Effect of Ghrelin on the Cardiovascular System
Abstract
:Simple Summary
Abstract
1. Introduction
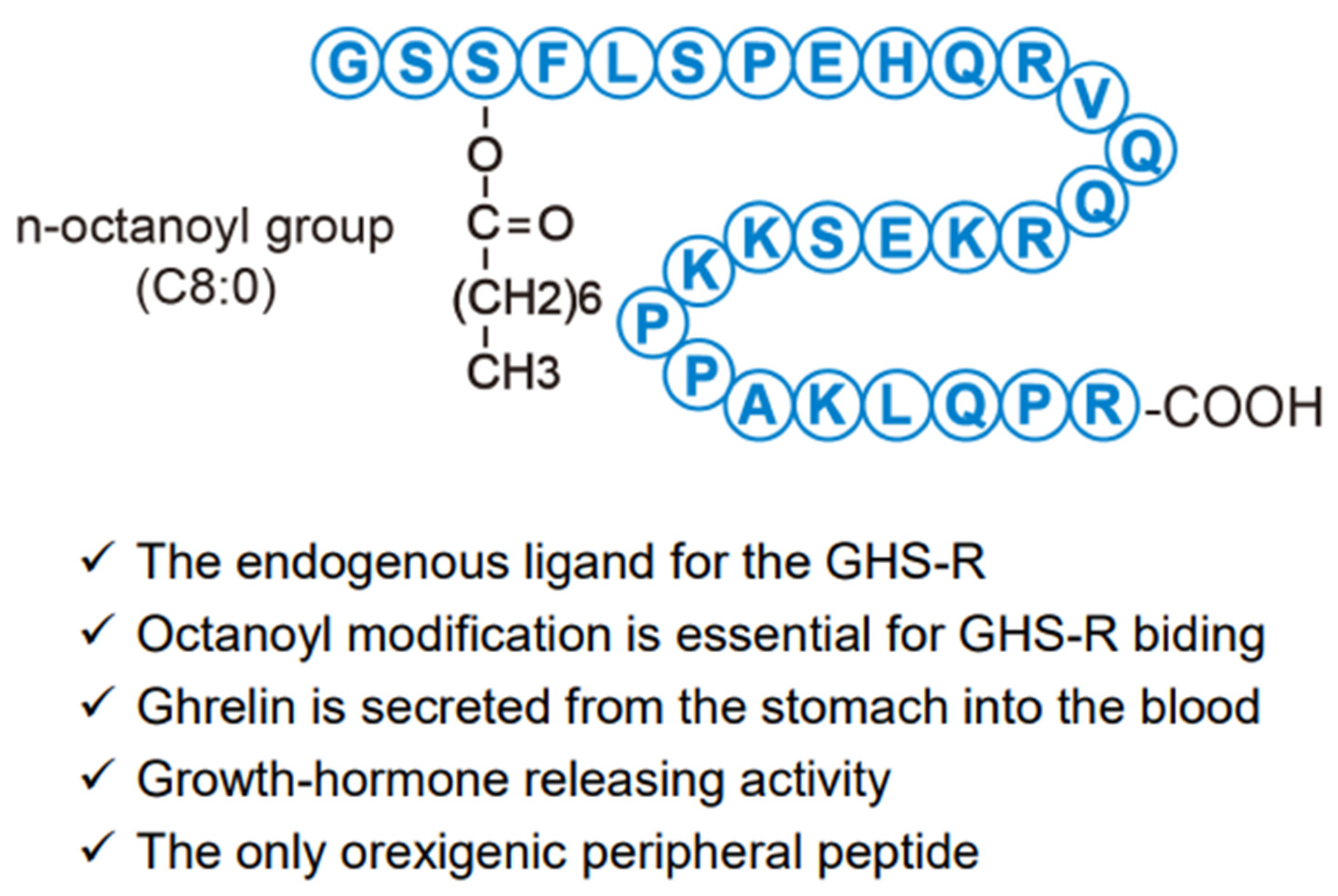
2. Characteristics of Ghrelin
3. Ghrelin Receptor
4. Mechanism of Ghrelin on GH Secretion and Feeding
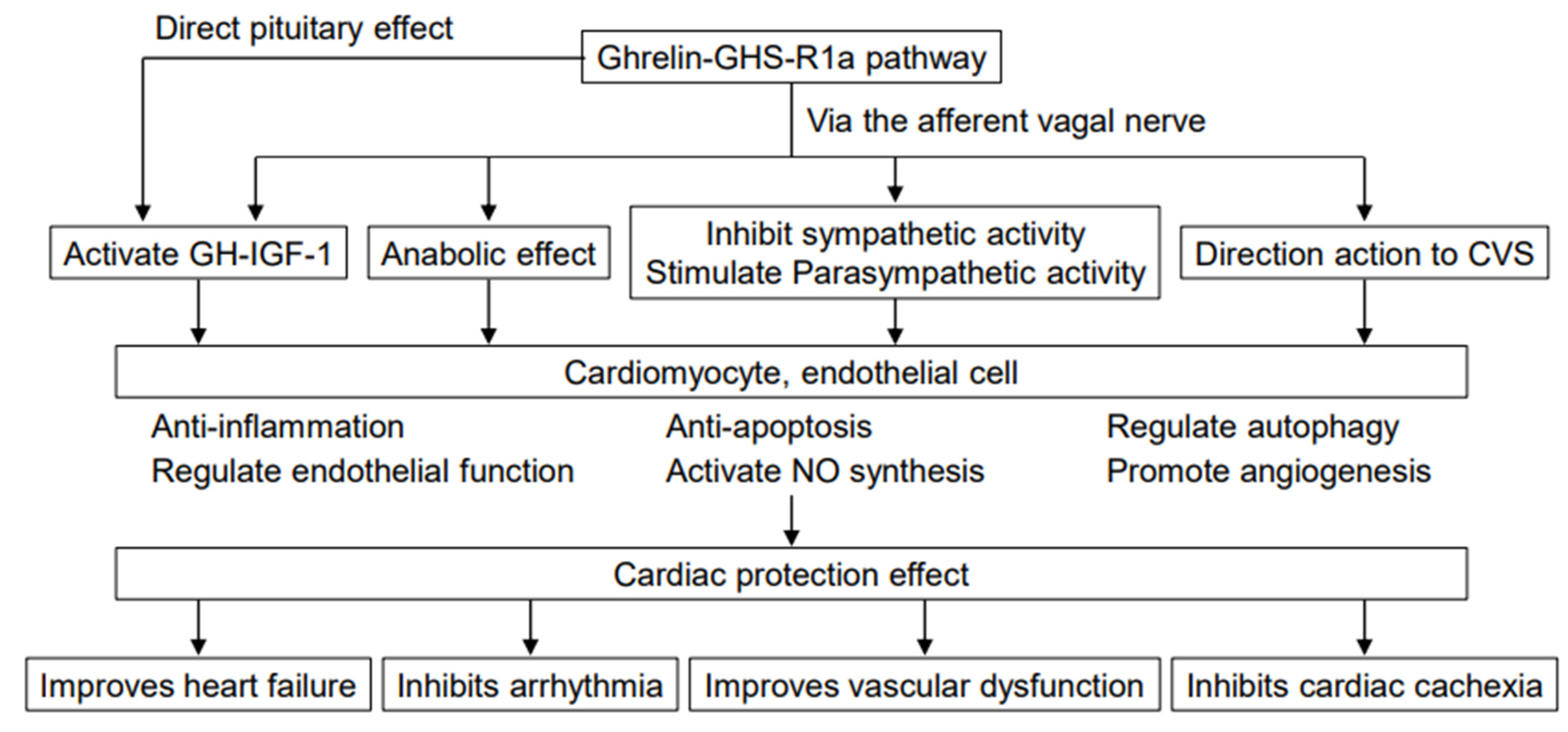
5. Effects of Ghrelin on the Cardiovascular System
5.1. Acute Effects of Ghrelin Administration
5.1.1. Effects of Ghrelin through the Sympathetic Nervous System
5.1.2. Effects of Ghrelin via GH/IGF-1
5.1.3. Direct Cardiovascular Effects of Ghrelin
5.2. Effects of Chronic Ghrelin Administration
5.2.1. Effects on Acute Myocardial Infarction
5.2.2. Effects on Heart Failure
5.2.3. Effects of Ghrelin on Alleviating Heart Failure in Humans
5.3. Role of Endogenous Ghrelin
5.4. Effects of Des-Acyl Ghrelin on the Cardiovascular System
6. Role of Ghrelin in Cachexia in Patients with Heart Failure
7. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kojima, M.; Hosoda, H.; Date, Y.; Nakazato, M.; Matsuo, H.; Kangawa, K. Ghrelin is a growth-hormone-releasing acylated peptide from stomach. Nature 1999, 402, 656–660. [Google Scholar] [CrossRef] [PubMed]
- Hosoda, H.; Kojima, M.; Mizushima, T.; Shimizu, S.; Kangawa, K. Structural divergence of human ghrelin: Identification of multiple ghrelin-derived molecules produced by post-translational processing. J. Biol. Chem. 2003, 278, 64–70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, J.; Brown, M.S.; Liang, G.; Grishin, N.V.; Goldstein, J.L. Identification of the acyltransferase that octanoylates ghrelin, an appetite-stimulating peptide hormone. Cell 2008, 132, 387–396. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kaiya, H.; Miyazato, M.; Kangawa, K.; Peter, R.E.; Unniappan, S. Ghrelin: A multifunctional hormone in non-mammalian vertebrates. Comp. Biochem. Physiol. A Mol. Integr. Physiol. 2008, 149, 109–128. [Google Scholar] [CrossRef] [PubMed]
- Date, Y.; Kojima, M.; Hosoda, H.; Sawaguchi, A.; Mondal, M.S.; Suganuma, T.; Matsukura, S.; Kangawa, K.; Nakazato, M. Ghrelin, a novel growth hormone-releasing acylated peptide, is synthesized in a distinct endocrine cell type in the gastrointestinal tracts of rats and humans. Endocrinology 2000, 141, 4255–4261. [Google Scholar] [CrossRef]
- Date, Y.; Murakami, N.; Toshinai, K.; Matsukura, S.; Niijima, A.; Matsuo, H.; Kangawa, K.; Nakazato, M. The role of the gastric afferent vagal nerve in ghrelin-induced feeding and growth hormone secretion in rats. Gastroenterology 2002, 123, 1120–1128. [Google Scholar] [CrossRef]
