Development of Smart-Ring-Based Chest Compression Depth Feedback Device for High Quality Chest Compressions: A Proof-of-Concept Study
Abstract
1. Introduction
2. Methods
2.1. Hardware System of the CPR Smart Ring
2.2. Chest Compression Depth Estimation Algorithm
2.2.1. Extraction of the Movement Component in an Acceleration Signal
2.2.2. CCD Estimation Using a Three-Axis Accelerometer
2.3. Experimental Settings to Evaluate the Accuracy of the Proposed Depth Feedback System
2.4. CPR Pilot Test Using an Adult/Infant Mannequin
3. Results
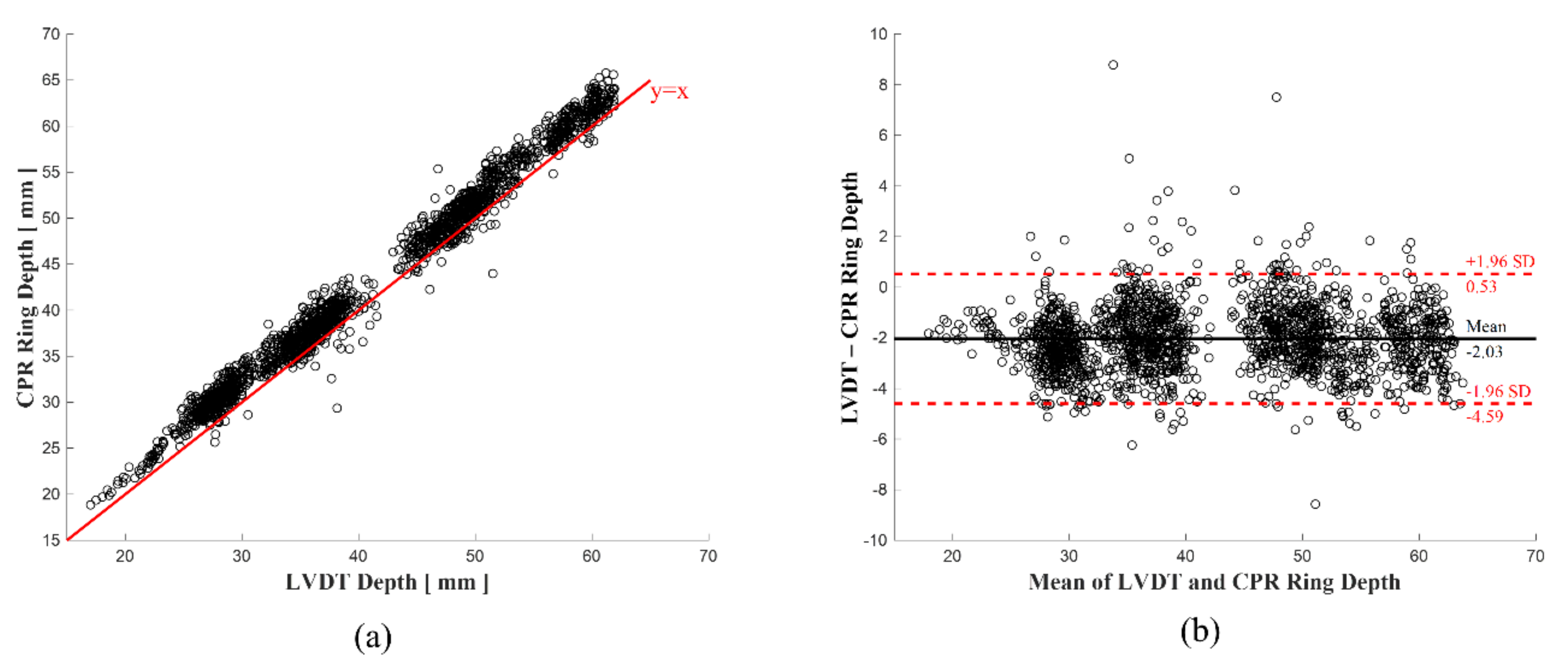
3.1. Accuracy of Estimated Depth of the Ring-Based CCD Feedback System
3.2. Accuracy in the CPR Pilot Test with Mannequins
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Neumar, R.W.; Shuster, M.; Callaway, C.W.; Gent, L.M.; Atkins, D.L.; Bhanji, F.; Brooks, S.C.; de Caen, A.R.; Donnino, M.W.; Ferrer, J.M.E.; et al. Part 1: Executive summary: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2015, 132, S315–S367. [Google Scholar] [CrossRef] [PubMed]
- Monsieurs, K.G.; Nolan, J.P.; Bossaert, L.L.; Greif, R.; Maconochie, I.K.; Nikolaou, N.I.; Perkins, G.D.; Soar, J.; Truhlář, A.; Wyllie, J.; et al. European resuscitation council guidelines for resuscitation 2015 Section 1. Executive summary. Resuscitation 2015, 95, 1–80. [Google Scholar] [CrossRef] [PubMed]
- Gruber, J.; Stumpf, D.; Zapletal, B.; Neuhold, S.; Fischer, H. Real-time feedback systems in CPR. Trends Anaesth. Crit. Care 2012, 2, 287–294. [Google Scholar] [CrossRef]
- Yeung, J.; Meeks, R.; Edelson, D.; Gao, F.; Soar, J.; Perkins, G.D. The use of CPR feedback/prompt devices during training and CPR performance: A systematic review. Resuscitation 2009, 80, 743–751. [Google Scholar] [CrossRef] [PubMed]
- Pozner, C.N.; Almozlino, A.; Elmer, J.; Poole, S.; McNamara, D.; Barash, D. Cardiopulmonary resuscitation feedback improves the quality of chest compression provided by hospital health care professionals. Am. J. Emerg. Med. 2011, 29, 618–625. [Google Scholar] [CrossRef]
- Skorning, M.H.; Beckers, S.K.; Brokmann, J.C.; Rörtgen, D.C.; Bergrath, S.; Veiser, T.; Heussen, N.; Rossaint, R. New visual feedback device improves performance of chest compressions by professionals in simulated cardiac arrest. Resuscitation 2010, 81, 53–58. [Google Scholar] [CrossRef]
- American Heart Association. Highlights of the 2015 American Heart Association guidelines Update for CPR and ECC; American Heart Association: Dallas, TX, USA, 2015. [Google Scholar]
- Park, C.; Kang, I.; Heo, S.; Chae, Y.; Kim, H.; Park, S.; Lee, M.; Jeong, W. A Randomised, Cross over Study Using a Mannequin Model to Evaluate the Effects on CPR Quality of Real-Time Audio-Visual Feedback Provided by a Smartphone Application. Hong Kong J. Emerg. Med. 2014, 21, 153–160. [Google Scholar] [CrossRef]
