The Multifaceted Role of Annexin A1 in Viral Infections
Abstract
:1. Introduction
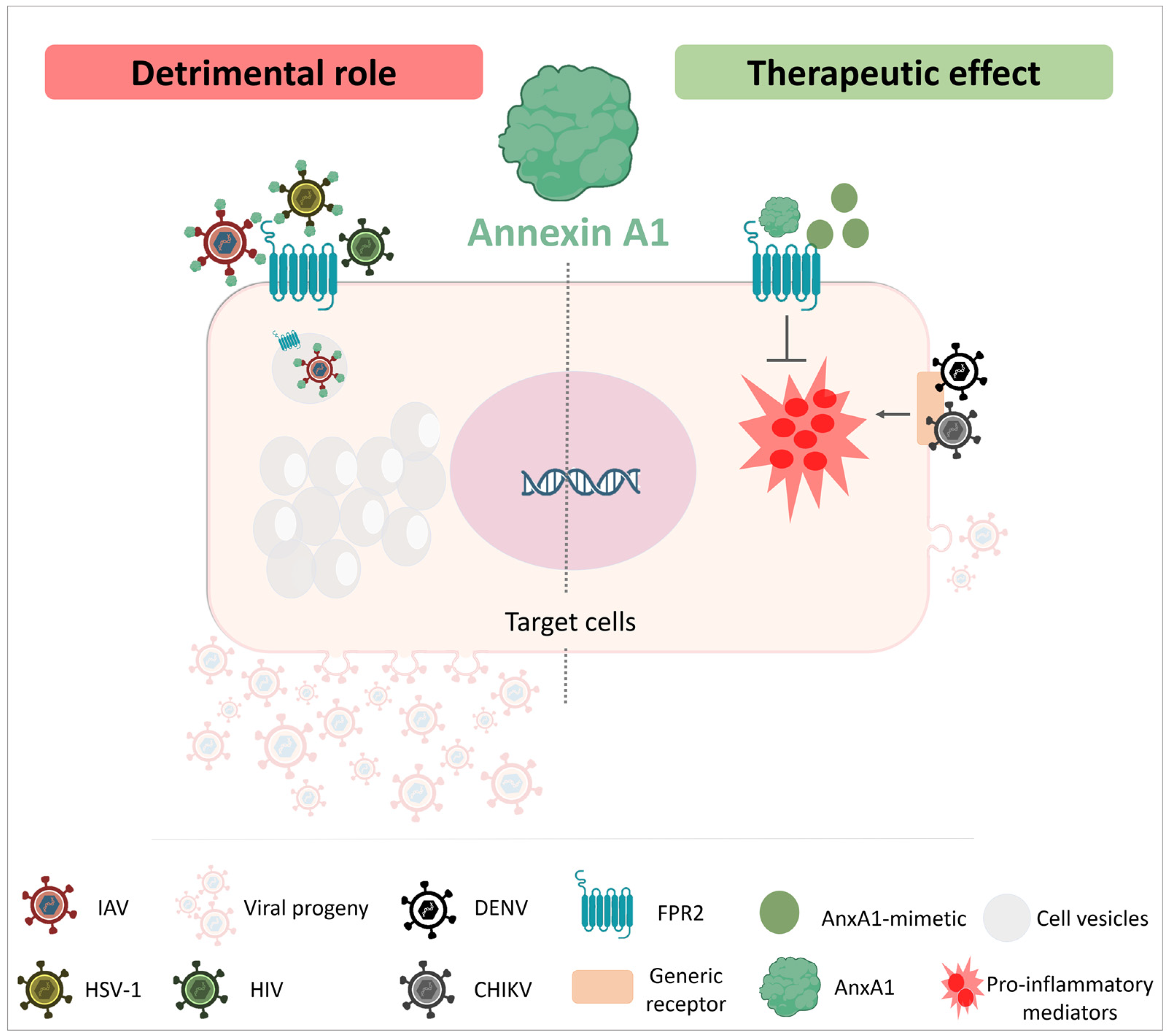
2. Inflammation, the Resolution Phase and Its Importance during Infections
3. Annexin A1
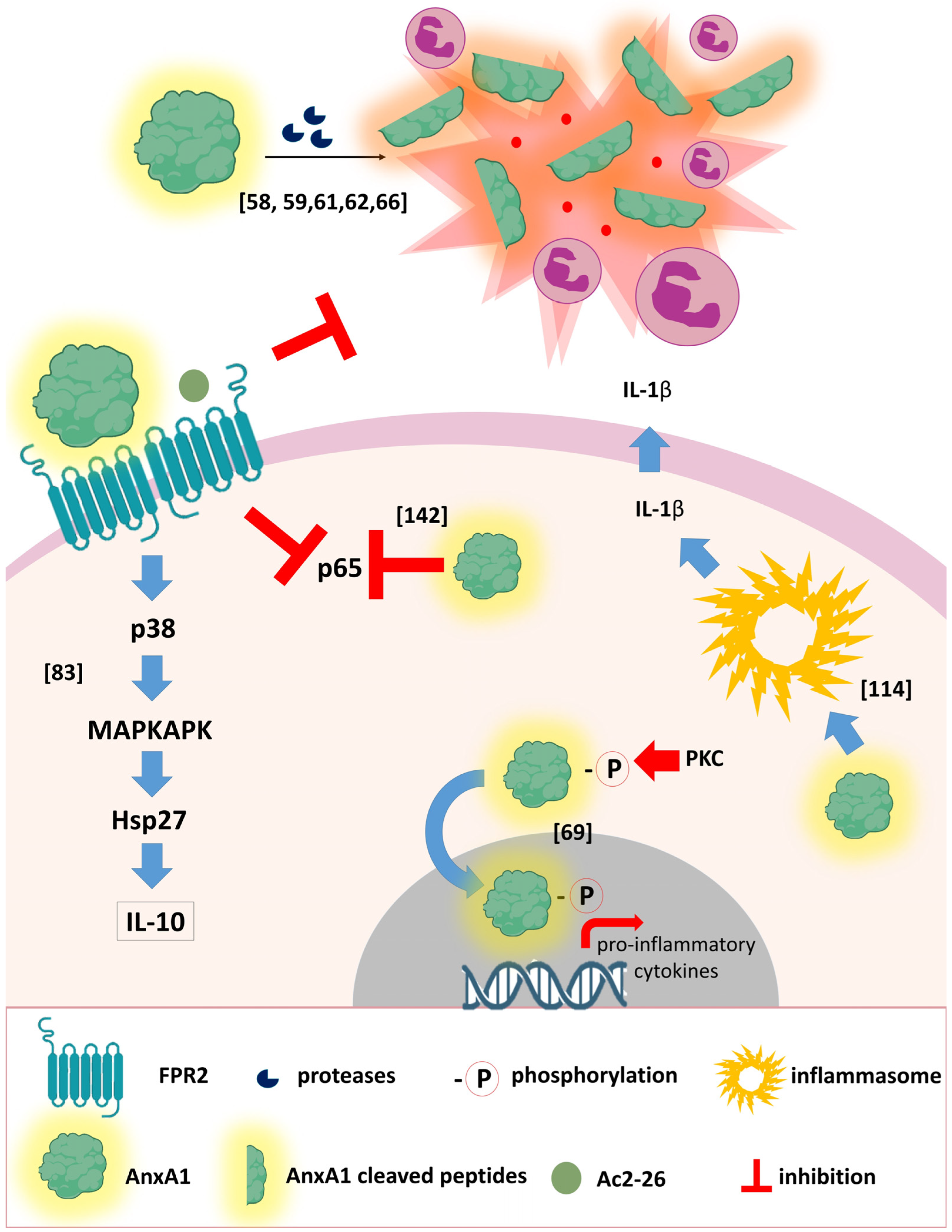
3.1. The AnxA1 Receptor
3.2. Annexin A1 during Respiratory Viral Infections
3.2.1. SARS-CoV-2 (COVID-2019)
3.2.2. Influenza Virus (IAV)
3.3. Annexin A1 during Non-Respiratory Viral Infections
3.3.1. Arbovirus
3.3.2. Hepatitis C Virus (HCV)
3.3.3. Human Papillomavirus (HPV)
3.3.4. Simian Immunodeficiency Virus (SIV)
3.3.5. Herpes Simplex Virus 1 (HSV-1)
3.3.6. Human T-Lymphotropic Virus 1 (HTLV-1)
3.3.7. Human Immunodeficiency Virus (HIV)
3.3.8. Measles/Reovirus
3.3.9. Foot and Mouth Disease Virus (FMDV)
4. Concluding Remarks
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- COVID-19 Excess Mortality Collaborators. Estimating excess mortality due to the COVID-19 pandemic: A systematic analysis of COVID-19-related mortality, 2020–21. Lancet 2022, 399, 1513–1536, Erratum in Lancet 2022, 399, 1468. [Google Scholar] [CrossRef] [PubMed]
- Sharma, V.; Sharma, M.; Dhull, D.; Sharma, Y.; Kaushik, S.; Kaushik, S. Zika virus: An emerging challenge to public health worldwide. Can. J. Microbiol. 2020, 66, 87–98. [Google Scholar] [CrossRef]
- Paget, J.; Spreeuwenberg, P.; Charu, V.; Taylor, R.J.; Iuliano, A.D.; Bresee, J.; Simonsen, L.; Viboud, C.; Global Seasonal Influenza-Associated Mortality Collaborator Network and GLaMOR Collaborating Teams. Global mortality associated with seasonal influenza epidemics: New burden estimates and predictors from the GLaMOR Project. J. Glob. Health 2019, 9, 020421. [Google Scholar] [CrossRef]
- Jacob, S.T.; Crozier, I.; Fischer, W.A., 2nd; Hewlett, A.; Kraft, C.S.; Vega, M.A.; Soka, M.J.; Wahl, V.; Griffiths, A.; Bollinger, L.; et al. Ebola virus disease. Nat. Rev. Dis. Prim. 2020, 6, 13. [Google Scholar] [CrossRef]
- Lanrewaju, A.A.; Enitan-Folami, A.M.; Sabiu, S.; Edokpayi, J.N.; Swalaha, F.M. Global public health implications of human exposure to viral contaminated water. Front. Microbiol. 2022, 13, 981896. [Google Scholar] [CrossRef] [PubMed]
- Torres-Flores, J.M.; Reyes-Sandoval, A.; Salazar, M.I. Dengue Vaccines: An Update. Biodrugs 2022, 36, 325–336. [Google Scholar] [CrossRef]
- Stephenson, K.E. Novel chikungunya vaccine shows promise for durable protection. Lancet Infect. Dis. 2022, 22, 1259–1261. [Google Scholar] [CrossRef]
- Medzhitov, R. The spectrum of inflammatory responses. Science 2021, 374, 1070–1075. [Google Scholar] [CrossRef] [PubMed]
- Maskin, L.P.; Bonelli, I.; Olarte, G.L.; Palizas, J.F.; Velo, A.E.; Lurbet, M.F.; Lovazzano, P.; Kotsias, S.; Attie, S.; Saubidet, I.L.; et al. High- Versus Low-Dose Dexamethasone for the Treatment of COVID-19-Related Acute Respiratory Distress Syndrome: A Multicenter, Randomized Open-Label Clinical Trial. J. Intensiv. Care Med. 2022, 37, 491–499. [Google Scholar] [CrossRef] [PubMed]
- WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group; Sterne, J.A.C.; Murthy, S.; Diaz, J.V.; Slutsky, A.S.; Villar, J.; Angus, D.C.; Annane, D.; Azevedo, L.C.P.; Berwanger, O.; et al. Association Between Administration of Systemic Corticosteroids and Mortality Among Critically Ill Patients With COVID-19: A Meta-analysis. JAMA 2020, 324, 1330–1341. [Google Scholar] [CrossRef] [PubMed]
- Buckley, C.D.; Gilroy, D.; Serhan, C.N.; Stockinger, B.; Tak, P.P. The resolution of inflammation. Nat. Rev. Immunol. 2013, 13, 59–66. [Google Scholar] [CrossRef]
- Fullerton, J.N.; Gilroy, D.W. Resolution of inflammation: A new therapeutic frontier. Nat. Rev. Drug Discov. 2016, 15, 551–567. [Google Scholar] [CrossRef]
- Sugimoto, M.A.; Vago, J.P.; Teixeira, M.M.; Sousa, L.P. Annexin A1 and the Resolution of Inflammation: Modulation of Neutrophil Recruitment, Apoptosis, and Clearance. J. Immunol. Res. 2016, 2016, 8239258. [Google Scholar] [CrossRef]
- Sousa, L.P.; Pinho, V.; Teixeira, M.M. Harnessing inflammation resolving-based therapeutic agents to treat pulmonary viral infections: What can the future offer to COVID-19? Br. J. Pharmacol. 2020, 177, 3898–3904. [Google Scholar] [CrossRef]
- Sugimoto, M.A.; Vago, J.P.; Perretti, M.; Teixeira, M.M. Mediators of the Resolution of the Inflammatory Response. Trends Immunol. 2019, 40, 212–227. [Google Scholar] [CrossRef]
- Tavares, L.P.; Melo, E.M.; Sousa, L.P.; Teixeira, M.M. Pro-resolving therapies as potential adjunct treatment for infectious diseases: Evidence from studies with annexin A1 and angiotensin-(1-7). Semin. Immunol. 2022, 59, 101601. [Google Scholar] [CrossRef] [PubMed]
- Gavins, F.N.E.; Yona, S.; Kamal, A.M.; Flower, R.J.; Perretti, M. Leukocyte antiadhesive actions of annexin 1: ALXR- and FPR-related anti-inflammatory mechanisms. Blood 2003, 101, 4140–4147. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, A.B.; Caloi, C.M.; Pimenta, S.T.S.; Seshayyan, S.; Govindarajulu, S.; Souto, F.J.D.; Damazo, A.S. Expression of annexin-A1 in blood and tissue leukocytes of leprosy patients. Rev. Soc. Bras. Med. Trop. 2020, 53, e20200277. [Google Scholar] [CrossRef]
