Finite Element Analysis and Validation of Segments C2-C7 of the Cervical Spine
Abstract
:1. Introduction
2. Materials and Methods
2.1. Finite Element Model Establishment
2.2. Load and Boundary Conditions
3. Results
3.1. Range of Motion
3.2. Intervertebral Disc Stress
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Panjabi, M.; Crisco, J.J.; Vasavada, A.; Oda, T.; Cholewicki, J.; Nibu, K.; Shin, E. Mechanical properties of the human cervical spine as shown by three-dimensional load-displacement curves. Spine 2001, 26, 2692–2700. [Google Scholar] [CrossRef]
- Nightingale, R.W.; Winkelstein, B.A.; Knaub, K.E.; Richardson, W.J.; Luck, J.F.; Myers, B.S. Comparative strengths and structural properties of the upper and lower cervical spine in flexion and extension. J. Biomech. 2002, 35, 725–732. [Google Scholar] [CrossRef]
- Wheeldon, J.A.; Pintar, F.A.; Knowles, S.; Yoganandan, N. Experimental flexion/extension data corridors for validation of finite element models of the young, normal cervical spine. J. Biomech. 2006, 39, 375–380. [Google Scholar] [CrossRef]
- Nightingale, R.W.; Carol Chancey, V.; Ottaviano, D.; Luck, J.F.; Tran, L.; Prange, M.; Myers, B.S. Flexion and extension structural properties and strengths for male cervical spine segments. J. Biomech. 2007, 40, 535–542. [Google Scholar] [CrossRef]
- Liu, Q.; Guo, Q.; Yang, J.; Zhang, P.; Xu, T.; Cheng, X.; Chen, J.; Guan, H.; Ni, B. Subaxial Cervical Intradiscal Pressure and Segmental Kinematics Following Atlantoaxial Fixation in Different Angles. World Neurosurg. 2016, 87, 521–528. [Google Scholar] [CrossRef]
- Belytschko, T.; Kulak, R.F.; Schultz, A.B.; Galante, J.O. Finite element stress analysis of an intervertebral disc. J. Biomech. 1974, 7, 277. [Google Scholar] [CrossRef]
- Bozic, K.J.; Keyak, J.H.; Skinner, H.B.; Bueff, H.U.; Bradford, D.S. Three-dimensional finite element modeling of a cervical vertebra: An investigation of burst fracture mechanism. J. Spinal Disord. 1994, 7, 102–110. [Google Scholar] [CrossRef]
- Teo, E.C.; Paul, J.P.; Evans, J.H. Finite element stress analysis of a cadaver second cervical vertebra. Med. Biol. Eng. Comput. 1994, 32, 236. [Google Scholar]