- Hayashida, T.; Nakahara, K.; Mondal, M.S.; Date, Y.; Nakazato, M.; Kojima, M.; Kangawa, K.; Murakami, N. Ghrelin in neonatal rats: Distribution in stomach and its possible role. J. Endocrinol. 2002, 173, 239–245. [Google Scholar] [CrossRef] [Green Version]
- Hosoda, H.; Kojima, M.; Matsuo, H.; Kangawa, K. Ghrelin and des-acyl ghrelin: Two major forms of rat ghrelin peptide in gastrointestinal tissue. Biochem. Biophys. Res. Commun. 2000, 279, 909–913. [Google Scholar] [CrossRef]
- Hosoda, H.; Doi, K.; Nagaya, N.; Okumura, H.; Nakagawa, E.; Enomoto, M.; Ono, F.; Kangawa, K. Optimum collection and storage conditions for ghrelin measurements: Octanoyl modification of ghrelin is rapidly hydrolyzed to desacyl ghrelin in blood samples. Clin. Chem. 2004, 50, 1077–1080. [Google Scholar] [CrossRef] [Green Version]
- Toshinai, K.; Mondal, M.S.; Nakazato, M.; Date, Y.; Murakami, N.; Kojima, M.; Kangawa, K.; Matsukura, S. Upregulation of Ghrelin expression in the stomach upon fasting, insulin-induced hypoglycemia, and leptin administration. Biochem. Biophys. Res. Commun. 2001, 281, 1220–1225. [Google Scholar] [CrossRef]
- Howard, A.D.; Feighner, S.D.; Cully, D.F.; Arena, J.P.; Liberator, P.A.; Rosenblum, C.I.; Hamelin, M.; Hreniuk, D.L.; Palyha, O.C.; Anderson, J.; et al. A receptor in pituitary and hypothalamus that functions in growth hormone release. Science 1996, 273, 974–977. [Google Scholar] [CrossRef] [PubMed]
- Camiña, J.P. Cell biology of the ghrelin receptor. J. Neuroendocrinol. 2006, 18, 65–76. [Google Scholar] [CrossRef] [PubMed]
- Callaghan, B.; Furness, J.B. Novel and conventional receptors for ghrelin, desacyl-ghrelin, and pharmacologically related compounds. Pharmacol. Rev. 2014, 66, 984–1001. [Google Scholar] [CrossRef]
- Guan, X.M.; Yu, H.; Palyha, O.C.; McKee, K.K.; Feighner, S.D.; Sirinathsinghji, D.J.; Smith, R.G.; Van der Ploeg, L.H.; Howard, A.D. Distribution of mRNA encoding the growth hormone secretagogue receptor in brain and peripheral tissues. Brain Res. Mol. Brain Res. 1997, 48, 23–29. [Google Scholar] [CrossRef]
- Papotti, M.; Ghè, C.; Cassoni, P.; Catapano, F.; Deghenghi, R.; Ghigo, E.; Muccioli, G. Growth hormone secretagogue binding sites in peripheral human tissues. J. Clin. Endocrinol. Metab. 2000, 85, 3803–3807. [Google Scholar] [CrossRef]
