, IL, USA, 1975. [Google Scholar]
- Reed, S.; Shell, R.; Kassis, K.; Tartaglia, K.; Wallihan, R.; Smith, K.; Hurtubise, L.; Martin, B.; Ledford, C.; Bradbury, S.; et al. Applying adult learning practices in medical education. Curr. Probl. Pediatr. Adolesc. Health Care 2014, 44, 170–181. [Google Scholar] [CrossRef] [PubMed]
- Cooperstein, S.E.; Kocevar-Weidinger, E. Beyond active learning: A constructivist approach to learning. Ref. Serv. Rev. 2010, 32, 141–148. [Google Scholar] [CrossRef]
- Kulasegaram, K.M.; Martimianakis, M.A.; Mylopoulos, M.; Whitehead, C.R.; Woods, N.N. Cognition before curriculum: Rethinking the integration of basic science and clinical learning. Acad. Med. 2013, 88, 1578–1585. [Google Scholar] [CrossRef]
- Wu-Pong, S.; Gobburu, J.; O’Barr, S.; Shah, K.; Huber, J.; Weiner, D. The future of the pharmaceutical sciences and graduate education: Recommendations from the AACP Graduate Education Special Interest Group. Am. J. Pharm. Educ. 2013, 77, S2. [Google Scholar] [CrossRef] [Green Version]
- Kerr, R.A. Curricular integration to enhance educational outcomes. Pharmacotherapy 2000, 20, 292S–296S. [Google Scholar] [CrossRef]
- Hopkins, R.; Pratt, D.; Bowen, J.L.; Regehr, G. Integrating basic science without integrating basic scientists: Reconsidering the place of individual teachers in curriculum reform. Acad. Med. 2015, 90, 9–153. [Google Scholar] [CrossRef]
- Hall, K.; Musing, E.; Miller, D.A.; Tisdale, J.E. Experiential training for pharmacy students: Time for a new approach. Can. J. Hosp. Pharm. 2012, 65, 285–293. [Google Scholar] [CrossRef] [Green Version]
- Medina, M.S.; Plaza, C.M.; Stowe, C.D.; Robinson, E.T.; DeLander, G.; Beck, D.E.; Melchert, R.B.; Supernaw, R.B.; Roche, V.F.; Gleason, B.L.; et al. Center for the Advancement of Pharmacy Education 2013 educational outcomes. Am. J. Pharm. Educ. 2013, 77, 162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Virani, S.S.; Alonso, A.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Delling, F.N.; et al. Heart disease and stroke statistics—2020 Update: A report from the American Heart Association. Circulation 2020, 141, e139–e596. [Google Scholar] [CrossRef] [PubMed]
- Glynn, P.; Lloyd-Jones, D.M.; Feinstein, M.J.; Carnethon, M.; Khan, S.S. Disparities in cardiovascular mortality related to heart failure in the United States. J. Am. Coll. Cardiol. 2019, 73, 2354–2355. [Google Scholar] [CrossRef]
- Khan, K.; Pattison, T.; Sherwood, M. Simulation in medical education. Med. Teach. 2011, 33, 1–3. [Google Scholar] [CrossRef]
- Davis, L.E.; Storjohann, T.D.; Spiegel, J.J.; Beiber, K.M.; Barletta, J.F. High-fidelity simulation for advanced cardiac life support training. Am. J. Pharm. Educ. 2013, 77, 59. [Google Scholar] [CrossRef] [Green Version]
- Harris, D.M.; Ryan, K.; Rabuck, C. Using a high-fidelity patient simulator with first-year medical students to facilitate learning of cardiovascular function curves. Adv. Physiol. Educ. 2012, 36, 213–219. [Google Scholar] [CrossRef]
- Al-Worafi, Y.M. (Ed.) Medication errors. In Drug Safety in Developing Countries: Achievements and Challenges; Academic Press: Cambridge, MA, USA, 2020. [Google Scholar]
- Leufer, T.; Cleary-Holdforth, J. Let’s do no harm: Medication errors in nursing: Part 1. Nurse Educ. Pract. 2013, 13, 213–216. [Google Scholar] [CrossRef]
- Farzi, S.; Abedi, H.; Ghodosi, A.; Yazdannik, A.R. Nurses’ experiences of medication errors. J. Qual. Res. Health Sci. 2014, 2, 310–319. [Google Scholar]
- Bose, D.D. An elective course in cardiovascular electrophysiology for pharmacy learners. Am. J. Pharm. Educ. 2016, 80, 130. [Google Scholar] [CrossRef]
- Woodruff, A.E.; Chilbert, M.R.; Prescott, W.A.; Wilcox, N.; Marzouk, O.; Prescott, G.M.; Slazak, E.M. Implementation and assessment of a heart failure virtual patient simulation in a required pharmacotherapy course. Am. J. Pharm. Educ. 2021, 86, 8650. [Google Scholar] [CrossRef]
- Douglass, M.A.; Casale, J.P.; Skirvin, J.A.; DiVall, M.V. A virtual patient software program to improve pharmacy student learning in a comprehensive disease management course. Am. J. Pharm. Educ. 2013, 77, 172. [Google Scholar] [CrossRef] [Green Version]