- Schloer, S.; Hübel, N.; Masemann, D.; Pajonczyk, D.; Brunotte, L.; Ehrhardt, C.; Brandenburg, L.; Ludwig, S.; Gerke, V.; Rescher, U. The annexin A1/FPR2 signaling axis expands alveolar macrophages, limits viral replication, and attenuates pathogenesis in the murine influenza A virus infection model. FASEB J. 2019, 33, 12188–12199. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.-C.; Wu, S.-R.; Yao, H.-W.; Ling, P.; Perng, G.-C.; Chiu, Y.-C.; Hsu, S.-M.; Chen, S.-H. Suppression of annexin A1 and its receptor reduces herpes simplex virus 1 lethality in mice. PLoS Pathog. 2022, 18, e1010692. [Google Scholar] [CrossRef]
- Yap, G.L.R.; Sachaphibulkij, K.; Foo, S.L.; Cui, J.; Fairhurst, A.-M.; Lim, L.H.K. Annexin-A1 promotes RIG-I-dependent signaling and apoptosis via regulation of the IRF3–IFNAR–STAT1–IFIT1 pathway in A549 lung epithelial cells. Cell Death Dis. 2020, 11, 463. [Google Scholar] [CrossRef] [PubMed]
- Garcia, C.C.; Guabiraba, R.; Soriani, F.M.; Teixeira, M.M. The development of anti-inflammatory drugs for infectious diseases. Discov. Med. 2010, 10, 479–488. [Google Scholar]
- Machado, M.G.; Tavares, L.P.; Souza, G.V.S.; Queiroz-Junior, C.M.; Ascenção, F.R.; Lopes, M.E.; Garcia, C.C.; Menezes, G.B.; Perretti, M.; Russo, R.C.; et al. The Annexin A1/FPR2 pathway controls the inflammatory response and bacterial dissemination in experimental pneumococcal pneumonia. FASEB J. 2020, 34, 2749–2764. [Google Scholar] [CrossRef] [PubMed]
- Costa, V.V.; Sugimoto, M.A.; Hubner, J.; Bonilha, C.S.; Queiroz-Junior, C.M.; Gonçalves-Pereira, M.H.; Chen, J.; Gobbetti, T.; Rodrigues, G.O.L.; Bambirra, J.L.; et al. Targeting the Annexin A1-FPR2/ALX pathway for host-directed therapy in dengue disease. Elife 2022, 11, e73853. [Google Scholar] [CrossRef]
- Vago, J.P.; Nogueira, C.R.C.; Tavares, L.P.; Soriani, F.M.; Lopes, F.; Russo, R.C.; Pinho, V.; Teixeira, M.M.; Sousa, L.P. Annexin A1 modulates natural and glucocorticoid-induced resolution of inflammation by enhancing neutrophil apoptosis. J. Leukoc. Biol. 2012, 92, 249–258. [Google Scholar] [CrossRef]
- de Araújo, S.; Costa, V.R.d.M.; Santos, F.M.; de Sousa, C.D.F.; Moreira, T.P.; Gonçalves, M.R.; Félix, F.B.; Queiroz-Junior, C.M.; Campolina-Silva, G.H.; Nogueira, M.L.; et al. Annexin A1-FPR2/ALX Signaling Axis Regulates Acute Inflammation during Chikungunya Virus Infection. Cells 2022, 11, 2717. [Google Scholar] [CrossRef]
- Tracy, R.P. The Five Cardinal Signs of Inflammation: Calor, Dolor, Rubor, Tumor ... and Penuria (Apologies to Aulus Cornelius Celsus, De medicina, c. A.D. 25). J. Gerontol. A Biol. Sci. Med. Sci. 2006, 61, 1051–1052. [Google Scholar] [CrossRef] [PubMed]
- Nathan, C.; Ding, A. Nonresolving Inflammation. Cell 2010, 140, 871–882. [Google Scholar] [CrossRef] [PubMed]
- Nathan, C. Points of control in inflammation. Nature 2002, 420, 846–852. [Google Scholar] [CrossRef]
- Kotas, M.E.; Medzhitov, R. Homeostasis, inflammation, and disease susceptibility. Cell 2015, 160, 816–827. [Google Scholar] [CrossRef]
- Abe, T.; Marutani, Y.; Shoji, I. Cytosolic DNA-sensing immune response and viral infection. Microbiol. Immunol. 2019, 63, 51–64. [Google Scholar] [CrossRef]
- Zhang, Q.; Xiang, R.; Huo, S.; Zhou, Y.; Jiang, S.; Wang, Q.; Yu, F. Molecular mechanism of interaction between SARS-CoV-2 and host cells and interventional therapy. Signal Transduct. Target. Ther. 2021, 6, 233. [Google Scholar] [CrossRef] [PubMed]
- Mdkhana, B.; Saheb-Sharif Askari, N.; Ramakrishnan, R.K.; Goel, S.; Hamid, Q.; Halwani, R. Nucleic Acid-Sensing Pathways During SARS-CoV-2 Infection: Expectations versus Reality. J. Inflamm. Res. 2021, 14, 199–216. [Google Scholar] [CrossRef] [PubMed]
- Serhan, C.N.; Chiang, N.; Van Dyke, T.E. Resolving inflammation: Dual anti-inflammatory and pro-resolution lipid mediators. Nat. Rev. Immunol. 2008, 8, 349–361. [Google Scholar] [CrossRef] [PubMed]
- Serhan, C.N.; Brain, S.D.; Buckley, C.D.; Gilroy, D.W.; Haslett, C.; O’Neill, L.A.J.; Perretti, M.; Rossi, A.G.; Wallace, J.L. Resolution of in flammation: State of the art, definitions and terms. FASEB J. 2007, 21, 325–332. [Google Scholar] [CrossRef]
- Perretti, M.; Leroy, X.; Bland, E.J.; Montero-Melendez, T. Resolution Pharmacology: Opportunities for Therapeutic Innovation in Inflammation. Trends Pharmacol. Sci. 2015, 36, 737–755. [Google Scholar] [CrossRef]
- Kourtzelis, I.; Hajishengallis, G.; Chavakis, T. Phagocytosis of Apoptotic Cells in Resolution of Inflammation. Front. Immunol. 2020, 11, 553. [Google Scholar] [CrossRef]
- Headland, S.E.; Norling, L.V. The resolution of inflammation: Principles and challenges. Semin. Immunol. 2015, 27, 149–160. [Google Scholar] [CrossRef] [PubMed]