- Sakai, T.; Kitamura, T.; Nishiyama, C.; Murakami, Y.; Ando, M.; Kawamura, T.; Tasaki, O.; Kuwagata, Y.; Shimazu, T.; Iwami, T. Cardiopulmonary Resuscitation Support Application on a Smartphone—Randomized Controlled Trial. Circ. J. 2015, 79, 1052–1057. [Google Scholar] [CrossRef]
- Song, Y.; Oh, J.; Chee, Y. A New Chest Compression Depth Feedback Algorithm for High-Quality CPR Based on Smartphone. Telemed. E-Health 2015, 21, 36–41. [Google Scholar] [CrossRef]
- Song, Y.; Chee, Y.; Oh, J.; Ahn, C.; Lim, T.H. Smartwatches as chest compression feedback devices: A feasibility study. Resuscitation 2016, 103, 20–23. [Google Scholar] [CrossRef]
- Lu, T.C.; Chang, Y.T.; Ho, T.W.; Chen, Y.; Lee, Y.-T.; Wang, Y.-S.; Chen, Y.-P.; Tsai, C.-L.; Ma, M.H.-M.; Fang, C.-C.; et al. Using a smartwatch with real-time feedback improves the delivery of high-quality cardiopulmonary resuscitation by healthcare professionals. Resuscitation 2019, 140, 16–22. [Google Scholar] [CrossRef] [PubMed]
- An, M.; Kim, Y.; Cho, W.-K. Effect of smart devices on the quality of CPR training: A systematic review. Resuscitation 2019, 144, 145–156. [Google Scholar] [CrossRef] [PubMed]
- Dellimore, K.; Heunis, S.; Gohier, F.; Archer, E.; De Villiers, A.; Smith, J.; Scheffer, C. Development of a diagnostic glove for unobtrusive measurement of chest compression force and depth during neonatal CPR. In Proceedings of the 2013 35th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC) IEEE, Osaka, Japan, 3–7 July 2013; Volume 2013, pp. 350–353. [Google Scholar]
- Lee, J.; Song, Y.; Oh, J.; Chee, Y.; Ahn, C.; Shin, H.; Kang, H.; Lim, T.H. Smartwatch feedback device for high-quality chest compressions by a single rescuer during infant cardiac arrest: A randomized, controlled simulation study. Eur. J. Emerg. Med. 2019, 26, 266. [Google Scholar] [CrossRef] [PubMed]
- Madgwick, S.O.H.; Andrew, J.L.H.; Ravi, V. Estimation of IMU and MARG orientation using a gradient descent algorithm. In Proceedings of the 2011 IEEE International Conference on rehAbilitation Robotics, Zurich, Switzerland, 29 June–1 July 2011. [Google Scholar]
- González-Otero, D.M.; De Gauna, S.R.; Ruiz, J.M.; Gutiérrez, J.J.; Saiz, P.; Leturiondo, M. Audiovisual Feedback Devices for Chest Compression Quality during CPR. Resusc. Asp. 2017, 77–96. [Google Scholar] [CrossRef][Green Version]
- Smereka, J.; Szarpak, L.; Smereka, A.; Leung, S.; Ruetzler, K. Evaluation of new two-thumb chest compression technique for infant CPR performed by novice physicians. A randomized, crossover, manikin trial. Am. J. Emerg. Med. 2017, 35, 604–609. [Google Scholar] [CrossRef]
- Lee, J.E.; Lee, J.; Oh, J.; Park, C.H.; Kang, H.; Lim, T.H.; Yoo, K.H. Comparison of two-thumb encircling and two-finger technique during infant cardiopulmonary resuscitation with single rescuer in simulation studies: A systematic review and meta-analysis. Medicine 2019, 98, 45. [Google Scholar] [CrossRef]
- Alvarez, J.C.; Álvarez, D.; López, A.M. Accelerometry-based distance estimation for ambulatory human motion analysis. Sensors 2018, 18, 4441. [Google Scholar] [CrossRef]