- Katugampola, S.D.; Pallikaros, Z.; Davenport, A.P. [125I-His9]-ghrelin, a novel radioligand for localizing GHS orphan receptors in human and rat tissue: Up-regulation of receptors with athersclerosis. Br. J. Pharmacol. 2001, 134, 143–149. [Google Scholar] [CrossRef] [Green Version]
- Callaghan, B.; Hunne, B.; Hirayama, H.; Sartor, D.M.; Nguyen, T.V.; Abogadie, F.C.; Ferens, D.; McIntyre, P.; Ban, K.; Baell, J.; et al. Sites of action of ghrelin receptor ligands in cardiovascular control. Am. J. Physiol. Heart Circ. Physiol. 2012, 303, H1011–H1021. [Google Scholar] [CrossRef] [Green Version]
- Baldanzi, G.; Filigheddu, N.; Cutrupi, S.; Catapano, F.; Bonissoni, S.; Fubini, A.; Malan, D.; Baj, G.; Granata, R.; Broglio, F.; et al. Ghrelin and des-acyl ghrelin inhibit cell death in cardiomyocytes and endothelial cells through ERK1/2 and PI 3-kinase/AKT. J Cell Biol. 2002, 159, 1029–1037. [Google Scholar] [CrossRef] [Green Version]
- Pei, X.M.; Yung, B.Y.; Yip, S.P.; Chan, L.W.; Wong, C.S.; Ying, M.; Siu, P.M. Protective effects of desacyl ghrelin on diabetic cardiomyopathy. Acta Diabetol. 2015, 52, 293–306. [Google Scholar] [CrossRef]
- Porporato, P.E.; Filigheddu, N.; Reano, S.; Ferrara, M.; Angelino, E.; Gnocchi, V.F.; Prodam, F.; Ronchi, G.; Fagoonee, S.; Fornaro, M.; et al. Acylated and unacylated ghrelin impair skeletal muscle atrophy in mice. J. Clin. Investig. 2013, 123, 611–622. [Google Scholar] [CrossRef] [Green Version]
- Schwartz, M.W.; Woods, S.C.; Porte, D., Jr.; Seeley, R.J.; Baskin, D.G. Central nervous system control of food intake. Nature 2000, 404, 661–671. [Google Scholar] [CrossRef]
- Nakazato, M.; Murakami, N.; Date, Y.; Kojima, M.; Matsuo, H.; Kangawa, K.; Matsukura, S. A role for ghrelin in the central regulation of feeding. Nature 2001, 409, 194–198. [Google Scholar] [CrossRef] [PubMed]
- Date, Y.; Shimbara, T.; Koda, S.; Toshinai, K.; Ida, T.; Murakami, N.; Miyazato, M.; Kokame, K.; Ishizuka, Y.; Ishida, Y.; et al. Peripheral ghrelin transmits orexigenic signals through the noradrenergic pathway from the hindbrain to the hypothalamus. Cell Metab. 2006, 4, 323–331. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Masuda, Y.; Tanaka, T.; Inomata, N.; Ohnuma, N.; Tanaka, S.; Itoh, Z.; Hosoda, H.; Kojima, M.; Kangawa, K. Ghrelin stimulates gastric acid secretion and motility in rats. Biochem. Biophys. Res. Commun. 2000, 276, 905–908. [Google Scholar] [CrossRef] [PubMed]
