The NADPH Oxidase Isoform 1 Contributes to Angiotensin II-Mediated DNA Damage in the Kidney
Abstract
:1. Introduction
2. Materials and Methods
2.1. Animals and Animal Treatment
2.1.1. Part 1: Nox1 Knockout Mice
2.1.2. Part 2: Nox2 Knockout Mice
2.1.3. Parts 3 and 4: Nox4 Knockout Mice
2.2. Renal Function
2.3. Histopathology
2.4. Measurement of ROS Formation
2.5. Isolation of Primary Kidney Cells for DNA Strand Break Detection via Comet Assay
2.6. Immunohistochemistry
2.7. Statistics
3. Results
3.1. Animal Characteristics and Blood Pressure Changes
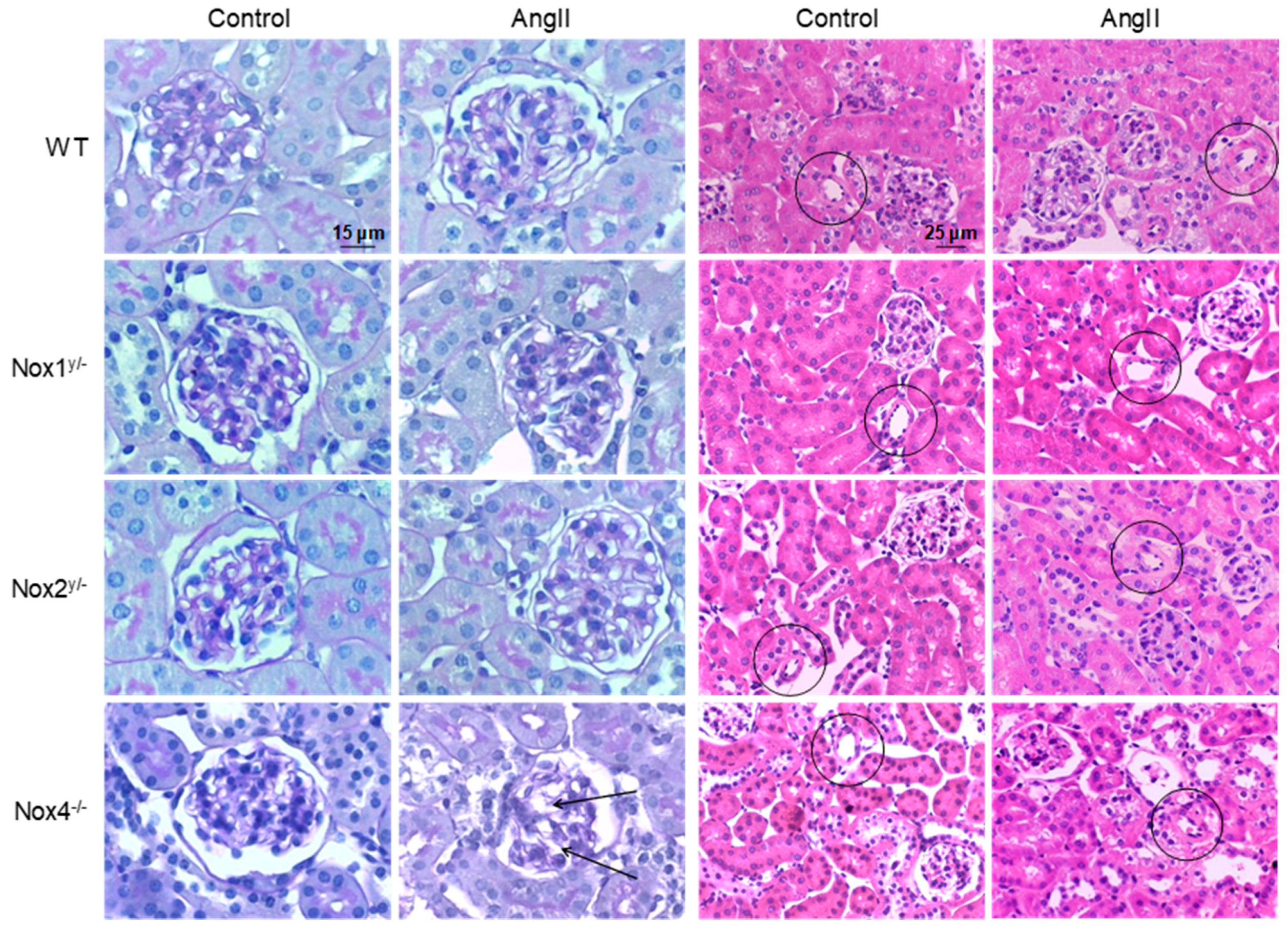
3.2. Renal Function and Morphology
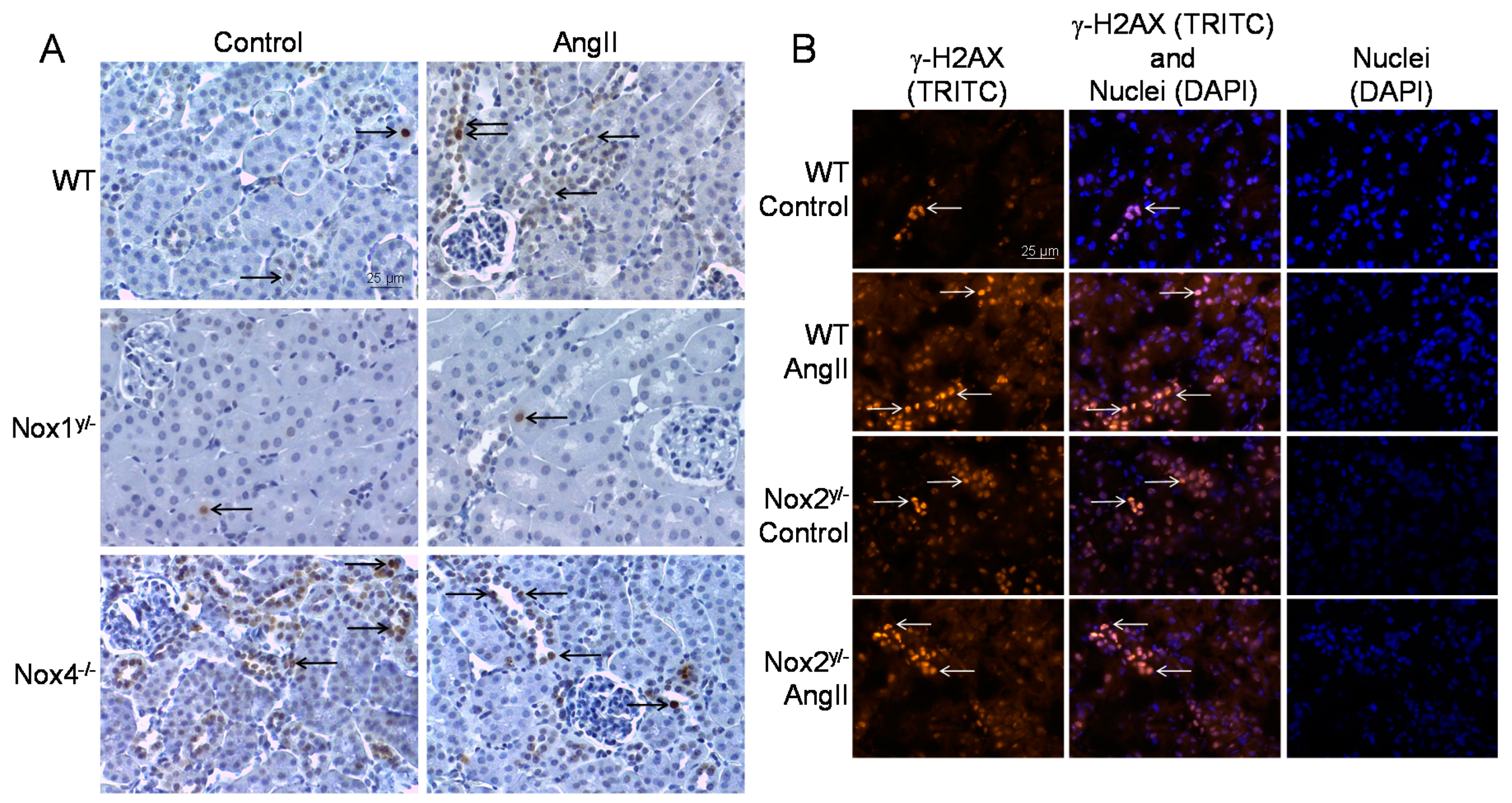
3.3. Markers of Oxidative Stress and DNA Damage
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Colt, J.S.; Schwartz, K.; Graubard, B.I.; Davis, F.; Ruterbusch, J.; DiGaetano, R.; Purdue, M.; Rothman, N.; Wacholder, S.; Chow, W.H. Hypertension and risk of renal cell carcinoma among white and black Americans. Epidemiology 2011, 22, 797–804. [Google Scholar] [CrossRef] [Green Version]
- Flaherty, K.T.; Fuchs, C.S.; Colditz, G.A.; Stampfer, M.J.; Speizer, F.E.; Willett, W.C.; Curhan, G.C. A prospective study of body mass index, hypertension, and smoking and the risk of renal cell carcinoma (United States). Cancer Causes Control 2005, 16, 1099–1106. [Google Scholar] [CrossRef]
- Hsieh, J.J.; Purdue, M.P.; Signoretti, S.; Swanton, C.; Albiges, L.; Schmidinger, M.; Heng, D.Y.; Larkin, J.; Ficarra, V. Renal cell carcinoma. Nat. Rev. Dis. Primers 2017, 3, 17009. [Google Scholar] [CrossRef]
- Laragh, J.H.; Lewis, K. Dahl Memorial Lecture. The renin system and four lines fo hypertension research. Nephron heterogeneity, the calcium connection, the prorenin vasodilator limb, and plasma renin and heart attack. Hypertension 1992, 20, 267–279. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deckers, I.A.; van den Brandt, P.A.; van Engeland, M.; van Schooten, F.J.; Godschalk, R.W.; Keszei, A.P.; Schouten, L.J. Polymorphisms in genes of the renin-angiotensin-aldosterone system and renal cell cancer risk: Interplay with hypertension and intakes of sodium, potassium and fluid. Int. J. Cancer 2015, 136, 1104–1116. [Google Scholar] [CrossRef] [PubMed]
- Schupp, N.; Schmid, U.; Rutkowski, P.; Lakner, U.; Kanase, N.; Heidland, A.; Stopper, H. Angiotensin II-induced genomic damage in renal cells can be prevented by angiotensin II type 1 receptor blockage or radical scavenging. Am. J. Physiol. Renal Physiol. 2007, 292, F1427–F1434. [Google Scholar] [CrossRef] [Green Version]
- Schmid, U.; Stopper, H.; Schweda, F.; Queisser, N.; Schupp, N. Angiotensin II induces DNA damage in the kidney. Cancer Res. 2008, 68, 9239–9246. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brand, S.; Amann, K.; Schupp, N. Angiotensin II-induced hypertension dose-dependently leads to oxidative stress and DNA damage in mouse kidneys and hearts. J. Hypertens. 2013, 31, 333–344. [Google Scholar] [CrossRef]
- Hartmann, C.; Schulz, I.; Epe, B.; Schupp, N. Angiotensin II-induced hypertension increases the mutant frequency in rat kidney. Arch. Toxicol. 2019, 93, 2045–2055. [Google Scholar] [CrossRef]
- Fazeli, G.; Stopper, H.; Schinzel, R.; Ni, C.W.; Jo, H.; Schupp, N. Angiotensin II induces DNA damage via AT1 receptor and NADPH oxidase isoform Nox4. Mutagenesis 2012, 27, 673–681. [Google Scholar] [CrossRef]
- Brand, S.; Amann, K.; Mandel, P.; Zimnol, A.; Schupp, N. Oxidative DNA damage in kidneys and heart of hypertensive mice is prevented by blocking angiotensin II and aldosterone receptors. PLoS ONE 2014, 9, e115715. [Google Scholar] [CrossRef] [PubMed]
- Garrido, A.M.; Griendling, K.K. NADPH oxidases and angiotensin II receptor signaling. Mol. Cell Endocrinol. 2009, 302, 148–158. [Google Scholar] [CrossRef] [Green Version]