- Vago, J.P.; Tavares, L.P.; Riccardi, C.; Teixeira, M.M.; Sousa, L.P. Exploiting the pro-resolving actions of glucocorticoid-induced proteins Annexin A1 and GILZ in infectious diseases. Biomed. Pharmacother. 2020, 133, 111033. [Google Scholar] [CrossRef] [PubMed]
- Flower, R.J.; Blackwell, G.J. Anti-inflammatory steroids induce biosynthesis of a phospholipase A2 inhibitor which prevents prostaglandin generation. Nature 1979, 278, 456–459. [Google Scholar] [CrossRef]
- Flower, R. Eleventh Gaddum memorial lecture. Lipocortin and the mechanism of action of the glucocorticoids. Br. J. Pharmacol. 1988, 94, 987–1015. [Google Scholar] [CrossRef] [PubMed]
- D’Acunto, C.W.; Gbelcova, H.; Festa, M.; Ruml, T. The complex understanding of Annexin A1 phosphorylation. Cell Signal. 2014, 26, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Ernst, J.D.; Hoye, E.; Blackwood, R.A.; Jaye, D. Purification and characterization of an abundant cytosolic protein from human neutrophils that promotes Ca2(+)-dependent aggregation of isolated specific granules. J. Clin. Investig. 1990, 85, 1065–1071. [Google Scholar] [CrossRef] [PubMed]
- Morand, E.; Hutchinson, P.; Hargreaves, A.; Goulding, N.J.; Boyce, N.W.; Holdsworth, S.R. Detection of intracellular lipocortin 1 in human leukocyte subsets. Clin. Immunol. Immunopathol. 1995, 76, 195–202. [Google Scholar] [CrossRef]
- Perretti, M.; Christian, H.; Wheller, S.K.; Aiello, I.; Mugridge, K.G.; Morris, J.F.; Flower, R.J.; Goulding, N.J. Annexin I is stored within gelatinase granules of human neutrophil and mobilized on the cell surface upon adhesion but not phagocytosis. Cell Biol. Int. 2000, 24, 163–174. [Google Scholar] [CrossRef]
- Perretti, M.; D’Acquisto, F. Annexin A1 and glucocorticoids as effectors of the resolution of inflammation. Nat. Rev. Immunol. 2009, 9, 62–70. [Google Scholar] [CrossRef]
- Roviezzo, F.; Getting, S.J.; Paul-Clark, M.J.; Yona, S.; Gavins, F.N.; Perretti, M.; Hannon, R.; Croxtall, J.D.; Buckingham, J.C.; Flower, R.J. The annexin-1 knockout mouse: What it tells us about the inflammatory response. J. Physiol. Pharmacol. 2002, 53, 541–553. [Google Scholar]
- Hannon, R.; Croxtall, J.D.; Getting, S.J.; Roviezzo, F.; Yona, S.; Paul-Clark, M.J.; Gavins, F.N.E.; Perretti, M.; Morris, J.F.; Buckingham, J.C.; et al. Aberrant inflammation and resistance to glucocorticoids in annexin 1-/- mouse. FASEB J. 2002, 17, 253–255. [Google Scholar] [CrossRef]
- Grewal, T.; Rentero, C.; Enrich, C.; Wahba, M.; Raabe, C.; Rescher, U. Annexin Animal Models—From Fundamental Principles to Translational Research. Int. J. Mol. Sci. 2021, 22, 3439. [Google Scholar] [CrossRef]
- Perretti, M.; Ahluwalia, A.; Harris, J.G.; Goulding, N.J.; Flower, R.J. Lipocortin-1 fragments inhibit neutrophil accumulation and neu-trophil-dependent edema in the mouse. A qualitative comparison with an anti-CD11b monoclonal antibody. J. Immunol. 1993, 151, 4306–4314. [Google Scholar] [CrossRef]
- Yang, Y.H.; Morand, E.F.; Getting, S.J.; Paul-Clark, M.; Liu, D.L.; Yona, S.; Hannon, R.; Buckingham, J.C.; Perretti, M.; Flower, R.J. Modulation of inflammation and response to dexamethasone by Annexin 1 in antigen-induced arthritis. Arthritis Rheum. 2004, 50, 976–984. [Google Scholar] [CrossRef] [PubMed]
- Ayoub, S.S.; Yazid, S.; Flower, R.J. Increased susceptibility of annexin-A1 null mice to nociceptive pain is indicative of a spinal antinociceptive action of annexin-A1. Br. J. Pharmacol. 2008, 154, 1135–1142. [Google Scholar] [CrossRef]
- Chatterjee, B.E.; Yona, S.; Rosignoli, G.; Young, R.E.; Nourshargh, S.; Flower, R.J.; Perretti, M. Annexin 1-deficient neutrophils exhibit enhanced transmigration in vivo and increased responsiveness in vitro. J. Leukoc. Biol. 2005, 78, 639–646. [Google Scholar] [CrossRef] [PubMed]
- Sakaguchi, M.; Murata, H.; Sonegawa, H.; Sakaguchi, Y.; Futami, J.-I.; Kitazoe, M.; Yamada, H.; Huh, N.-H. Truncation of annexin A1 Is a regulatory lever for linking epidermal growth factor signaling with cytosolic phospholipase A2 in normal and malignant squamous epithelial cells. J. Biol. Chem. 2007, 282, 35679–35686. [Google Scholar] [CrossRef]
- Wang, W.; Creutz, C.E. Role of the amino-terminal domain in regulating interactions of annexin I with membranes: Effects of amino-terminal truncation and mutagenesis of the phosphorylation sites. Biochemistry 1994, 33, 275–282. [Google Scholar] [CrossRef] [PubMed]
- Rescher, U.; Goebeler, V.; Wilbers, A.; Gerke, V. Proteolytic cleavage of annexin 1 by human leukocyte elastase. Biochim. Biophys. Acta. 2006, 1763, 1320–1324. [Google Scholar] [CrossRef] [PubMed]
- Vong, L.; D’Acquisto, F.; Pederzoli-Ribeil, M.; Lavagno, L.; Flower, R.J.; Witko-Sarsat, V.; Perretti, M. Annexin 1 cleavage in activated neutrophils: A pivotal role for proteinase 3. J. Biol. Chem. 2007, 282, 29998–30004. [Google Scholar] [CrossRef] [PubMed]