- Park, J.; Lim, T.; Lee, Y.; Kim, W.; Cho, Y.; Kang, H. Assessment of chest compression depth obtained using the PocketCPR as an educational tool according to smartphone attachment site. Am. J. Emerg. Med. 2016, 34, 2243–2246. [Google Scholar] [CrossRef]
- Perkins, G.D.; Kocierz, L.; Smith, S.C.; McCulloch, R.A.; Davies, R.P. Compression feed-back devices over estimate chest compression depth when performed on a bed. Resuscitation 2009, 80, 79–82. [Google Scholar] [CrossRef]
- Nishisaki, A.; Maltese, M.R.; Niles, D.E.; Sutton, R.M.; Urbano, J.; Berg, R.A.; Nadkarni, V.M. Backboards are important when chest compressions are provided on a soft mattress. Resuscitation 2012, 83, 1013–1020. [Google Scholar] [CrossRef]
- Handley, A.J. In-hospital chest compressions—The patient on a bed. Resuscitation 2012, 83, 795–796. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Oh, J.; Kang, H.; Lim, T.; Kim, W.; Chee, Y.; Song, Y.; Ahn, C.; Cho, J.H. Proper target depth of an accelerometer-based feedback device during CPR performed on a hospital bed: A randomized simulation study. Am. J. Emerg. Med. 2015, 33, 1425–1429. [Google Scholar] [CrossRef] [PubMed]
- Oh, J.; Song, Y.; Kang, B.; Kang, H.; Lim, T.; Suh, Y.; Chee, Y. The use of dual accelerometers improves measurement of chest compression depth. Resuscitation 2012, 83, 500–504. [Google Scholar] [CrossRef] [PubMed]
- Cheng, A.; Brown, L.L.; Duff, J.P.; Davidson, J.; Overly, F.; Tofil, N.M.; Peterson, D.T.; White, M.L.; Bhanji, F.; Bank, I.; et al. Improving cardiopulmonary resuscitation with a CPR feedback device and refresher simulations (CPR CARES Study): A randomized clinical trial. JAMA Pediatrics 2015, 169, 137–144. [Google Scholar] [CrossRef]
- Krasteva, V.; Jekova, I.; Didon, J.-P. An audiovisual feedback device for compression depth, rate and complete chest recoil can improve the CPR performance of lay persons during self-training on a manikin. Physiol. Meas. 2011, 32, 687–699. [Google Scholar] [CrossRef]
- Wutzler, A.; Bannehr, M.; Von Ulmenstein, S.; Loehr, L.; Förster, J.; Kühnle, Y.; Finn, A.; Storm, C.; Haverkamp, W. Performance of chest compressions with the use of a new audio-visual feedback device: A randomized manikin study in health care professionals. Resuscitation 2015, 87, 81–85. [Google Scholar] [CrossRef]
- Lin, C.-Y.; Hsia, S.-H.; Lee, E.-P.; Chan, O.-W.; Lin, J.-J.; Wu, H.-P. Effect of Audiovisual Cardiopulmonary Resuscitation Feedback Device on Improving Chest Compression Quality. Sci. Rep. 2020, 10, 1–7. [Google Scholar] [CrossRef]
- Kirkbright, S.; Finn, J.; Tohira, H.; Bremner, A.; Jacobs, I.; Celenza, A. Audiovisual feedback device use by health care professionals during CPR: A systematic review and meta-analysis of randomised and non-randomised trials. Resuscitation 2014, 85, 460–471. [Google Scholar] [CrossRef]
