Endoscopic Color Doppler Ultrasonographic Evaluation of Gastric Varices Secondary to Left-Sided Portal Hypertension
Abstract
:1. Introduction

2. Subjects and Methods
2.1. Patients
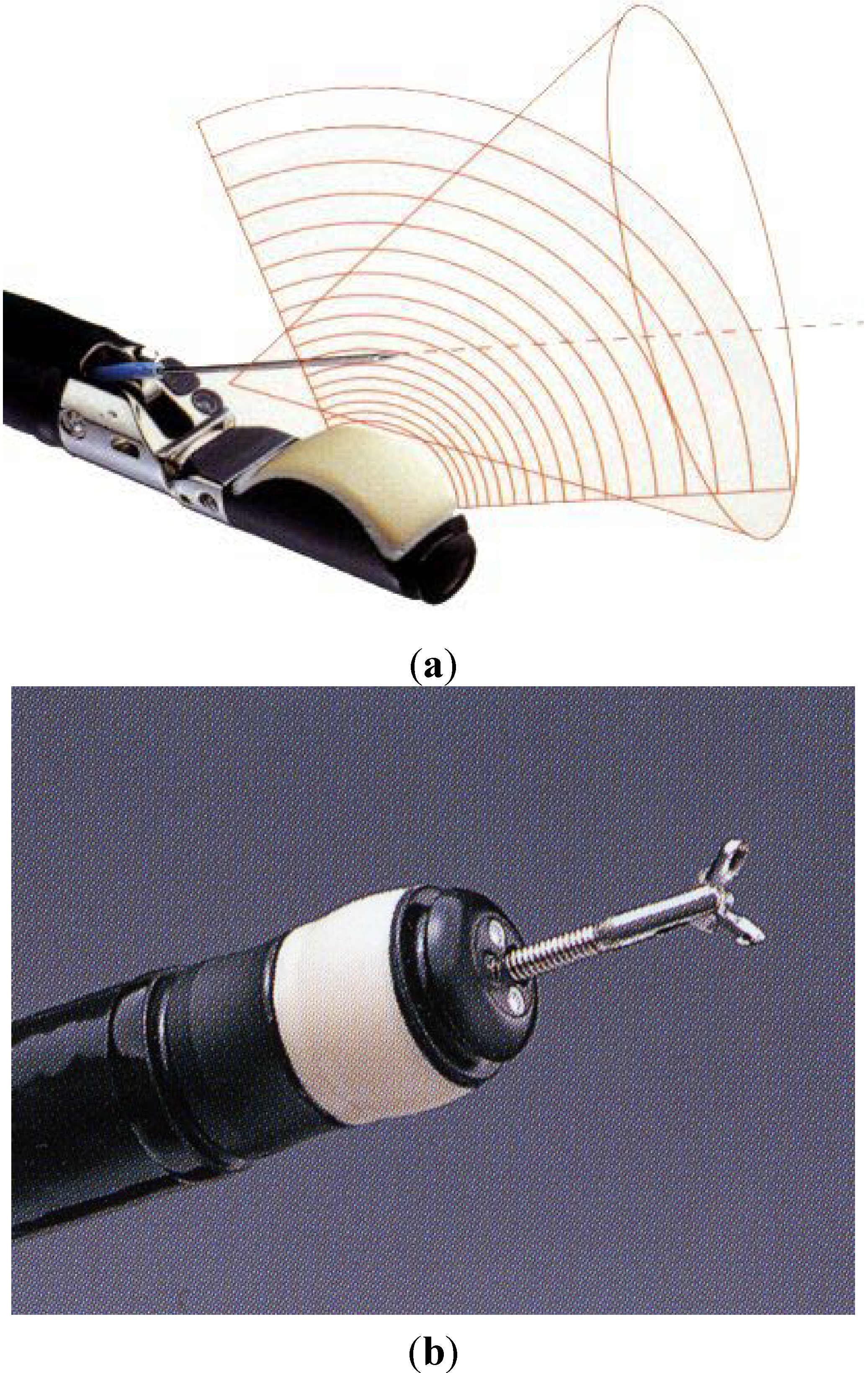
2.2. ECDUS
3. Results
3.1. Clinical Details
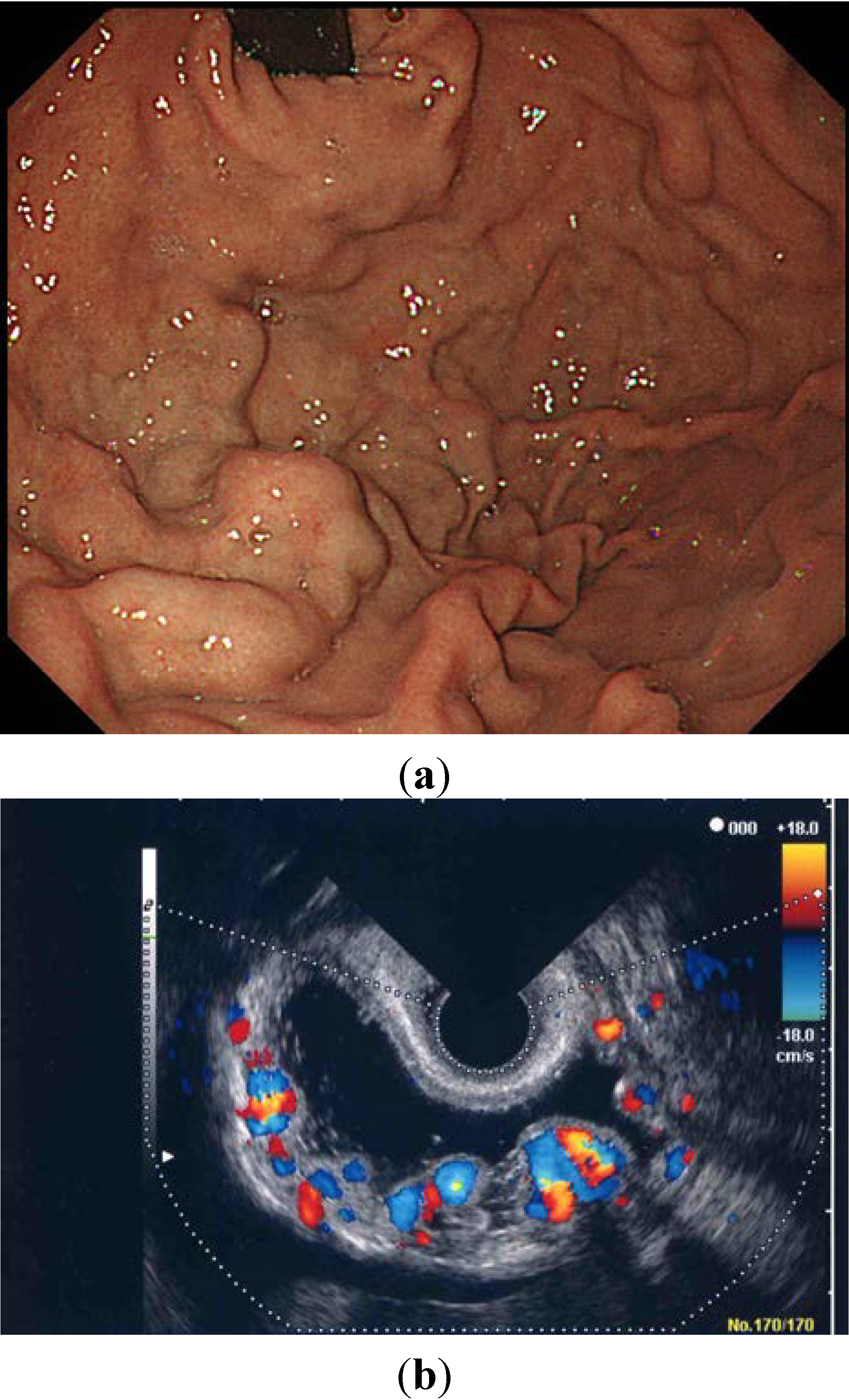
3.2. Endoscopic Findings
3.3. ECDUS

4. Discussion
5. Conclusions
Conflicts of Interest
References
- Trudeau, W.; Prindiville, T. Endoscopic injection sclerosis in bleeding gastric varices. Gastrointest. Endosc. 1986, 32, 264–268. [Google Scholar] [CrossRef]
- Cho, K.C.; Patel, Y.D.; Wachsberg, R.H.; Seeff, J. Varices in portal hypertension: Evaluation with CT. Radiographics 1995, 15, 609–622. [Google Scholar] [CrossRef]
- Sato, T.; Yamazaki, K.; Toyota, J.; Karino, Y.; Ohmura, T. Evaluation of magnetic resonance angiography in detection of gastric varices. J. Gastroenterol. 1999, 34, 321–326. [Google Scholar] [CrossRef]
- Willmann, J.K.; Weishaupt, D.; Bӧhm, T.; Pfammater, T.; Seifert, B.; Marincek, B.; Bauerfeind, P. Detection of submucosal gastric fundal varices with multi-detector row CT angiography. Gut 2003, 52, 886–892. [Google Scholar] [CrossRef]
- Marks, L.J.; Weingarten, B.; Gerst, G.R. Carcinoma of the tail of the pancreas associated with bleeding gastric varices and hypersplenism. Ann. Intern. Med. 1952, 37, 1077–1084. [Google Scholar] [CrossRef]
- Goldstein, G.B. Splenic vein thrombosis causing gastric varices and bleeding. Am. J. Gastroenterol. 1972, 58, 319–325. [Google Scholar] [PubMed]
- Moossa, A.R.; Gadd, M.A. Isolated splenic vein thrombosis. World J. Surg. 1985, 9, 384–390. [Google Scholar] [CrossRef]
- Madsen, M.; Petersen, T.H.; Sommer, H. Segmental portal hypertension. Ann. Surg. 1986, 204, 72–77. [Google Scholar] [CrossRef]