- Teo, E.C.; Ng, H.W. Evaluation of the Role of Ligaments, Facets and Disc Nucleus in Lower Cervical Spine Under Compression and Sagittal Moments Using Finite Element Method. Med. Eng. Phys. 2001, 23, 155–164. [Google Scholar] [CrossRef]
- Del Palomar, A.P.; Calvo, B.; Doblaré, M. An Accurate Finite Element Model of the Cervical Spine Under Quasi-Static Loading. J. Biomech. 2008, 41, 523–531. [Google Scholar] [CrossRef]
- Panzer, M.B.; Fice, J.B.; Cronin, D.S. Cervical Spine Response in Frontal Crash. Med. Eng. Phys. 2011, 33, 1147–1159. [Google Scholar] [CrossRef] [PubMed]
- Oxland, T.R. Fundamental Biomechanics of the Spine—What we Have Learned in the Past 25 Years and Future Directions. J. Biomech. 2016, 49, 817–832. [Google Scholar] [CrossRef]
- Kim, Y.H.; Khuyagbaatar, B.; Kim, K. Recent Advances in Finite Element Modeling of the Human Cervical Spine. J. Mech. Sci. Technol. 2018, 32, 1–10. [Google Scholar] [CrossRef]
- DeWit, J.A.; Cronin, D.S. Cervical Spine Segment Finite Element Model for Traumatic Injury Prediction. J. Mech. Behav. Biomed. 2012, 10, 138–150. [Google Scholar] [CrossRef] [PubMed]
- Cronin, D.S. Finite Element Modeling of Potential Cervical Spine Pain Sources in Neutral Position Low Speed Rear Impact. J. Mech. Behav. Biomed. 2014, 33, 55–66. [Google Scholar] [CrossRef] [PubMed]
- Mustafy, T.; Moglo, K.; Adeeb, S.; El-Rich, M. Injury Mechanisms of the Ligamentous Cervical C2-C3 Functional Spinal Unit to Complex Loading Modes: Finite Element Study. J. Mech. Behav. Biomed. 2016, 53, 384–396. [Google Scholar] [CrossRef] [PubMed]
- Meyer, F.; Humm, J.; Purushothaman, Y.; Willinger, R.; Pintar, F.A.; Yoganandan, N. Forces and Moments in Cervical Spinal Column Segments in Frontal Impacts Using Finite Element Modeling and Human Cadaver Tests. J. Mech. Behav. Biomed. 2019, 90, 681–688. [Google Scholar] [CrossRef]
- Zhang, Q.H.; Teo, E.C.; Ng, H.W.; Lee, V.S. Finite Element Analysis of Moment-Rotation Relationships for Human Cervical Spine. J. Biomech. 2006, 39, 189–193. [Google Scholar] [CrossRef]
- Kallemeyn, N.; Gandhi, A.; Kode, S.; Shivanna, K.; Smucker, J.; Grosland, N. Validation of a C2–C7 Cervical Spine Finite Element Model Using Specimen-Specific Flexibility Data. Med. Eng. Phys. 2010, 32, 482–489. [Google Scholar] [CrossRef]