- Santillo, M.; Colantuoni, A.; Mondola, P.; Guida, B.; Damiano, S. NOX signaling in molecular cardiovascular mechanisms involved in the blood pressure homeostasis. Front. Physiol. 2015, 6, 194. [Google Scholar] [CrossRef] [PubMed]
- Bedard, K.; Krause, K.H. The NOX family of ROS-generating NADPH oxidases: Physiology and pathophysiology. Physiol. Rev. 2007, 87, 245–313. [Google Scholar] [CrossRef] [PubMed]
- Gill, P.S.; Wilcox, C.S. NADPH oxidases in the kidney. Antioxid. Redox Signal. 2006, 8, 1597–1607. [Google Scholar] [CrossRef] [PubMed]
- Tu, H.; Wen, C.P.; Tsai, S.P.; Chow, W.H.; Wen, C.; Ye, Y.; Zhao, H.; Tsai, M.K.; Huang, M.; Dinney, C.P.; et al. Cancer risk associated with chronic diseases and disease markers: Prospective cohort study. BMJ 2018, 360, k134. [Google Scholar] [CrossRef] [Green Version]
- Zimnol, A.; Amann, K.; Mandel, P.; Hartmann, C.; Schupp, N. Angiotensin II type 1a receptor-deficient mice develop angiotensin II-induced oxidative stress and DNA damage without blood pressure increase. Am. J. Physiol. Renal Physiol. 2017, 313, F1264–F1273. [Google Scholar] [CrossRef]
- Westhoff, J.H.; Hilgers, K.F.; Steinbach, M.P.; Hartner, A.; Klanke, B.; Amann, K.; Melk, A. Hypertension induces somatic cellular senescence in rats and humans by induction of cell cycle inhibitor p16INK4a. Hypertension 2008, 52, 123–129. [Google Scholar] [CrossRef] [Green Version]
- Schupp, N.; Kolkhof, P.; Queisser, N.; Gärtner, S.; Schmid, U.; Kretschmer, A.; Hartmann, E.; Oli, R.G.; Schäfer, S.; Stopper, H. Mineralocorticoid receptor-mediated DNA damage in kidneys of DOCA-salt hypertensive rats. FASEB J. 2011, 25, 968–978. [Google Scholar] [CrossRef]
- Lamprecht, M.R.; Sabatini, D.M.; Carpenter, A.E. CellProfiler: Free, versatile software for automated biological image analysis. Biotechniques 2007, 42, 71–75. [Google Scholar] [CrossRef] [Green Version]