- Asakawa, A.; Inui, A.; Kaga, T.; Yuzuriha, H.; Nagata, T.; Ueno, N.; Makino, S.; Fujimiya, M.; Niijima, A.; Fujino, M.A.; et al. Ghrelin is an appetite-stimulatory signal from stomach with structural resemblance to motilin. Gastroenterology 2001, 120, 337–345. [Google Scholar] [CrossRef]
- Broglio, F.; Arvat, E.; Benso, A.; Gottero, C.; Muccioli, G.; Papotti, M.; van der Lely, A.J.; Deghenghi, R.; Ghigo, E. Ghrelin, a natural GH secretagogue produced by the stomach, induces hyperglycemia and reduces insulin secretion in humans. J. Clin. Endocrinol. Metab. 2001, 86, 5083–5086. [Google Scholar] [CrossRef]
- Shirai, M.; Joe, N.; Tsuchimochi, H.; Sonobe, T.; Schwenke, D.O. Ghrelin Supresses Sympathetic Hyperexcitation in Acute Heart Failure in Male Rats: Assessing Centrally and Peripherally Mediated Pathways. Endocrinology 2015, 156, 3309–3316. [Google Scholar] [CrossRef]
- Mano-Otagiri, A.; Ohata, H.; Iwasaki-Sekino, A.; Nemoto, T.; Shibasaki, T. Ghrelin suppresses noradrenaline release in the brown adipose tissue of rats. J. Endocrinol. 2009, 201, 341–349. [Google Scholar] [CrossRef]
- Nagaya, N.; Kojima, M.; Uematsu, M.; Yamagishi, M.; Hosoda, H.; Oya, H.; Hayashi, Y.; Kangawa, K. Hemodynamic and hormonal effects of human ghrelin in healthy volunteers. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2001, 280, R1483–R1487. [Google Scholar] [CrossRef] [Green Version]
- Nagaya, N.; Uematsu, M.; Kojima, M.; Ikeda, Y.; Yoshihara, F.; Shimizu, W.; Hosoda, H.; Hirota, Y.; Ishida, H.; Mori, H.; et al. Chronic administration of ghrelin improves left ventricular dysfunction and attenuates development of cardiac cachexia in rats with heart failure. Circulation 2001, 104, 1430–1435. [Google Scholar] [CrossRef] [Green Version]
- Shimizu, S.; Akiyama, T.; Kawada, T.; Sonobe, T.; Kamiya, A.; Shishido, T.; Tokudome, T.; Hosoda, H.; Shirai, M.; Kangawa, K.; et al. Centrally administered ghrelin activates cardiac vagal nerve in anesthetized rabbits. Auton. Neurosci. 2011, 162, 60–65. [Google Scholar] [CrossRef] [PubMed]
- Matsumura, K.; Tsuchihashi, T.; Fujii, K.; Abe, I.; Iida, M. Central ghrelin modulates sympathetic activity in conscious rabbits. Hypertension 2002, 40, 694–699. [Google Scholar] [CrossRef] [Green Version]