- Erbulut, D.U.; Zafarparandeh, I.; Lazoglu, I.; Ozer, A.F. Application of an Asymmetric Finite Element Model of the C2-T1 Cervical Spine for Evaluating the Role of Soft Tissues in Stability. Med. Eng. Phys. 2014, 36, 915–921. [Google Scholar] [CrossRef] [PubMed]
- Herron, M.R.; Park, J.; Dailey, A.T.; Brockmeyer, D.L.; Ellis, B.J. Febio Finite Element Models of the Human Cervical Spine. J. Biomech. 2020, 113, 110077. [Google Scholar] [CrossRef] [PubMed]
- Hua, W.; Zhi, J.; Ke, W.; Wang, B.; Yang, S.; Li, L.; Yang, C. Adjacent Segment Biomechanical Changes After One- Or Two-Level Anterior Cervical Discectomy and Fusion Using Either a Zero-Profile Device or Cage Plus Plate: A Finite Element Analysis. Comput. Biol. Med. 2020, 120, 103760. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Yuchi, C.X.; Gao, Z.; Ma, X.; Zhao, D.; Li, J.W.; Xu, B.; Zhang, C.Q.; Wang, Z.; Du, C.F.; et al. Comparative Analysis of the Biomechanics of the Adjacent Segments After Minimally Invasive Cervical Surgeries Versus Anterior Cervical Discectomy and Fusion: A Finite Element Study. J. Orthop. Transl. 2020, 23, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Khalaf, K.; Nikkhoo, M. Comparative Biomechanical Analyses of Lower Cervical Spine Post Anterior Fusion Versus Intervertebral Disc Arthroplasty: A Geometrically Patient-Specific Poroelastic Finite Element Investigation. J. Orthop. Transl. 2022, 36, 33–43. [Google Scholar] [CrossRef]
- Nishida, N.; Tripathi, S.; Mumtaz, M.; Kelkar, A.; Kumaran, Y.; Sakai, T.; Goel, V.K. Soft Tissue Injury in Cervical Spine is a Risk Factor for Intersegmental Instability: A Finite Element Analysis. World Neurosurg. 2022, 164, e358–e366. [Google Scholar] [CrossRef]
- Yuan, W.; Zhang, H.; Zhou, X.; Wu, W.; Zhu, Y. The Influence of Artificial Cervical Disc Prosthesis Height on the Cervical Biomechanics: A Finite Element Study. World Neurosurg. 2018, 113, e490–e498. [Google Scholar] [CrossRef]
- Zhou, E.; Huang, H.; Zhao, Y.; Wang, L.; Fan, Y. The Effects of Titanium Mesh Cage Size on the Biomechanical Responses of Cervical Spine After Anterior Cervical Corpectomy and Fusion: A Finite Element Study. Clin. Biomech. 2022, 91, 105547. [Google Scholar] [CrossRef]
- Wang, K.; Wang, H.; Deng, Z.; Li, Z.; Zhan, H.; Niu, W. Cervical Traction Therapy with and without Neck Support: A Finite Element Analysis. Musculoskel. Sci. Prac. 2017, 28, 1–9. [Google Scholar] [CrossRef]