- Yogi, A.; Mercure, C.; Touyz, J.; Callera, G.E.; Montezano, A.C.; Aranha, A.B.; Tostes, R.C.; Reudelhuber, T.; Touyz, R.M. Renal redox-sensitive signaling, but not blood pressure, is attenuated by Nox1 knockout in angiotensin II-dependent chronic hypertension. Hypertension 2008, 51, 500–506. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chrissobolis, S.; Banfi, B.; Sobey, C.G.; Faraci, F.M. Role of Nox isoforms in angiotensin II-induced oxidative stress and endothelial dysfunction in brain. J. Appl. Physiol. 2012, 113, 184–191. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johar, S.; Cave, A.C.; Narayanapanicker, A.; Grieve, D.J.; Shah, A.M. Aldosterone mediates angiotensin II-induced interstitial cardiac fibrosis via a Nox2-containing NADPH oxidase. FASEB J. 2006, 20, 1546–1548. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schroder, K.; Zhang, M.; Benkhoff, S.; Mieth, A.; Pliquett, R.; Kosowski, J.; Kruse, C.; Luedike, P.; Michaelis, U.R.; Weissmann, N.; et al. Nox4 is a protective reactive oxygen species generating vascular NADPH oxidase. Circ. Res. 2012, 110, 1217–1225. [Google Scholar] [CrossRef] [Green Version]
- Matsuno, K.; Yamada, H.; Iwata, K.; Jin, D.; Katsuyama, M.; Matsuki, M.; Takai, S.; Yamanishi, K.; Miyazaki, M.; Matsubara, H.; et al. Nox1 is involved in angiotensin II-mediated hypertension: A study in Nox1-deficient mice. Circulation 2005, 112, 2677–2685. [Google Scholar] [CrossRef]
- Byrne, J.A.; Grieve, D.J.; Bendall, J.K.; Li, J.M.; Gove, C.; Lambeth, J.D.; Cave, A.C.; Shah, A.M. Contrasting roles of NADPH oxidase isoforms in pressure-overload versus angiotensin II-induced cardiac hypertrophy. Circ. Res. 2003, 93, 802–805. [Google Scholar] [CrossRef]