- Sutton, J.P.; Yarborough, D.Y.; Richards, J.T. Isolated splenic vein occlusion. Arch. Surg. 1970, 100, 623–626. [Google Scholar] [CrossRef]
- Babb, R.R. Splenic vein obstruction: A curable cause of variceal bleeding. Am. J. Dig. Dis. 1976, 21, 512–513. [Google Scholar] [CrossRef]
- Muhletaler, C.; Gerlock, A.J.; Goncharenko, V.; Avant, G.R.; Flexner, J.M. Gastric varices secondary to splenic vein occlusion: Radiographic diagnosis and clinical significance. Radiology 1979, 132, 593–598. [Google Scholar] [CrossRef] [PubMed]
- Ku, Y.; Kawa, Y.; Fujiwara, S.; Nishiyama, H.; Tanaka, Y.; Okumura, S.; Ohyanagi, H.; Saitoh, Y. Hemodynamic study of occlusion of the splenic vein caused by carcinoma of the pancreas. Surg. Gynecol. Obstet. 1989, 168, 17–24. [Google Scholar] [PubMed]
- Sakorafas, G.H.; Sarr, M.G.; Farley, D.R.; Farnell, M.B. The significance of sinistral portal hypertension complicating chronic pancreatitis. Am. J. Surg. 2000, 179, 129–133. [Google Scholar] [CrossRef]
- Kӧklü, S.; Yüksel, O.; Arhan, M.; Coban, S.; Basar, O.; Yolcu, O.F.; Ucar, E.; Ibis, M.; Ertugrul, I.; Sahin, B. Report of 24 left-sided portal hypertension cases: A single-center prospective cohort study. Dig. Dis. Sci. 2005, 50, 976–982. [Google Scholar] [CrossRef]
- Paramythiotis, D.; Papavramidis, T.S.; Giavroglou, K.; Potsi, S.; Girtovitis, F.; Michalopoulos, A.; Papadopoulos, V.N.; Prousalidis, J. Massive variceal bleeding secondary to splenic vein thrombosis successfully treated with splenic artery embolization: A case report. J. Med. Case Rep. 2010, 4. [Google Scholar] [CrossRef]
- Sato, T.; Kitagawa, S.; Kimura, M.; Ohmura, T.; Karino, Y. Gastric Varices Secondary to Splenic Vein Occlusion due to Pancreatic Diseases. Pancreatic Dis. Ther. S 2013, 3. [Google Scholar] [CrossRef]