- Schmidt, H.; Heuer, F.; Drumm, J.; Klezl, Z.; Claes, L.; Wilke, H.J. Application of a calibration method provides more realistic results for a finite element model of a lumbar spinal segment. Clin. Biomech. 2007, 22, 377–384. [Google Scholar] [CrossRef]
- Panjabi, M.M. Cervical Spine Models for Biomechanical Research. Spine 1998, 23, 2684. [Google Scholar] [CrossRef]
- Yoganandan, N.; Kumaresan, S.; Pintar, F.A. Geometric and mechanical properties of human cervical spine ligaments. J. Biomech. Eng. 2000, 122, 623. [Google Scholar] [CrossRef] [PubMed]
- Ha, S.K. Finite element modeling of multi-level cervical spinal segments (c3–c6) and biomechanical analysis of an elastomer-type prosthetic disc. Med. Eng. Phys. 2006, 28, 534–541. [Google Scholar] [CrossRef]
- Kumaresan, S.; Yoganandan, N.; Pintar, F.A. Finite element modeling approaches of human cervical spine facet joint capsule. J. Biomech. 1998, 31, 371–376. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Lewis, G. Influence of the constitutive material behavior model assigned to the annulus fibrosus and the nucleus pulposus on the biomechanical performance of a model of the cervical spine: A finite element analysis study. J. Mech. Med. Biol. 2010, 10, 151–166. [Google Scholar] [CrossRef]
- Ezquerro, F.; Vacas, F.G.; Postigo, S.; Prado, M.; Simón, A. Calibration of the finite element model of a lumbar functional spinal unit using an optimization technique based on differential evolution. Med. Eng. Phys. 2011, 33, 89–95. [Google Scholar] [CrossRef]
- Kim, H.; Chun, H.; Lee, H.; Kang, K.; Lee, C.; Chang, B.; Yeom, J.S. The biomechanical influence of the facet joint orientation and the facet tropism in the lumbar spine. Spine J. 2013, 13, 1301–1308. [Google Scholar] [CrossRef] [PubMed]
- Panzer, M.B.; Cronin, D.S. C4–c5 segment finite element model development, validation, and load-sharing investigation. J. Biomech. 2009, 42, 480–490. [Google Scholar] [CrossRef] [PubMed]
- Camacho, D.L.; Nightingale, R.W.; Robinette, J.J.; Vanguri, S.K.; Coates, D.J.; Myers, B.S. (Eds.) Experimental Flexibility Measurements for the Development of a Computational Head-Neck Model Validated for Near-Vertex Head Impact; SAE International: Warrendale, PA, USA, 1997. [Google Scholar]