- Bouabout, G.; Ayme-Dietrich, E.; Jacob, H.; Champy, M.F.; Birling, M.C.; Pavlovic, G.; Madeira, L.; Fertak, L.E.; Petit-Demouliere, B.; Sorg, T.; et al. Nox4 genetic inhibition in experimental hypertension and metabolic syndrome. Arch. Cardiovasc. Dis. 2018, 111, 41–52. [Google Scholar] [CrossRef]
- Miyano, K.; Sumimoto, H. Role of the small GTPase Rac in p22phox-dependent NADPH oxidases. Biochimie 2007, 89, 1133–1144. [Google Scholar] [CrossRef]
- Zimmerman, M.C.; Dunlay, R.P.; Lazartigues, E.; Zhang, Y.; Sharma, R.V.; Engelhardt, J.F.; Davisson, R.L. Requirement for Rac1-dependent NADPH oxidase in the cardiovascular and dipsogenic actions of angiotensin II in the brain. Circ. Res. 2004, 95, 532–539. [Google Scholar] [CrossRef] [Green Version]
- Peterson, J.R.; Burmeister, M.A.; Tian, X.; Zhou, Y.; Guruju, M.R.; Stupinski, J.A.; Sharma, R.V.; Davisson, R.L. Genetic silencing of Nox2 and Nox4 reveals differential roles of these NADPH oxidase homologues in the vasopressor and dipsogenic effects of brain angiotensin II. Hypertension 2009, 54, 1106–1114. [Google Scholar] [CrossRef] [Green Version]
- Zhu, K.; Kakehi, T.; Matsumoto, M.; Iwata, K.; Ibi, M.; Ohshima, Y.; Zhang, J.; Liu, J.; Wen, X.; Taye, A.; et al. NADPH oxidase NOX1 is involved in activation of protein kinase C and premature senescence in early stage diabetic kidney. Free Radic. Biol. Med. 2015, 83, 21–30. [Google Scholar] [CrossRef] [PubMed]
- You, Y.H.; Okada, S.; Ly, S.; Jandeleit-Dahm, K.; Barit, D.; Namikoshi, T.; Sharma, K. Role of Nox2 in diabetic kidney disease. Am. J. Physiol. Renal Physiol. 2013, 304, F840–F848. [Google Scholar] [CrossRef] [PubMed]
- Babelova, A.; Avaniadi, D.; Jung, O.; Fork, C.; Beckmann, J.; Kosowski, J.; Weissmann, N.; Anilkumar, N.; Shah, A.M.; Schaefer, L.; et al. Role of Nox4 in murine models of kidney disease. Free Radic. Biol. Med. 2012, 53, 842–853. [Google Scholar] [CrossRef]