- Chung, Y.W.; Oh, H.Y.; Kim, J.Y.; Kim, J.H.; Kim, I.Y. Allergen-induced proteolytic cleavage of annexin-1 and activation of cytosolic phospholipase A2 in the lungs of a mouse model of asthma. Proteomics 2004, 4, 3328–3334. [Google Scholar] [CrossRef]
- Tsao, F.H.C.; Meyer, K.C.; Chen, X.; Rosenthal, N.S.; Hu, J. Degradation of annexin I in bronchoalveolar lavage fluid from patients with cystic fibrosis. Am. J. Respir. Cell Mol. Biol. 1998, 18, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Tsao, F.H.C.; Xiang, Z.; Abbasi, A.; Meyer, K.C. Neutrophil necrosis and annexin 1 degradation associated with airway inflammation in lung transplant recipients with cystic fibrosis. BMC Pulm. Med. 2012, 12, 44. [Google Scholar] [CrossRef]
- Smith, S.F.; Tetley, T.D.; Guz, A.; Flower, R.J. Detection of lipocortin 1 in human lung lavage fluid: Lipocortin degradation as a possible proteolytic mechanism in the control of inflammatory mediators and inflammation. Environ. Health Perspect. 1990, 85, 135–144. [Google Scholar] [CrossRef]
- Vago, J.P.; Tavares, L.P.; Sugimoto, M.A.; Lima, G.L.N.; Galvão, I.; de Caux, T.R.; Lima, K.M.; Ribeiro, A.L.C.; Carneiro, F.S.; Nunes, F.F.C.; et al. Proresolving Actions of Synthetic and Natural Protease Inhibitors Are Mediated by Annexin A1. J. Immunol. 2016, 196, 1922–1932. [Google Scholar] [CrossRef]
- Perretti, M.; Wheller, S.K.; Flower, R.J.; Wahid, S.; Pitzalis, C. Modulation of cellular annexin I in human leukocytes infiltrating DTH skin reactions. J. Leukoc. Biol. 1999, 65, 583–589. [Google Scholar] [CrossRef] [PubMed]
- Lima, K.M.; Vago, J.P.; Caux, T.R.; Negreiros-Lima, G.L.; Sugimoto, M.A.; Tavares, L.P.; Arribada, R.G.; Carmo, A.A.F.; Galvão, I.; Costa, B.R.C.; et al. The resolution of acute inflammation induced by cyclic AMP is dependent on annexin A1. J. Biol. Chem. 2017, 292, 13758–13773. [Google Scholar] [CrossRef]
- Galvão, I.; Vago, J.P.; Barroso, L.C.; Tavares, L.P.; Queiroz-Junior, C.M.; Costa, V.V.; Carneiro, F.S.; Ferreira, T.P.; Silva, P.M.R.; Amaral, F.A.; et al. Annexin A1 promotes timely resolution of inflammation in murine gout. Eur. J. Immunol. 2017, 47, 585–596. [Google Scholar] [CrossRef]
- Williams, S.L.; Milne, I.R.; Bagley, C.J.; Gamble, J.R.; Vadas, M.A.; Pitson, S.M.; Khew-Goodall, Y. A proinflammatory role for proteolytically cleaved annexin A1 in neutrophil transendothelial migration. J. Immunol. 2010, 185, 3057–3063. [Google Scholar] [CrossRef]
- Rüger, M.; Kipp, E.; Schubert, N.; Schröder, N.; Pufe, T.; Stope, M.B.; Kipp, M.; Blume, C.; Tauber, S.C.; Brandenburg, L.-O. The formyl peptide receptor agonist Ac2-26 alleviates neuroinflammation in a mouse model of pneumococcal meningitis. J. NeuroInflamm. 2020, 17, 325. [Google Scholar] [CrossRef]
- Chiang, N.; Serhan, C.N.; Dahlén, S.E.; Drazen, J.M.; Hay, D.W.P.; Rovati, G.E.; Shimizu, T.; Yokomizo, T.; Brink, C. The lipoxin receptor ALX: Potent ligand-specific and stereoselective actions in vivo. Pharmacol. Rev. 2006, 58, 463–487. [Google Scholar] [CrossRef] [PubMed]
- Zhao, B.; Wang, J.; Liu, L.; Li, X.; Liu, S.; Xia, Q.; Shi, J. Annexin A1 translocates to nucleus and promotes the expression of pro-inflammatory cytokines in a PKC-dependent manner after OGD/R. Sci. Rep. 2016, 6, 27028. [Google Scholar] [CrossRef] [PubMed]
- McArthur, S.; Juban, G.; Gobbetti, T.; Desgeorges, T.; Theret, M.; Gondin, J.; Toller-Kawahisa, J.E.; Reutelingsperger, C.P.; Chazaud, B.; Perretti, M.; et al. Annexin A1 drives macrophage skewing to accelerate muscle regeneration through AMPK activation. J. Clin. Investig. 2020, 130, 1156–1167. [Google Scholar] [CrossRef] [PubMed]
- Ferraro, B.; Leoni, G.; Hinkel, R.; Ormanns, S.; Paulin, N.; Ortega-Gomez, A.; Viola, J.R.; de Jong, R.; Bongiovanni, D.; Bozoglu, T.; et al. Pro-Angiogenic Macrophage Phenotype to Promote Myocardial Repair. J. Am. Coll. Cardiol. 2019, 73, 2990–3002. [Google Scholar] [CrossRef] [PubMed]
- Oliani, S.M.; Ciocca, G.A.; Pimentel, T.A.; Damazo, A.S.; Gibbs, L.; Perretti, M. Fluctuation of annexin-A1 positive mast cells in chronic granulomatous inflammation. Inflamm. Res. 2008, 57, 450–456. [Google Scholar] [CrossRef] [PubMed]
- Sinniah, A.; Yazid, S.; Bena, S.; Oliani, S.M.; Perretti, M.; Flower, R.J. Endogenous Annexin-A1 Negatively Regulates Mast Cell-Mediated Allergic Reactions. Front. Pharmacol. 2019, 10, 1313. [Google Scholar] [CrossRef] [PubMed]
- Rivière, S.; Challet, L.; Fluegge, D.; Spehr, M.; Rodriguez, I. Formyl peptide receptor-like proteins are a novel family of vomeronasal chemosensors. Nature 2009, 459, 574–577. [Google Scholar] [CrossRef]
- Qin, C.X.; Norling, L.V.; Vecchio, E.A.; Brennan, E.P.; May, L.T.; Wootten, D.; Godson, C.; Perretti, M.; Ritchie, R.H. Formylpeptide receptor 2: Nomenclature, structure, signalling and translational perspectives: IUPHAR review 35. Br. J. Pharmacol. 2022, published online ahead of print. [Google Scholar] [CrossRef]