- Womack, W.; Leahy, P.D.; Patel, V.V.; Puttlitz, C.M. Finite element modeling of kinematic and load transmission alterations due to cervical intervertebral disc replacement. Spine 2011, 36, E1126–E1133. [Google Scholar] [CrossRef] [PubMed]
- Pospiech, J.; Stolke, D.; Wilke, H.J.; Claes, L.E. Intradiscal pressure recordings in the cervical spine. Neurosurgery 1999, 44, 379–385. [Google Scholar] [CrossRef]
- Mattucci, S.F.E.; Moulton, J.A.; Chandrashekar, N.; Cronin, D.S. Strain rate dependent properties of younger human cervical spine ligaments. J. Mech. Behav. Biomed. 2012, 10, 216–226. [Google Scholar] [CrossRef] [Green Version]
- Yoganandan, N.; Knowles, S.A.; Maiman, D.J.; Pintar, F.A. Anatomic Study of the Morphology of Human Cervical Facet Joint. Spine 2003, 28, 2317–2323. [Google Scholar] [CrossRef] [PubMed]
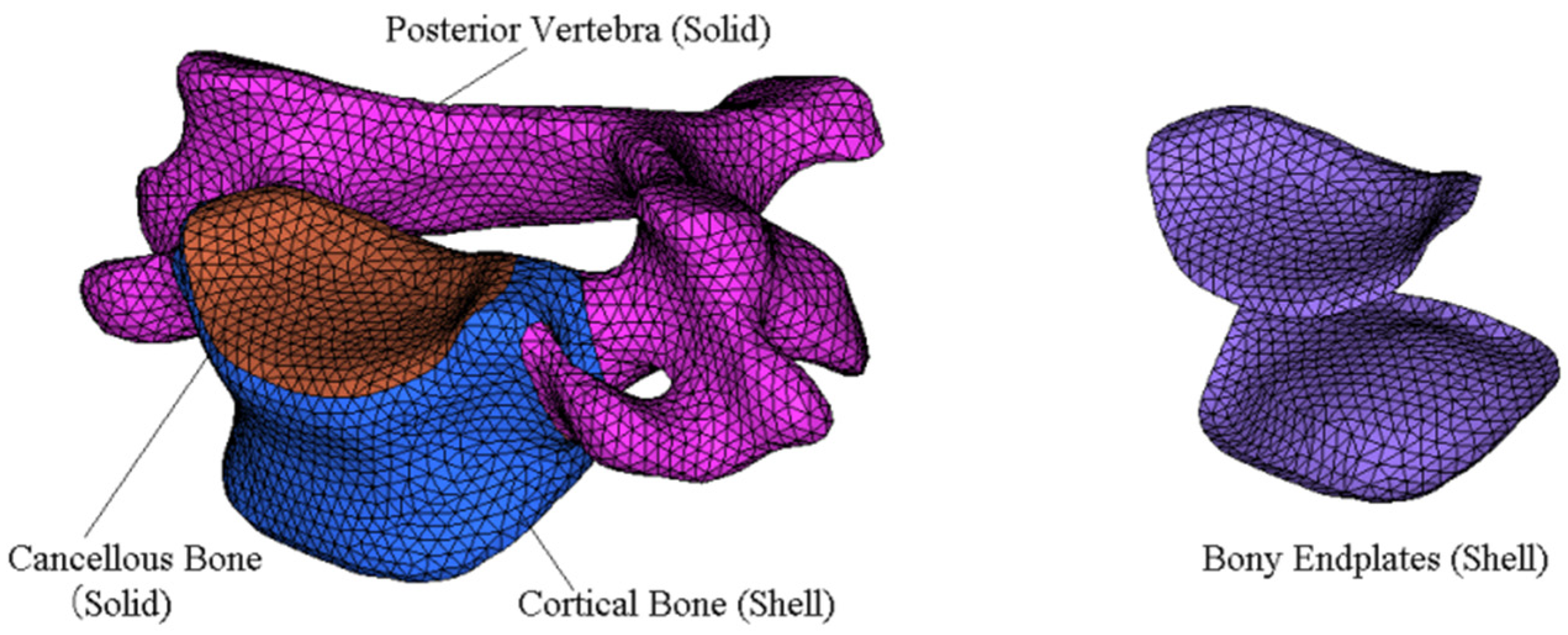
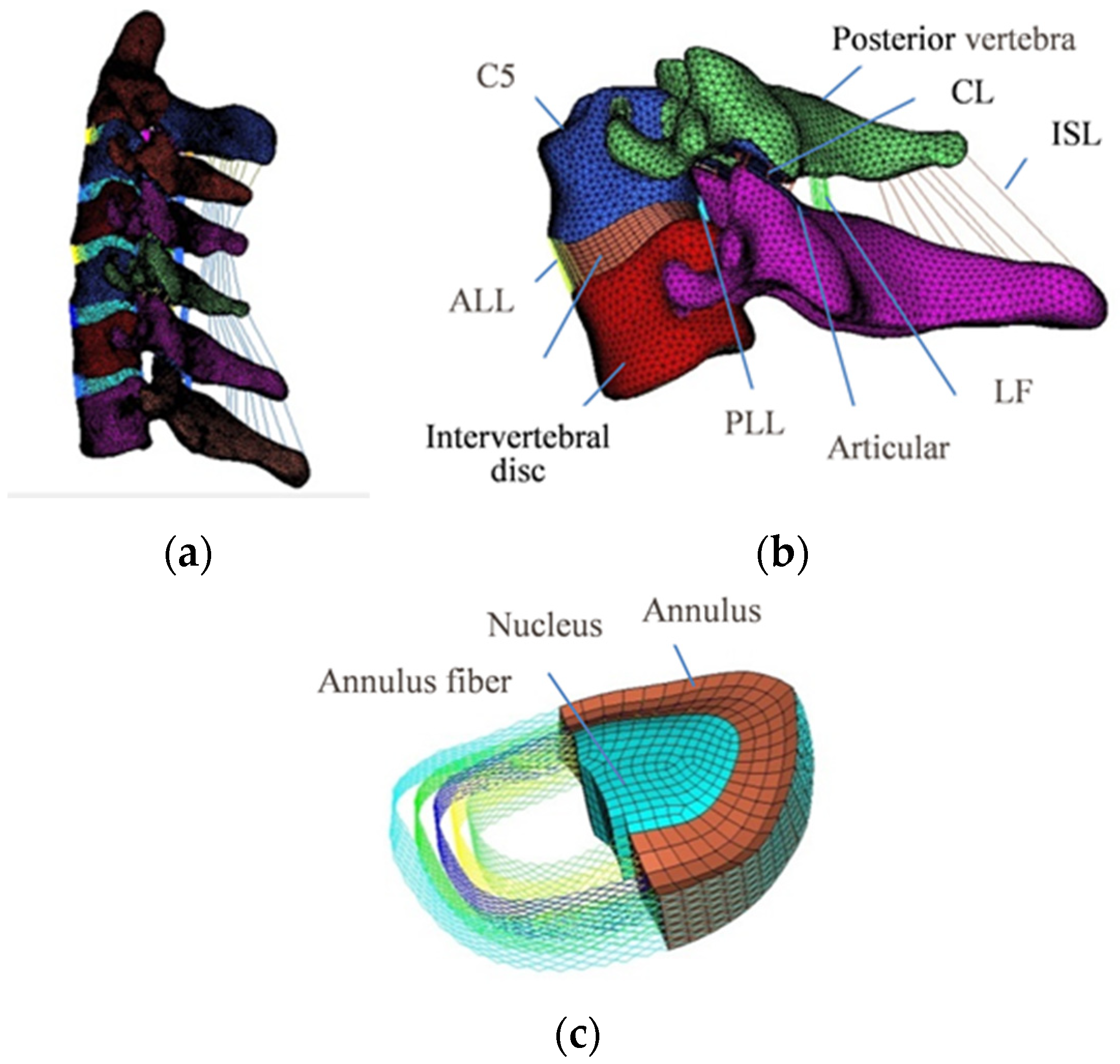




| Component | Element Type | Young’s Modulus (MPa) | Poisson’s Ratio | Reference |
|---|---|---|---|---|
| Cortical bone | S3 | 12,000 | 0.29 | [18] |
| Cancellous bone | C3D4 | 100 | 0.29 | [32] |
| Posterior vertebra | C3D4 | 3500 | 0.29 | [18] |
| Articular cartilage | C3D6 | 10.4 | 0.4 | [33] |
| Endplate | S3 | 500 | 0.4 | [18] |
| Nucleus pulposus | C3D8H | Hyperelastic (C10 = 0.348, D1 = 0.3) | [34] | |
| Annulus ground substance | C3D8R | Hyperelastic (C10 = 0.12, C01 = 0.09) | [35] | |
| Annulus fiber | T3D2 | 358–550 | 0.3 | [36] |
| ALL | CONN3D2 | Nonlinear (Incompressible) | [19,37] | |
| PLL | CONN3D2 | - | - | |
| FL | CONN3D2 | - | - | |
| ISL | CONN3D2 | - | - | |
| CL | CONN3D2 | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheng, X.; Wang, T.; Pan, C. Finite Element Analysis and Validation of Segments C2-C7 of the Cervical Spine. Metals 2022, 12, 2056. https://doi.org/10.3390/met12122056
Cheng X, Wang T, Pan C. Finite Element Analysis and Validation of Segments C2-C7 of the Cervical Spine. Metals. 2022; 12(12):2056. https://doi.org/10.3390/met12122056
Chicago/Turabian StyleCheng, Xuejin, Tao Wang, and Changjiang Pan. 2022. "Finite Element Analysis and Validation of Segments C2-C7 of the Cervical Spine" Metals 12, no. 12: 2056. https://doi.org/10.3390/met12122056