- Jha, J.C.; Gray, S.P.; Barit, D.; Okabe, J.; El-Osta, A.; Namikoshi, T.; Thallas-Bonke, V.; Wingler, K.; Szyndralewiez, C.; Heitz, F.; et al. Genetic targeting or pharmacologic inhibition of NADPH oxidase nox4 provides renoprotection in long-term diabetic nephropathy. J. Am. Soc. Nephrol. 2014, 25, 1237–1254. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nwabuo, C.C.; Vasan, R.S. Pathophysiology of Hypertensive Heart Disease: Beyond Left Ventricular Hypertrophy. Curr. Hypertens. Rep. 2020, 22, 11. [Google Scholar] [CrossRef] [PubMed]
- Di Marco, E.; Gray, S.P.; Chew, P.; Kennedy, K.; Cooper, M.E.; Schmidt, H.H.; Jandeleit-Dahm, K.A. Differential effects of NOX4 and NOX1 on immune cell-mediated inflammation in the aortic sinus of diabetic ApoE-/-mice. Clin. Sci. 2016, 130, 1363–1374. [Google Scholar] [CrossRef]
- Sobey, C.G.; Judkins, C.P.; Rivera, J.; Lewis, C.V.; Diep, H.; Lee, H.W.; Kemp-Harper, B.K.; Broughton, B.R.; Selemidis, S.; Gaspari, T.A.; et al. NOX1 deficiency in apolipoprotein E-knockout mice is associated with elevated plasma lipids and enhanced atherosclerosis. Free Radic. Res. 2015, 49, 186–198. [Google Scholar] [CrossRef]
- Gray, S.P.; Di Marco, E.; Kennedy, K.; Chew, P.; Okabe, J.; El-Osta, A.; Calkin, A.C.; Biessen, E.A.; Touyz, R.M.; Cooper, M.E.; et al. Reactive Oxygen Species Can Provide Atheroprotection via NOX4-Dependent Inhibition of Inflammation and Vascular Remodeling. Arterioscler. Thromb. Vasc. Biol. 2016, 36, 295–307. [Google Scholar] [CrossRef] [Green Version]
- Lan, T.; Kisseleva, T.; Brenner, D.A. Deficiency of NOX1 or NOX4 Prevents Liver Inflammation and Fibrosis in Mice through Inhibition of Hepatic Stellate Cell Activation. PLoS ONE 2015, 10, e0129743. [Google Scholar] [CrossRef]
- Helfinger, V.V.G.F.; Henke, N.; Kunze, M.M.; Schmid, T.; Heidler, J.; Wittig, I.; Radeke, H.H.; Marschall, V.; Anderson, K. Hydrogen peroxide formation by Nox4 limits malignant transformation. bioRxiv 2017. [Google Scholar] [CrossRef] [Green Version]