- Chen, T.; Xiong, M.; Zong, X.; Ge, Y.; Zhang, H.; Wang, M.; Han, G.W.; Yi, C.; Ma, L.; Ye, R.D.; et al. Structural basis of ligand binding modes at the human formyl peptide receptor 2. Nat. Commun. 2020, 11, 1208. [Google Scholar] [CrossRef]
- Zhuang, Y.; Liu, H.; Zhou, X.E.; Verma, R.K.; de Waal, P.W.; Jang, W.; Xu, T.-H.; Wang, L.; Meng, X.; Zhao, G.; et al. Structure of formylpeptide receptor 2-Gi complex reveals insights into ligand recognition and signaling. Nat. Commun. 2020, 11, 885. [Google Scholar] [CrossRef]
- He, H.Q.; Troksa, E.L.; Caltabiano, G.; Pardo, L.; Ye, R.D. Structural determinants for the interaction of formyl peptide receptor 2 with peptide ligands. J. Biol. Chem. 2014, 289, 2295–2306, Erratum in J. Biol. Chem. 2014, 289, 4814. [Google Scholar] [CrossRef]
- Ye, R.D.; Boulay, F.; Wang, J.M.; Dahlgren, C.; Gerard, C.; Parmentier, M.; Serhan, C.N.; Murphy, P.M. International union of basic and clinical pharmacology. LXXIII. nomenclature for the formyl peptide receptor (FPR) family. Pharmacol. Rev. 2009, 61, 119–161. [Google Scholar] [CrossRef]
- Zhuang, Y.; Wang, L.; Guo, J.; Sun, D.; Wang, Y.; Liu, W.; Xu, H.E.; Zhang, C. Molecular recognition of formylpeptides and diverse agonists by the formylpeptide receptors FPR1 and FPR2. Nat. Commun. 2022, 13, 1054. [Google Scholar] [CrossRef]
- Ge, Y.; Zhang, S.; Wang, J.; Xia, F.; Wan, J.; Lu, J.; Ye, R.D. Dual modulation of formyl peptide receptor 2 by aspirin-triggered lipoxin contributes to its anti-inflammatory activity. FASEB J. 2020, 34, 6920–6933. [Google Scholar] [CrossRef]
- Ge, Y.J.; Liao, Q.W.; Xu, Y.C.; Zhao, Q.; Wu, B.L.; Ye, R.D. Anti-inflammatory signaling through G protein-coupled receptors. Acta Pharmacol. Sin. 2020, 41, 1531–1538. [Google Scholar] [CrossRef] [PubMed]
- Cooray, S.N.; Gobbetti, T.; Montero-Melendez, T.; McArthur, S.; Thompson, D.; Clark, A.J.L.; Flower, R.J.; Perretti, M. Ligand-specific conformational change of the G-protein–coupled receptor ALX/FPR2 determines proresolving functional responses. Proc. Natl. Acad. Sci. USA 2013, 110, 18232–18237. [Google Scholar] [CrossRef]
- Han, P.F.; Che, X.D.; Li, H.Z.; Gao, Y.Y.; Wei, X.C.; Li, P.C. Annexin A1 involved in the regulation of inflammation and cell signaling pathways. Chin. J. Traumatol. 2020, 23, 96–101. [Google Scholar] [CrossRef] [PubMed]
- Tcherniuk, S.; Cenac, N.; Comte, M.; Frouard, J.; Errazuriz-Cerda, E.; Galabov, A.; Morange, P.-E.; Vergnolle, N.; Si-Tahar, M.; Alessi, M.-C.; et al. Formyl Peptide Receptor 2 Plays a Deleterious Role During Influenza A Virus Infections. J. Infect. Dis. 2016, 214, 237–247. [Google Scholar] [CrossRef]
- Bist, P.; Shu, S.; Lee, H.; Arora, S.; Nair, S.; Lim, J.Y.; Dayalan, J.; Gasser, S.; Biswas, S.K.; Fairhurst, A.-M.; et al. Annexin-A1 regulates TLR-mediated IFN-β production through an interaction with TANK-binding kinase 1. J. Immunol. 2013, 191, 4375–4382. [Google Scholar] [CrossRef] [PubMed]
- Ampomah, P.B.; Moraes, L.A.; Lukman, H.M.; Lim, L.H.K. Formyl peptide receptor 2 is regulated by RNA mimics and viruses through an IFN-β-STAT3-dependent pathway. FASEB J. 2018, 32, 1468–1478. [Google Scholar] [CrossRef]
- Zhang, X.; Li, X.; Li, X.; Zheng, L.; Lei, L. ANXA1 silencing increases the sensitivity of cancer cells to low-concentration arsenic trioxide treatment by inhibiting ERK MAPK activation. Tumori. J. 2015, 101, 360–367. [Google Scholar] [CrossRef]
- Canacik, O.; Sabirli, R.; Altintas, E.; Karsli, E.; Karis, D.; Kaymaz, B.; Sabirli, G.T.; Kurt, Ö.; Koseler, A. Annexin A1 as a potential prognostic biomarker for COVID-19 disease: Case–control study. Int. J. Clin. Pract. 2021, 75, e14606. [Google Scholar] [CrossRef]
- Busch, M.H.; Timmermans, S.A.M.E.G.; Aendekerk, J.P.; Ysermans, R.; Amiral, J.; Damoiseaux, J.G.M.C.; Reutelingsperger, C.P.; van Paassen, P. Annexin A1 Is Associated with Adverse Clinical Outcomes in Patients with COVID-19. J. Clin. Med. 2022, 11, 7486. [Google Scholar] [CrossRef]
- Arora, S.; Lim, W.; Bist, P.; Perumalsamy, R.; Lukman, H.M.; Li, F.; Welker, L.B.; Yan, B.; Sethi, G.; Tambyah, P.A.; et al. Influenza A virus enhances its propagation through the modulation of Annexin-A1 dependent endosomal trafficking and apoptosis. Cell Death Differ. 2016, 23, 1243–1256. [Google Scholar] [CrossRef]
- Rahman, F.; Chebbo, M.; Courtin, N.; Fotso, A.F.; Alessi, M.-C.; Riteau, B. The Annexin A1 Receptor FPR2 Regulates the Endosomal Export of Influenza Virus. Int. J. Mol. Sci. 2018, 19, 1400. [Google Scholar] [CrossRef]
- Molás, R.B.; Ribeiro, M.R.; Ramalho Dos Santos, M.J.C.; Borbely, A.U.; Oliani, D.V.; Oliani, A.H.; Nadkarni, S.; Nogueira, M.L.; Moreli, J.B.; Oliani, S.M. The involvement of annexin A1 in human placental response to maternal Zika virus infection. Antivir. Res. 2020, 179, 104809. [Google Scholar] [CrossRef]