- Little, A.G.; Moosa, A.R. Gastrointestinal hemorrhage from left-sided portal hypertension. An unappreciated complication of pancreatitis. Am. J. Surg. 1981, 141, 153–158. [Google Scholar] [CrossRef]
- Sarin, S.K.; Lahoti, D.; Saxena, S.P.; Murthy, N.S.; Makwana, U.K. Prevalence, classification and natural history of gastric varices: A long-term follow-up study in 568 portal hypertensive patients. Hepatology 1992, 16, 1343–1349. [Google Scholar] [CrossRef]
- Sato, T.; Yamazaki, K.; Akaike, J.; Toyota, J.; Karino, Y.; Ohmura, T. Clinical and endoscopic features of gastric varices secondary to splenic vein occlusion. Hepatol. Res. 2007, 38, 1076–1082. [Google Scholar]
- Itzchak, W.; Glickman, M. Splenic vein thrombosis in patients with a normal size spleen. Investig. Radiol. 1977, 12, 158–163. [Google Scholar] [CrossRef]
- Heider, T.R.; Azeem, S.; Galanko, J.A.; Behrns, K.E. The natural history of pancreatitis-induced splenic vein thrombosis. Ann. Surg. 2004, 239, 876–880. [Google Scholar] [CrossRef]
- Butler, J.R.; Eckert, G.J.; Zyromski, N.J.; Leonardi, M.J.; Lillemore, K.D.; Howard, T.J. Natural history of pancreatitis-induced splenic vein thrombosis: A systematic review and meta-analysis of its incidence and rate of gastrointestinal bleeding. HPB (Oxf.) 2011, 13, 839–845. [Google Scholar] [CrossRef]
- Idezuki, Y. General rules for recording endoscopic findings of esophagogastric varices. World J. Surg. 1995, 19, 420–423. [Google Scholar] [CrossRef]
- Beppu, K.; Inokuchi, K.; Koyanagi, N.; Nakayama, S.; Sakata, H.; Kitano, S.; Kobayashi, M. Prediction of variceal hemorrhage by esophageal endoscopy. Gastrointest. Endosc. 1981, 27, 213–218. [Google Scholar] [CrossRef]