- Ishizaki, S.; Murase, T.; Sugimura, Y.; Kakiya, S.; Yokoi, H.; Tachikawa, K.; Arima, H.; Miura, Y.; Oiso, Y. Role of ghrelin in the regulation of vasopressin release in conscious rats. Endocrinology 2002, 143, 1589–1593. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Matsumura, K.; Fukuhara, M.; Kagiyama, S.; Fujii, K.; Iida, M. Ghrelin acts at the nucleus of the solitary tract to decrease arterial pressure in rats. Hypertension 2004, 43, 977–982. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saccà, L.; Cittadini, A.; Fazio, S. Growth hormone and the heart. Endocr. Rev. 1994, 15, 555–573. [Google Scholar] [CrossRef]
- Ren, J.; Samson, W.K.; Sowers, J.R. Insulin-like growth factor I as a cardiac hormone: Physiological and pathophysiological implications in heart disease. J. Mol. Cell. Cardiol. 1999, 31, 2049–2061. [Google Scholar] [CrossRef]
- Nyström, H.C.; Klintland, N.; Caidahl, K.; Bergström, G.; Wickman, A. Short-term administration of growth hormone (GH) lowers blood pressure by activating eNOS/nitric oxide (NO)-pathway in male hypophysectomized (Hx) rats. BMC Physiol. 2005, 5, 17. [Google Scholar] [CrossRef] [Green Version]
- Okumura, H.; Nagaya, N.; Enomoto, M.; Nakagawa, E.; Oya, H.; Kangawa, K. Vasodilatory effect of ghrelin, an endogenous peptide from the stomach. J. Cardiovasc. Pharmacol. 2002, 39, 779–783. [Google Scholar] [CrossRef]
- Shimizu, Y.; Nagaya, N.; Teranishi, Y.; Imazu, M.; Yamamoto, H.; Shokawa, T.; Kangawa, K.; Kohno, N.; Yoshizumi, M. Ghrelin improves endothelial dysfunction through growth hormone-independent mechanisms in rats. Biochem. Biophys. Res. Commun. 2003, 310, 830–835. [Google Scholar] [CrossRef]
- Conconi, M.T.; Nico, B.; Guidolin, D.; Baiguera, S.; Spinazzi, R.; Rebuffat, P.; Malendowicz, L.K.; Vacca, A.; Carraro, G.; Parnigotto, P.P.; et al. Ghrelin inhibits FGF-2-mediated angiogenesis in vitro and in vivo. Peptides 2004, 25, 2179–2185. [Google Scholar] [CrossRef]
- Wiley, K.E.; Davenport, A.P. Comparison of vasodilators in human internal mammary artery: Ghrelin is a potent physiological antagonist of endothelin-1. Br. J. Pharmacol. 2002, 136, 1146–1152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shinde, U.A.; Desai, K.M.; Yu, C.; Gopalakrishnan, V. Nitric oxide synthase inhibition exaggerates the hypotensive response to ghrelin: Role of calcium-activated potassium channels. J. Hypertens. 2005, 23, 779–784. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Fang, W.Y.; Qu, X.K.; Yuan, F.; Wang, W.G.; Fei, J.; Wang, Z.G. AMPK activity is down-regulated in endothelial cells of GHS-R−/− mice. Int. J. Clin. Exp. Pathol. 2013, 6, 1770–1780. [Google Scholar] [PubMed]