- Mieure, K.D.; Vincent, W.R., III; Cox, M.R.; Jones, M.D. A high-fidelity simulation mannequin to introduce pharmacy students to advanced cardiovascular life support. Am. J. Pharm. Educ. 2010, 74, 22. [Google Scholar] [CrossRef] [Green Version]
- Seybert, A.L.; Kobulinsky, L.R.; McKaveney, T.P. Human patient simulation in a pharmacotherapy course. Am. J. Pharm. Educ. 2008, 72, 37. [Google Scholar] [CrossRef] [Green Version]
- Maxwell, W.D.; Mohorn, P.L.; Haney, J.S.; Phillips, C.M.; Lu, Z.K.; Clark, K.; Corboy, A.; Ragucci, K.R. Impact of an advanced cardiac life support simulation laboratory experience on pharmacy student confidence and knowledge. Am. J. Pharm. Educ. 2016, 80, 140. [Google Scholar] [CrossRef]
- Bingham, A.L.; Sen, S.; Finn, L.A.; Cawley, M.J. Retention of advanced cardiac life support knowledge and skills following high-fidelity mannequin simulation training. Am. J. Pharm. Educ. 2015, 79, 12. [Google Scholar] [CrossRef] [Green Version]
- Vyas, D.; Bhutada, N.S.; Feng, X. Patient simulation to demonstrate students’ competency in core domain abilities prior to beginning advanced pharmacy practice experiences. Am. J. Pharm. Educ. 2012, 76, 176. [Google Scholar] [CrossRef]
- Vyas, D.; Wombwell, E.; Russell, E.; Caligiuri, F. High-fidelity patient simulation series to supplement introductory pharmacy practice experiences. Am. J. Pharm. Educ. 2010, 74, 169. [Google Scholar] [CrossRef] [Green Version]
- Marken, P.A.; Zimmerman, C.; Kennedy, C.; Schremmer, R.; Smith, K.V. Human simulators and standardized patients to teach difficult conversations to interprofessional health care teams. Am. J. Pharm. Educ. 2010, 74, 120. [Google Scholar] [CrossRef] [Green Version]


| Phase-I | ||
|---|---|---|
| Chief Complaint: “Lately, I feel like my heart has been racing a bit. It really doesn’t bother me that much, but I wanted to have it checked out to be sure.” | ||
| History of Present Illness: Cooper Riley is a 64-year-old Black male with heart failure and a history of persistent AFib who presents to his primary care physician complaining of palpitations that he first noticed 7 days ago. He reports that he is aware of the palpitations but that he has remained relatively asymptomatic. There has not been a noticeable change in his level of fatigue or exercise capacity during his normal daily activities. Mr. Riley has had congestive heart failure for 6 years. For the past few years, his baseline exercise capacity would be described as a slight limitation of physical activity with some symptoms during normal daily activities but asymptomatic at rest. He has a history of AFib that was cardioverted to NSR and he has been on amiodarone to maintain NSR for the past 8 months. | ||
| Past Medical History | ||
| ||
| Family History: Both parents are deceased. His father died from AMI at age 64. His mother died of breast cancer at the age of 70 years. | ||
| SH: Mr. Riley works as an accountant. He is married with two healthy children. He does not smoke but occasionally “drinks a few beers on the weekend.” His wife, who is accompanying him, only speaks Spanish. | ||
| Medications | ||
| ||
| Allergies: No known drug allergies | ||
| Phase-II-Laboratory Values | ||
| Na 140 mEq/L | Hgb 12.0 g/dL | Ca 8.5 mg/dL |
| K 4.0 mEq/L | Hct 35.8% | Mg 2.1 mEq/L |
| Cl 105 mEq/L | Plt 212 × 103/mm3 | TSH < 0.1 milliunits/L |
| CO2 24 mEq/L | WBC 9.5 × 103/mm3 | FT4 3 ng/dL |
| BUN 22 mg/dL | Polys 65% | INR 2.7 |
| SCr 1.1 mg/dL | Bands 2% | |
| Glu 109 mg/dL | Lymphs 30% | |
| Patient Case-1 Following ICS, the Student Should Be Able to: |
|
|
|
|
|
|
|
|
|
|
| Patient Case-2 Following ICS, in addition to the Learning Objectives described for Patient Case-1, the student should be able to: |
|
|
|
|
| Test Question | Pretest Number of Correct Responses N (%) | Post-test Number of Correct Responses N (%) | Change in Score (%) |
|---|---|---|---|
| Write two symptoms of CHF | 34 (50.0) | 62 (91.2) | 41.2 |
| Which of the following is true regarding atrial fibrillation? | 9 (13.2) | 8 (11.8) | −1.4 |