- González-Otero, D.M.; De Gauna, S.R.; Ruiz, J.; Chicote, B.; Plaza, S. Feasibility of compression depth estimation from the acceleration signal during cardiopulmonary resuscitation in long-distance trains. In Proceedings of the 2015 Computing in Cardiology Conference (CinC), Nice, France, 6–9 September 2015; pp. 533–536. [Google Scholar]
- Chung, T.N.; Kim, S.W.; You, J.S.; Cho, Y.S.; Chung, S.P.; Park, I.; Kim, S.H. The Specific Effect of Metronome Guidance on the Quality of One-person Cardiopulmonary Resuscitation and Rescuer Fatigue. J. Emerg. Med. 2012, 43, 1049–1054. [Google Scholar] [CrossRef]
- You, J.S.; Chung, S.P.; Chang, C.H.; Park, I.; Lee, H.S.; Kim, S.; Lee, H.S. Effects of flashlight guidance on chest compression performance in cardiopulmonary resuscitation in a noisy environment. Emerg. Med. J. 2012, 30, 628–632. [Google Scholar] [CrossRef]








| Absolute Errors of Compression Depth (mm) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| 21–30 mm | 31–40 mm | 41–50 mm | 51–60 mm | ||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||
| Proposed Algorithm | 2.41 | 0.95 | 1.99 | 1.12 | 1.92 | 1.12 | 1.99 | 1.10 | |
| Song et al. Algorithm | 2.59 | 0.96 | 2.14 | 1.15 | 2.10 | 1.17 | 2.08 | 1.11 | |
| Absolute Error (mm) | ||||||
|---|---|---|---|---|---|---|
| Situation #1 | Situation #2 | Situation #3 | ||||
| Mean | SD | Mean | SD | Mean | SD | |
| Proposed Algorithm | 1.99 | 1.10 | 2.19 | 0.88 | 1.36 | 1.09 |
| Song et al. Algorithm | 2.08 | 1.11 | 2.32 | 0.89 | 2.03 | 1.41 |
| Absolute Error between Either the Smart Ring or Smartwatch and the Mannequin LVDT (mm) | ||||||
|---|---|---|---|---|---|---|
| Adult Mannequin | Infant Mannequin (Two Finger) | Infant Mannequin (Two Thumb) | ||||
| Mean | SD | Mean | SD | Mean | SD | |
| |Mannequin LVDT—Ring| | 3.1 | 1.9 | 7.6 | 2.4 | 2.9 | 1.8 |
| |Mannequin LVDT—Watch| | 11.8 | 4.2 | 10.7 | 3.5 | 7.7 | 5.3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, S.; Song, Y.; Lee, J.; Oh, J.; Lim, T.H.; Ahn, C.; Kim, I.Y. Development of Smart-Ring-Based Chest Compression Depth Feedback Device for High Quality Chest Compressions: A Proof-of-Concept Study. Biosensors 2021, 11, 35. https://doi.org/10.3390/bios11020035
Lee S, Song Y, Lee J, Oh J, Lim TH, Ahn C, Kim IY. Development of Smart-Ring-Based Chest Compression Depth Feedback Device for High Quality Chest Compressions: A Proof-of-Concept Study. Biosensors. 2021; 11(2):35. https://doi.org/10.3390/bios11020035
Chicago/Turabian StyleLee, Seungjae, Yeongtak Song, Jongshill Lee, Jaehoon Oh, Tae Ho Lim, Chiwon Ahn, and In Young Kim. 2021. "Development of Smart-Ring-Based Chest Compression Depth Feedback Device for High Quality Chest Compressions: A Proof-of-Concept Study" Biosensors 11, no. 2: 35. https://doi.org/10.3390/bios11020035
APA StyleLee, S., Song, Y., Lee, J., Oh, J., Lim, T. H., Ahn, C., & Kim, I. Y. (2021). Development of Smart-Ring-Based Chest Compression Depth Feedback Device for High Quality Chest Compressions: A Proof-of-Concept Study. Biosensors, 11(2), 35. https://doi.org/10.3390/bios11020035