- Pemberton, C.J.; Tokola, H.; Bagi, Z.; Koller, A.; Pöntinen, J.; Ola, A.; Vuolteenaho, O.; Szokodi, I.; Ruskoaho, H. Ghrelin induces vasoconstriction in the rat coronary vasculature without altering cardiac peptide secretion. Am. J. Physiol. Heart Circ. Physiol. 2004, 287, H1522–H1529. [Google Scholar] [CrossRef] [PubMed]
- Grossini, E.; Molinari, C.; Mary, D.A.; Ghigo, E.; Bona, G.; Vacca, G. Intracoronary ghrelin infusion decreases coronary blood flow in anesthetized pigs. Endocrinology 2007, 148, 806–812. [Google Scholar] [CrossRef] [Green Version]
- Kanamoto, N.; Akamizu, T.; Hosoda, H.; Hataya, Y.; Ariyasu, H.; Takaya, K.; Hosoda, K.; Saijo, M.; Moriyama, K.; Shimatsu, A.; et al. Substantial production of ghrelin by a human medullary thyroid carcinoma cell line. J. Clin. Endocrinol. Metab. 2001, 86, 4984–4990. [Google Scholar] [CrossRef]
- Schwenke, D.O.; Tokudome, T.; Kishimoto, I.; Horio, T.; Shirai, M.; Cragg, P.A.; Kangawa, K. Early ghrelin treatment after myocardial infarction prevents an increase in cardiac sympathetic tone and reduces mortality. Endocrinology 2008, 149, 5172–5176. [Google Scholar] [CrossRef] [Green Version]
- Soeki, T.; Kishimoto, I.; Schwenke, D.O.; Tokudome, T.; Horio, T.; Yoshida, M.; Hosoda, H.; Kangawa, K. Ghrelin suppresses cardiac sympathetic activity and prevents early left ventricular remodeling in rats with myocardial infarction. Am. J. Physiol. Heart Circ. Physiol. 2008, 294, H426–H432. [Google Scholar] [CrossRef] [Green Version]
- Yuan, M.J.; Huang, H.; Tang, Y.H.; Wu, G.; Gu, Y.W.; Chen, Y.J.; Huang, C.X. Effects of ghrelin on Cx43 regulation and electrical remodeling after myocardial infarction in rats. Peptides 2011, 32, 2357–2361. [Google Scholar] [CrossRef]
- Soeki, T.; Niki, T.; Uematsu, E.; Bando, S.; Matsuura, T.; Kusunose, K.; Ise, T.; Ueda, Y.; Tomita, N.; Yamaguchi, K.; et al. Ghrelin protects the heart against ischemia-induced arrhythmias by preserving connexin-43 protein. Heart Vessels 2013, 28, 795–801. [Google Scholar] [CrossRef]
- Mao, Y.; Tokudome, T.; Otani, K.; Kishimoto, I.; Nakanishi, M.; Hosoda, H.; Miyazato, M.; Kangawa, K. Ghrelin prevents incidence of malignant arrhythmia after acute myocardial infarction through vagal afferent nerves. Endocrinology 2012, 153, 3426–3434. [Google Scholar] [CrossRef] [PubMed]