| Which of the following may cause atrial fibrillation? | 62 (91.2) | 60 (88.2) | −3.0 |
| Which of the following arrhythmias is depicted by the image above? (QR widening was shown) | 62 (91.2) | 66 (97.1) | 5.9 |
| For the image in question 4 above, which of the following is true? | 68 (100) | 68 (100) | 0 |
| Which of the following arrhythmias is shown in the image below? (Ventricular tachycardia was shown) | 38 (55.9) | 63 (92.6) | 36.7 |
| Mean percent correct responses | 66.9% | 80.2% | +13.3% |
| Area 1: Did ICS Enhance Learner Integration of Pathophysiology and Pharmacology with Clinical Decision Making? | |||||
|---|---|---|---|---|---|
| Question Statement | SA N (%) | A N (%) | N N (%) | D N (%) | SD |
| The review lecture prior to the simulation was helpful. | 48 (55.8) | 34 (39.5) | 3 (3.5) | 1 (1.2) | 0 (0) |
| The introduction to patient monitor and its components prior to the simulation was helpful. | 54 (62.8) | 32 (37.2) | 0 (0) | 0 (0) | 0 (0) |
| The simulation helped me learn the pathophysiology of arrhythmias. | 42 (48.8) | 31 (36.1) | 11 (12.8) | 2 (2.3) | 0 (0) |
| The simulation made me interested in clinical application. | 58 (67.4) | 22 (25.6) | 5 (5.8) | 1 (1.2) | 0 (0) |
| The simulation made the content seem more relevant to me. | 54 (62.8) | 24 (27.9) | 8 (9.3) | 0 (0) | 0 (0) |
| Area 2: Did ICS Enhance Student’s Experience of Integration–Connecting the Dots between Pharmacology and Pathophysiology and the Clinical Setting? | |||||
| Question statement | SA N (%) | A N (%) | N N (%) | D N (%) | SD |
| The simulation helped me identify different types of arrhythmias based on the ECG findings. | 44 (51.2) | 33 (38.4) | 4 (4.7) | 5 (5.8) | 0 (0) |
| The simulation helped me learn about adverse events associated with antiarrhythmic medications. | 32 (37.2) | 48 (55.8) | 3 (3.5) | 2 (2.3) | 1 (1.2) |
| The simulation helped me learn the importance of medication reconciliation and the impact of diversity factors on the same. | 42 (48.8) | 35 (40.7) | 7 (8.1) | 2 (2.3) | 0 (0) |
| The simulation enhanced my clinical decision-making process, especially in the context of diversity-related factors. | 47 (54.7) | 31 (36.1) | 6 (7.0) | 1 (1.2) | 1 (1.2) |
| The simulation improved my communication skills related to the members of the health care team. | 38 (44.2) | 35 (40.7) | 11 (12.8) | 2 (2.3) | 0 (0) |
| The simulation improved communication skills between the team and the patient. | 37 (43.0) | 27 (31.4) | 17 (19.8) | 5 (5.8) | 0 (0) |
| The case realistically simulated a situation I may encounter in clinical practice. | 49 (57.0) | 33 (38.4) | 4 (4.7) | 0 (0) | 0 (0) |
| Area 3: Assessing the Impact of ICS | |||||
| Question statement | SA N (%) | A N (%) | N N (%) | D N (%) | SD |
| The simulated case was challenging enough to intrigue my interests. | 47 (54.7) | 34 (39.5) | 4 (4.7) | 0 (0) | 1 (1.2) |
| I have enjoyed the simulation. | 47 (54.7) | 32 (37.2) | 6 (7.0) | 1 (1.2) | 0 (0) |
| I would like more simulation activities in other courses. | 48 (55.8) | 27 (31.4) | 9 (10.5) | 2 (2.3) | 0 (0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malhotra, A.; Oh, S.; Jin, Z.; Feng, X. Closing the Integration Gap: A Pilot for Incorporating Foundational Sciences, DEI-Decision Making, Empathy, and Communication for Congestive Heart Failure and Arrhythmia Management by Pharmacy Students. Pharmacy 2022, 10, 77. https://doi.org/10.3390/pharmacy10040077
Malhotra A, Oh S, Jin Z, Feng X. Closing the Integration Gap: A Pilot for Incorporating Foundational Sciences, DEI-Decision Making, Empathy, and Communication for Congestive Heart Failure and Arrhythmia Management by Pharmacy Students. Pharmacy. 2022; 10(4):77. https://doi.org/10.3390/pharmacy10040077
Chicago/Turabian StyleMalhotra, Ashim, Song Oh, Zhuqiu Jin, and Xiaodong Feng. 2022. "Closing the Integration Gap: A Pilot for Incorporating Foundational Sciences, DEI-Decision Making, Empathy, and Communication for Congestive Heart Failure and Arrhythmia Management by Pharmacy Students" Pharmacy 10, no. 4: 77. https://doi.org/10.3390/pharmacy10040077