- Kodama, R.; Kato, M.; Furuta, S.; Ueno, S.; Zhang, Y.; Matsuno, K.; Yabe-Nishimura, C.; Tanaka, E.; Kamata, T. ROS-generating oxidases Nox1 and Nox4 contribute to oncogenic Ras-induced premature senescence. Genes Cells 2013, 18, 32–41. [Google Scholar] [CrossRef] [PubMed]
- Stalin, J.; Garrido-Urbani, S.; Heitz, F.; Szyndralewiez, C.; Jemelin, S.; Coquoz, O.; Ruegg, C.; Imhof, B.A. Inhibition of host NOX1 blocks tumor growth and enhances checkpoint inhibitor-based immunotherapy. Life Sci. Alliance 2019, 2, e201800265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liang, S.; Ma, H.Y.; Zhong, Z.; Dhar, D.; Liu, X.; Xu, J.; Koyama, Y.; Nishio, T.; Karin, D.; Karin, G.; et al. NADPH Oxidase 1 in Liver Macrophages Promotes Inflammation and Tumor Development in Mice. Gastroenterology 2019, 156, 1156–1172.e1156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ha, S.Y.; Paik, Y.H.; Yang, J.W.; Lee, M.J.; Bae, H.; Park, C.K. NADPH Oxidase 1 and NADPH Oxidase 4 Have Opposite Prognostic Effects for Patients with Hepatocellular Carcinoma after Hepatectomy. Gut Liver 2016, 10, 826–835. [Google Scholar] [CrossRef] [PubMed] [Green Version]
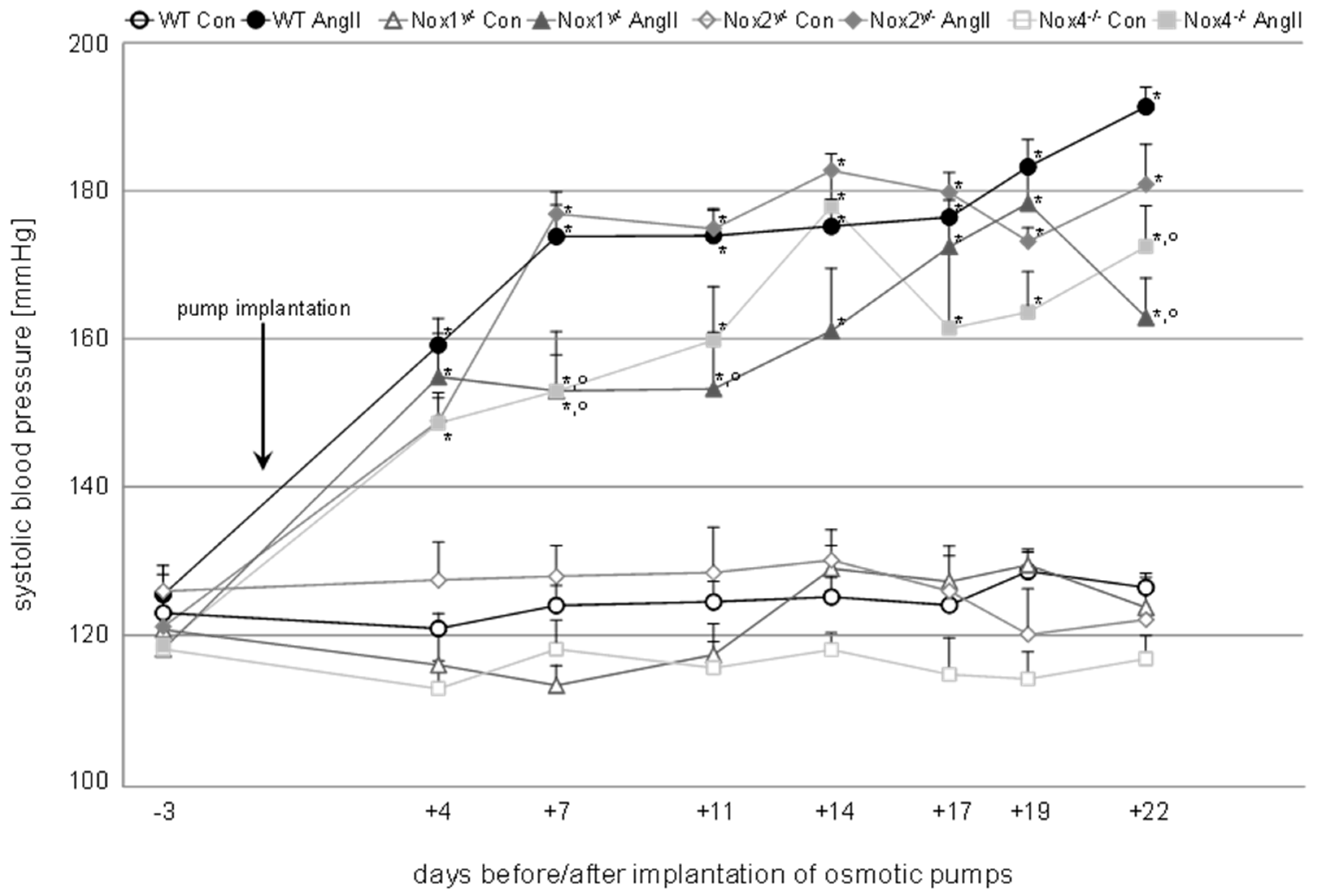



| Body Weight (g) | Relative Kidney Weight (‰) | Relative Heart Weight (‰) | Systolic Blood Pressure (mmHg) | Diastolic Blood Pressure (mmHg) | ||
|---|---|---|---|---|---|---|
| Wildtype | Control | 30.6 ± 0.3 | 6.4 ± 0.2 | 6.3 ± 0.2 | 127 ± 2 | 83 ± 3 |
| AngII | 28.1 ± 0.3 *** | 6.6 ± 0.2 | 7.9 ± 0.3 *** | 194 ± 3 *** | 121 ± 4 *** | |
| Nox1y/− | Control | 28.3 ± 0.6 ++ | 6.0 ±.0.2 | 6.3 ± 0.2 | 124 ± 2 | 84 ± 4 |
| AngII | 27.9 ± 0.8 | 6.0 ± 0.1 | 7.3 ± 0.4 * | 163 ± 5 ***,°°° | 103 ± 9 | |
| Nox2y/− | Control | 33.3 ± 0.9 +++ | 6.2 ± 0.2 | 5.6 ± 0.2 | 123 ± 5 | 78 ± 9 |