- Hiramoto, H.; Dansako, H.; Takeda, M.; Satoh, S.; Wakita, T.; Ikeda, M.; Kato, N. Annexin A1 negatively regulates viral RNA replication of hepatitis C virus. Acta Med. Okayama 2015, 69, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Calmon, M.F.; Mota, M.T.; Babeto, É.; Candido, N.M.; Girol, A.P.; Mendiburu, C.F.; Bonilha, J.L.; Silvestre, R.V.D.; Rosa, B.M.; Thome, J.A.; et al. Overexpression of ANXA1 in penile carcinomas positive for high-risk HPVs. PLoS ONE 2013, 8, e53260. [Google Scholar] [CrossRef] [PubMed]
- Queiroz, C.J.; Nakata, C.M.; Solito, E.; Damazo, A.S. Relationship between HPV and the biomarkers annexin A1 and p53 in oropharyngeal cancer. Infect. Agents Cancer 2014, 9, 13. [Google Scholar] [CrossRef]
- Sena, A.A.; Glavan, T.; Jiang, G.; Sankaran-Walters, S.; Grishina, I.; Dandekar, S.; Goulart, L.R. Divergent Annexin A1 expression in periphery and gut is associated with systemic immune activation and impaired gut immune response during SIV infection. Sci. Rep. 2016, 6, 31157. [Google Scholar] [CrossRef] [PubMed]
- Nedellec, R.; Coetzer, M.; Shimizu, N.; Hoshino, H.; Polonis, V.R.; Morris, L.; Mårtensson, U.E.A.; Binley, J.; Overbaugh, J.; Mosier, D.E. Virus entry via the alternative coreceptors CCR3 and FPRL1 differs by human immunodeficiency virus type 1 subtype. J. Virol. 2009, 83, 8353–8363. [Google Scholar] [CrossRef]
- Jiang, C.; Parrish, N.F.; Wilen, C.B.; Li, H.; Chen, Y.; Pavlicek, J.W.; Berg, A.; Lu, X.; Song, H.; Tilton, J.C.; et al. Primary infection by a human immunodeficiency virus with atypical coreceptor tropism. J. Virol. 2011, 85, 10669–10681. [Google Scholar] [CrossRef] [PubMed]
- Cashin, K.; Jakobsen, M.R.; Sterjovski, J.; Roche, M.; Ellett, A.; Flynn, J.K.; Borm, K.; Gouillou, M.; Churchill, M.J.; Gorry, P.R. Linkages between HIV-1 specificity for CCR5 or CXCR4 and in vitrousage of alternative coreceptors during progressive HIV-1 subtype C infection. Retrovirology 2013, 10, 98. [Google Scholar] [CrossRef]
- Shimizu, N.; Tanaka, A.; Oue, A.; Mori, T.; Apichartpiyakul, C.; Hoshino, H. A short amino acid sequence containing tyrosine in the N-terminal region of G protein-coupled receptors is critical for their potential use as co-receptors for human and simian immunodeficiency viruses. J. Gen. Virol. 2008, 89, 3126–3136. [Google Scholar] [CrossRef]
- Santana, B.B.; Queiroz, M.A.F.; Cerveira, R.A.; Rodrigues, C.M.; Amoras, E.D.S.G.; da Costa, C.A.; de Sousa, M.S.; Ishak, R.; Goulart, L.R.; Vallinoto, A.C.R. Low Annexin A1 level in HTLV-1 infected patients is a potential biomarker for the clinical progression and diagnosis of HAM/TSP. BMC Infect. Dis. 2021, 21, 219. [Google Scholar] [CrossRef] [PubMed]
- Del Valle, D.M.; Kim-Schulze, S.; Huang, H.H.; Beckmann, N.D.; Nirenberg, S.; Wang, B.; Lavin, Y.; Swartz, T.H.; Madduri, D.; Stock, A.; et al. An inflammatory cytokine signature predicts COVID-19 severity and survival. Nat. Med. 2020, 26, 1636–1643. [Google Scholar] [CrossRef]
- Msemburi, W.; Karlinsky, A.; Knutson, V.; Aleshin-Guendel, S.; Chatterji, S.; Wakefield, J. The WHO estimates of excess mortality associated with the COVID-19 pandemic. Nature 2023, 613, 130–137. [Google Scholar] [CrossRef]
- Zhou, Y.; Fu, B.; Zheng, X.; Wang, D.; Zhao, C.; Qi, Y.; Sun, R.; Tian, Z.; Xu, X.; Wei, H. Pathogenic T-cells and inflammatory monocytes incite inflammatory storms in severe COVID-19 patients. Natl. Sci. Rev. 2020, 7, 998–1002. [Google Scholar] [CrossRef]
- Liu, Y.; Zhang, C.; Huang, F.; Yang, Y.; Wang, F.; Yuan, J.; Zhang, Z.; Qin, Y.; Li, X.; Zhao, D.; et al. Elevated plasma levels of selective cytokines in COVID-19 patients reflect viral load and lung injury. Natl. Sci. Rev. 2020, 7, 1003–1011. [Google Scholar] [CrossRef] [PubMed]
- Caricchio, R.; Gallucci, M.; Dass, C.; Zhang, X.; Gallucci, S.; Fleece, D.; Bromberg, M.; Criner, G.J. Preliminary predictive criteria for COVID-19 cytokine storm. Ann. Rheum. Dis. 2021, 80, 88–95. [Google Scholar] [CrossRef] [PubMed]
- Webb, B.J.; Peltan, I.D.; Jensen, P.; Hoda, D.; Hunter, B.; Silver, A.; Starr, N.; Buckel, W.; Grisel, N.; Hummel, E.; et al. Clinical criteria for COVID-19-associated hyperinflammatory syndrome: A cohort study. Lancet Rheumatol. 2020, 2, e754–e763. [Google Scholar] [CrossRef]
- Corral-Gudino, L.; Bahamonde, A.; Arnaiz-Revillas, F.; Gómez-Barquero, J.; Abadía-Otero, J.; García-Ibarbia, C.; Mora, V.; Cerezo-Hernández, A.; Hernández, J.L.; López-Muñíz, G.; et al. Methylprednisolone in adults hospitalized with COVID-19 pneumonia: An open-label randomized trial (GLUCOCOVID). Wien. Klin. Wochenschr. 2021, 133, 303–311. [Google Scholar] [CrossRef]
- RECOVERY Collaborative Group; Horby, P.; Lim, W.S.; Emberson, R.J.; Mafham, M.; Bell, L.J.; Linsell, L.; Staplin, N.; Brightling, C.; Ustianowski, A.; et al. Dexamethasone in Hospitalized Patients with Covid-19. N. Engl. J. Med. 2021, 384, 693–704. [Google Scholar] [CrossRef]
- Vital, S.A.; Senchenkova, E.Y.; Ansari, J.; Gavins, F.N.E. Targeting AnxA1/Formyl Peptide Receptor 2 Pathway Affords Protection against Pathological Thrombo-Inflammation. Cells 2020, 9, 2473. [Google Scholar] [CrossRef] [PubMed]