- Boustiere, C.; Dumas, O.; Jouffre, C.; Letard, J.C.; Patouillard, B.; Etaix, J.P.; Barthélémy, C.; Audigier, J.C. Endoscopic ultrasonography classification of gastric varices in patients with cirrhosis. Comparison with endoscopic findings. J. Hapatol. 1993, 19, 268–272. [Google Scholar]
- Caletti, G.C.; Brocchi, E.; Ferrari, A.; Fiorino, S.; Barbara, L. Value of endoscopic ultrasonography in the management of portal hypertension. Endoscopy 1992, 24 (Suppl. 1), 342–346. [Google Scholar] [CrossRef]
- Sanyal, A.J. The value of EUS in the management of portal hypertension. Gastrointest. Endosc. 2000, 52, 575–577. [Google Scholar] [CrossRef]
- Sato, T.; Yamazaki, K.; Toyota, J.; Karino, Y.; Ohmura, T.; Akaike, J. Observation of gastric variceal flow characteristics by endoscopic ultrasonography using color Doppler. Am. J. Gastroenterol. 2008, 103, 575–580. [Google Scholar] [CrossRef]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Sato, T.; Yamazaki, K.; Kimura, M.; Toyota, J.; Karino, Y. Endoscopic Color Doppler Ultrasonographic Evaluation of Gastric Varices Secondary to Left-Sided Portal Hypertension. Diagnostics 2014, 4, 94-103. https://doi.org/10.3390/diagnostics4030094
Sato T, Yamazaki K, Kimura M, Toyota J, Karino Y. Endoscopic Color Doppler Ultrasonographic Evaluation of Gastric Varices Secondary to Left-Sided Portal Hypertension. Diagnostics. 2014; 4(3):94-103. https://doi.org/10.3390/diagnostics4030094
Chicago/Turabian StyleSato, Takahiro, Katsu Yamazaki, Mutsuumi Kimura, Jouji Toyota, and Yoshiyasu Karino. 2014. "Endoscopic Color Doppler Ultrasonographic Evaluation of Gastric Varices Secondary to Left-Sided Portal Hypertension" Diagnostics 4, no. 3: 94-103. https://doi.org/10.3390/diagnostics4030094