- Nagaya, N.; Moriya, J.; Yasumura, Y.; Uematsu, M.; Ono, F.; Shimizu, W.; Ueno, K.; Kitakaze, M.; Miyatake, K.; Kangawa, K. Effects of ghrelin administration on left ventricular function, exercise capacity, and muscle wasting in patients with chronic heart failure. Circulation 2004, 110, 3674–3679. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mao, Y.; Tokudome, T.; Otani, K.; Kishimoto, I.; Miyazato, M.; Kangawa, K. Excessive sympathoactivation and deteriorated heart function after myocardial infarction in male ghrelin knockout mice. Endocrinology 2013, 154, 1854–1863. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mao, Y.; Tokudome, T.; Kishimoto, I.; Otani, K.; Nishimura, H.; Yamaguchi, O.; Otsu, K.; Miyazato, M.; Kangawa, K. Endogenous ghrelin attenuates pressure overload-induced cardiac hypertrophy via a cholinergic anti-inflammatory pathway. Hypertension 2015, 65, 1238–1244. [Google Scholar] [CrossRef]
- Wang, M.; Qian, L.; Li, J.; Ming, H.; Fang, L.; Li, Y.; Zhang, M.; Xu, Y.; Ban, Y.; Zhang, W.; et al. GHSR deficiency exacerbates cardiac fibrosis: Role in macrophage inflammasome activation and myofibroblast differentiation. Cardiovasc. Res. 2020, 116, 2091–2102. [Google Scholar] [CrossRef]
- Nonaka, M.; Kurebayashi, N.; Murayama, T.; Sugihara, M.; Terawaki, K.; Shiraishi, S.; Miyano, K.; Hosoda, H.; Kishida, S.; Kangawa, K.; et al. Therapeutic potential of ghrelin and des-acyl ghrelin against chemotherapy-induced cardiotoxicity. Endocr. J. 2017, 64, S35–S39. [Google Scholar] [CrossRef] [Green Version]
- Evans, W.J.; Morley, J.E.; Argilés, J.; Bales, C.; Baracos, V.; Guttridge, D.; Jatoi, A.; Kalantar-Zadeh, K.; Lochs, H.; Mantovani, G.; et al. Cachexia: A new definition. Clin. Nutr. 2008, 27, 793–799. [Google Scholar] [CrossRef]
- Levine, B.; Kalman, J.; Mayer, L.; Fillit, H.M.; Packer, M. Elevated circulating levels of tumor necrosis factor in severe chronic heart failure. N. Engl. J. Med. 1990, 323, 236–241. [Google Scholar] [CrossRef]
- Loncar, G.; Fülster, S.; von Haehling, S.; Popovic, V. Metabolism and the heart: An overview of muscle, fat, and bone metabolism in heart failure. Int. J. Cardiol. 2013, 162, 77–85. [Google Scholar] [CrossRef]
- Doehner, W.; Frenneaux, M.; Anker, S.D. Metabolic impairment in heart failure: The myocardial and systemic perspective. J. Am. Coll. Cardiol. 2014, 64, 1388–1400. [Google Scholar] [CrossRef]
- Muccioli, G.; Tschöp, M.; Papotti, M.; Deghenghi, R.; Heiman, M.; Ghigo, E. Neuroendocrine and peripheral activities of ghrelin: Implications in metabolism and obesity. Eur. J. Pharmacol. 2002, 440, 235–254. [Google Scholar] [CrossRef]