- Ural, O.; Kıratlı, H.E.; Sümer, Ş.; Demir, N.A.; Kırık, S.Y.; Vatansev, H.; Akyürek, F.; Cebeci, H.; Arslan, U.; Demir, L.S. COVID-19 Tanısıyla Takip Edilen Hastalarda Annexin-1 (ANXA-1), Annexin-2 (ANXA-2) ve Kemik Morfogenetik Protein-7 (BMP-7) Serum Düzeyinin Değerlendirilmesi [Evaluation of Annexin-1 (ANXA-1), Annexin-2 (ANXA-2) and Bone Morpho-genetic Protein-7 (BMP-7) Serum Levels in Patients Followed Up With A Diagnosis of COVID-19]. Mikrobiyol. Bul. 2022, 56, 25–35. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, A.D.; Weinberg, S.E.; Swaminathan, S.; Chaudhuri, S.; Mubarak, H.F.; Schipma, M.J.; Mao, C.; Wang, X.; El-Shennawy, L.; Dashzeveg, N.K.; et al. Unique molecular signatures sustained in circulating monocytes and reg-ulatory T cells in Convalescent COVID-19 patients. bioRxiv 2022. [Google Scholar] [CrossRef]
- Bonavita, A.G. Ac2-26 mimetic peptide of annexin A1 to treat severe COVID-19: A hypothesis. Med. Hypotheses 2020, 145, 110352. [Google Scholar] [CrossRef] [PubMed]
- Neumann, G.; Noda, T.; Kawaoka, Y. Emergence and pandemic potential of swine-origin H1N1 influenza virus. Nature 2009, 459, 931–939. [Google Scholar] [CrossRef]
- Ni, C.; Gao, S.; Zheng, Y.; Liu, P.; Zhai, Y.; Huang, W.; Jiang, H.; Lv, Q.; Kong, D.; Jiang, Y. Annexin A1 Attenuates Neutrophil Migration and IL-6 Expression through Fpr2 in a Mouse Model of Streptococcus suis-Induced Meningitis. Infect. Immun. 2021, 89, e00680-20. [Google Scholar] [CrossRef]
- Cui, J.; Morgan, D.; Cheng, D.H.; Foo, S.L.; Yap, G.L.R.; Ampomah, P.B.; Arora, S.; Sachaphibulkij, K.; Periaswamy, B.; Fairhurst, A.-M.; et al. RNA-Sequencing-Based Transcriptomic Analysis Reveals a Role for Annexin-A1 in Classical and Influenza A Virus-Induced Autophagy. Cells 2020, 9, 1399. [Google Scholar] [CrossRef]
- Courtin, N.; Fotso, A.F.; Fautrad, P.; Mas, F.; Alessi, M.-C.; Riteau, B. Antiviral activity of formyl peptide receptor 2 antagonists against influenza viruses. Antivir. Res. 2017, 143, 252–261. [Google Scholar] [CrossRef]
- Hossain, S.; Choudhury, M.R.; Islam, M.A.; Hassan, M.; Yeasmin, S.; Hossain, F.; Zaman, M.M. Post-chikungunya arthritis: A longitudinal study in a tertiary care hospital in Bangladesh. Trop. Med. Health 2022, 50, 21. [Google Scholar] [CrossRef]
- Cunha, M.S.; de Moura Coletti, T.; Guerra, J.M.; Ponce, C.C.; Fernandes, N.C.C.A.; Résio, R.A.; Claro, I.M.; Salles, F.; Neto, D.F.L.; Sabino, E. A fatal case of dengue hemorrhagic fever associated with dengue virus 4 (DENV-4) in Brazil: Genomic and histopathological findings. Braz. J. Microbiol. 2022, 53, 1305–1312. [Google Scholar] [CrossRef]
- Cavalcante, T.B.; Ribeiro, M.R.C.; Sousa, P.D.S.; Costa, E.D.P.F.; Alves, M.T.S.S.D.B.E.; Simões, V.M.F.; Batista, R.F.L.; Takahasi, E.H.M.; Amaral, G.A.; Khouri, R.; et al. Congenital Zika syndrome: Growth, clinical, and motor development outcomes up to 36 months of age and differences according to microcephaly at birth. Int. J. Infect. Dis. 2021, 105, 399–408. [Google Scholar] [CrossRef] [PubMed]
- Cirino, G.; Flower, R.J.; Browning, J.L.; Sinclair, L.K.; Pepinsky, R.B. Recombinant human lipocortin 1 inhibits thromboxane release from guinea-pig isolated perfused lung. Nature 1987, 328, 270–272. [Google Scholar] [CrossRef] [PubMed]
- Puttamallesh, V.N.; Sreenivasamurthy, S.K.; Singh, P.K.; Harsha, H.C.; Ganjiwale, A.; Broor, S.; Pandey, A.; Narayana, J.; Prasad, T.S.K. Proteomic profiling of serum samples from chikungunya-infected patients provides insights into host response. Clin. Proteom. 2013, 10, 14. [Google Scholar] [CrossRef] [PubMed]
- Galvão, I.; de Carvalho, R.V.H.; Vago, J.P.; Silva, A.L.N.; Carvalho, T.G.; Antunes, M.M.; Ribeiro, F.; Menezes, G.B.; Zamboni, D.; Sousa, L.P.; et al. The role of annexin A1 in the modulation of the NLRP3 inflammasome. Immunology 2020, 160, 78–89. [Google Scholar] [CrossRef]
- Polaris Observatory HCV Collaborators. Global change in hepatitis C virus prevalence and cascade of care between 2015 and 2020: A modelling study. Lancet Gastroenterol. Hepatol. 2022, 7, 396–415. [Google Scholar] [CrossRef]
- Sejima, H.; Mori, K.; Ariumi, Y.; Ikeda, M.; Kato, N. Identification of host genes showing differential expression profiles with cell-based long-term replication of hepatitis C virus RNA. Virus Res. 2012, 167, 74–85. [Google Scholar] [CrossRef]
- Lehtinen, M.; Pimenoff, V.N.; Nedjai, B.; Louvanto, K.; Verhoef, L.; Heideman, D.A.M.; El-Zein, M.; Widschwendter, M.; Dillner, J. Assessing the risk of cervical neoplasia in the post-HPV vaccination era. Int. J. Cancer 2023, 152, 1060–1068. [Google Scholar] [CrossRef]
- Zawacka-Pankau, J.E. The Role of p53 Family in Cancer. Cancers 2022, 14, 823. [Google Scholar] [CrossRef]
- Kastenhuber, E.R.; Lowe, S.W. Putting p53 in Context. Cell 2017, 170, 1062–1078. [Google Scholar] [CrossRef]