| AngII | 28.6 ± 0.6 *** | 6.3 ± 0.2 | 7.2 ± 0.4 ** | 181 ± 6 *** | 129 ± 8 *** | |
| Nox4−/− | Control | 31.1 ± 0.5 | 6.1 ± 0.2 | 6.5 ± 0.4 | 115 ± 4 | 70 ± 4 |
| AngII | 27.7 ± 0.6 *** | 6.0 ± 0.2 | 7.0 ± 0.5 | 170 ± 7 ***,°°° | 118 ± 5 *** |
| Drink Volume [mL] | Creatinine Clearance [µL/min] | GSI | MSI | TSI | VSI | ||
|---|---|---|---|---|---|---|---|
| Wildtype | Control | 3.9 ± 0.3 | 73 ± 9 | 1.1 ± 0.1 | 1.0 ± 0.2 | 0.1 ± 0.2 | 0.7 ± 0.1 |
| AngII | 7.1 ± 0.5 *** | 74 ± 13 | 1.3 ± 0.1 | 1.1 ± 0.2 | 0.1 ± 0.1 | 1.1 ± 0.1 *** | |
| Nox1y/− | Control | 4.4 ± 0.7 | 94 ± 11 | 1.2 ± 0.1 | 0.3 ± 0.1 + | 0.1 ± 0.0 | 0.6 ± 0.1 |
| AngII | 4.5 ± 1.1 | 81 ± 8 | 1.4 ± 0.2 | 0.4 ± 0.1 | 0.1 ± 0.1 | 0.8 ± 0.1 ° | |
| Nox2y/− | Control | 3.5 ± 0.2 | 105 ± 22 | 1.2 ± 0.1 | 0.8 ± 0.1 | 0.3 ± 0.0 | 0.9 ± 0.1 |
| AngII | 7.6 ± 0.8 *** | 77 ± 7 | 1.0 ± 0.1 | 0.6 ± 0.0 | 0.2 ± 0.0 | 1.3 ± 0.1 * | |
| Nox4−/− | Control | 3.8 ± 0.4 | 53 ± 11 | 1.3 ± 0.1 | 1.2 ± 0.1 | 0.1 ± 0.0 | 0.8 ± 0.1 |
| AngII | 7.4 ± 0.9 ** | 52 ± 5 | 1.2 ± 0.0 | 1.5 ± 0.1 ** | 0.1 ± 0.0 | 1.1 ± 0.1 * |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zimnol, A.; Spicker, N.; Balhorn, R.; Schröder, K.; Schupp, N. The NADPH Oxidase Isoform 1 Contributes to Angiotensin II-Mediated DNA Damage in the Kidney. Antioxidants 2020, 9, 586. https://doi.org/10.3390/antiox9070586
Zimnol A, Spicker N, Balhorn R, Schröder K, Schupp N. The NADPH Oxidase Isoform 1 Contributes to Angiotensin II-Mediated DNA Damage in the Kidney. Antioxidants. 2020; 9(7):586. https://doi.org/10.3390/antiox9070586
Chicago/Turabian StyleZimnol, Anna, Nora Spicker, Ronja Balhorn, Katrin Schröder, and Nicole Schupp. 2020. "The NADPH Oxidase Isoform 1 Contributes to Angiotensin II-Mediated DNA Damage in the Kidney" Antioxidants 9, no. 7: 586. https://doi.org/10.3390/antiox9070586