- Schwartz, G.J. The role of gastrointestinal vagal afferents in the control of food intake: Current prospects. Nutrition 2000, 16, 866–873. [Google Scholar] [CrossRef]
- von Haehling, S.; Anker, S.D. Treatment of cachexia: An overview of recent developments. Int. J. Cardiol. 2015, 184, 736–742. [Google Scholar] [CrossRef] [PubMed]
- Attanasio, P.; Anker, S.D.; Doehner, W.; von Haehling, S. Hormonal consequences and prognosis of chronic heart failure. Curr. Opin. Endocrinol. Diabetes Obes. 2011, 18, 224–230. [Google Scholar] [CrossRef]
- Nagaya, N.; Kangawa, K. Ghrelin improves left ventricular dysfunction and cardiac cachexia in heart failure. Curr. Opin. Pharmacol. 2003, 3, 146–151. [Google Scholar] [CrossRef]
- Nagaya, N.; Kangawa, K. Therapeutic potential of ghrelin in the treatment of heart failure. Drugs 2006, 66, 439–448. [Google Scholar] [CrossRef]
- Shintani, M.; Ogawa, Y.; Ebihara, K.; Aizawa-Abe, M.; Miyanaga, F.; Takaya, K.; Hayashi, T.; Inoue, G.; Hosoda, K.; Kojima, M.; et al. Ghrelin, an endogenous growth hormone secretagogue, is a novel orexigenic peptide that antagonizes leptin action through the activation of hypothalamic neuropeptide Y/Y1 receptor pathway. Diabetes 2001, 50, 227–232. [Google Scholar] [CrossRef] [Green Version]
- Palus, S.; Schur, R.; Akashi, Y.J.; Bockmeyer, B.; Datta, R.; Halem, H.; Dong, J.; Culler, M.D.; Adams, V.; Anker, S.D.; et al. Ghrelin and its analogues, BIM-28131 and BIM-28125, improve body weight and regulate the expression of MuRF-1 and MAFbx in a rat heart failure model. PLoS ONE 2011, 6, e26865. [Google Scholar] [CrossRef]
- Lenk, K.; Palus, S.; Schur, R.; Datta, R.; Dong, J.; Culler, M.D.; Anker, S.; Springer, J.; Schuler, G.; Adams, V. Effect of ghrelin and its analogues, BIM-28131 and BIM-28125, on the expression of myostatin in a rat heart failure model. J. Cachexia Sarcopenia Muscle 2013, 4, 63–69. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hosoda, H. Effect of Ghrelin on the Cardiovascular System. Biology 2022, 11, 1190. https://doi.org/10.3390/biology11081190
Hosoda H. Effect of Ghrelin on the Cardiovascular System. Biology. 2022; 11(8):1190. https://doi.org/10.3390/biology11081190
Chicago/Turabian StyleHosoda, Hiroshi. 2022. "Effect of Ghrelin on the Cardiovascular System" Biology 11, no. 8: 1190. https://doi.org/10.3390/biology11081190