- Huibregtse, J.M.; Scheffner, M.; Howley, P.M. Cloning and expression of the cDNA for E6-AP, a protein that mediates the interaction of the human papillomavirus E6 oncoprotein with p53. Mol. Cell. Biol. 1993, 13, 775–784. [Google Scholar] [CrossRef]
- Schiffman, M.; Doorbar, J.; Wentzensen, N.; de Sanjosé, S.; Fakhry, C.; Monk, B.J.; Stanley, M.A.; Franceschi, S. Carcinogenic human papillomavirus infection. Nat. Rev. Dis. Prim. 2016, 2, 16086. [Google Scholar] [CrossRef]
- Calmon, M.F.; Sichero, L.; Boccardo, E.; Villa, L.L.; Rahal, P. HPV16 E6 regulates annexin 1 (ANXA1) protein expression in cervical carcinoma cell lines. Virology 2016, 496, 35–41. [Google Scholar] [CrossRef]
- Mellors, J.W.; Rinaldo, C.R., Jr.; Gupta, P.; White, R.M.; Todd, J.A.; Kingsley, L.A. Prognosis in HIV-1 infection predicted by the quantity of virus in plasma. Science 1996, 272, 1167–1170, Erratum in Science 1997, 275, 14. [Google Scholar] [CrossRef] [PubMed]
- Veazey, R.S.; Lackner, A.A. Getting to the guts of HIV pathogenesis. J. Exp. Med. 2004, 200, 697–700. [Google Scholar] [CrossRef]
- Bookstaver, P.B.; Mohorn, P.L.; Shah, A.; Tesh, L.D.; Quidley, A.M.; Kothari, R.; Bland, C.; Weissman, S. Management of Viral Central Nervous System Infections: A Primer for Clinicians. J. Cent. Nerv. Syst. Dis. 2017, 9, 1179573517703342. [Google Scholar] [CrossRef] [PubMed]
- Huang, P.; Zhou, Y.; Liu, Z.; Zhang, P. Interaction between ANXA1 and GATA-3 in Immunosuppression of CD4+ T Cells. Mediat. Inflamm. 2016, 2016, 1701059. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.H.; Song, W.; Deane, J.A.; Kao, W.; Ooi, J.D.; Ngo, D.; Kitching, A.R.; Morand, E.F.; Hickey, M.J. Deficiency of annexin A1 in CD4+ T cells exacerbates T cell-dependent inflammation. J. Immunol. 2013, 190, 997–1007. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Yoshihara, E.; Son, A.; Matsuo, Y.; Masutani, H.; Sugie, K.; Maeda, M.; Yodoi, J. Differential roles of Annexin A1 (ANXA1/lipocortin-1/lipomodulin) and thioredoxin binding protein-2 (TBP-2/VDUP1/TXNIP) in glucocorticoid signaling of HTLV-I-transformed T cells. Immunol. Lett. 2010, 131, 11–18. [Google Scholar] [CrossRef]
- Fan, Y.; Wei, C.; Xiao, W.; Zhang, W.; Wang, N.; Chuang, P.Y.; He, J.C. Temporal profile of the renal transcriptome of HIV-1 transgenic mice during disease progression. PLoS ONE 2014, 9, e93019. [Google Scholar] [CrossRef]
- Ciechonska, M.; Key, T.; Duncan, R. Efficient reovirus- and measles virus-mediated pore expansion during syncytium formation is dependent on annexin A1 and intracellular calcium. J. Virol. 2014, 88, 6137–6147. [Google Scholar] [CrossRef]
- Ma, X.; Zhang, K.; Luo, Z.; Nian, X.; Choudhury, S.K.M.; Zhu, Z.; Song, R.; Pei, J.; Huo, Y.; Li, Y.; et al. FMDV 3A Antagonizes the Effect of ANXA1 to Positively Modulate Viral Replication. J. Virol. 2022, 96, e0031722. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Huang, L.; Zhao, W.; Rigas, B. Annexin 1 induced by anti-inflammatory drugs binds to NF-kappaB and inhibits its activation: Anticancer effects in vitro and in vivo. Cancer Res. 2010, 70, 2379–2388. [Google Scholar] [CrossRef] [PubMed]
| |||
|---|---|---|---|
| Virus | In Vivo (Model); In Vitro (Cell Type) | Comment | Reference |
| SARS-CoV-2 (COVID-19) | Case-control study with analysis of clinic-based blood samples | Lower AnxA1 levels were found in the severe/critical disease group compared with the control and moderate disease groups | [89] |
| Prospective cohort study with analysis of clinic-based blood samples | Elevated levels of AnxA1 were observed in cases of moderate and severe disease | [90] | |
| Influenza A virus (IAV) | Human epithelial cell line (A549) or MDCK cells; C57BL/6 (WT mice) | Activation of FPR2 stimulated viral replication through an ERK-dependent pathway, resulting in reduced survival in mice | [85] |
| AnxA1-KO and WT mice; A549 cells | AnxA1 increased viral replication, affected virus binding, and promoted the trafficking of endosomal viruses to the nucleus | [91] | |
| A549 cells | The blocking of FPR2 signaling inhibited viral replication and interfered with the endosomal trafficking of IAV | [92] | |
| C57BL/6 (WT) mice; samples: lungs of mice | The activation of the AnxA1/FPR2 pathway demonstrated beneficial effects for the host, improving survival, inhibiting viral replication and expanding alveolar macrophages | [19] | |
| A549 cells | AnxA1 plays a regulatory role in RIG-I signaling and induces apoptotic cell death upon infection | [21] | |
| |||
| Virus | In vivo (model); in vitro (cell type) | Comment | Reference |
| Chikungunya (CHIKV) | AnxA1-KO; FPR2-KO and WT mice | The activation of the AnxA1/FPR2 pathway demonstrated beneficial effects for the host by reducing the inflammatory response | [26] |
| Dengue virus (DENV) | AnxA1-KO; FPR2-KO; A129, and WT mice | The activation of the AnxA1/FPR2 pathway demonstrated beneficial effects for the host | [24] |
| Zika virus (ZIKV) | Cross-sectional study with analysis of clinic-based samples: placental fragments of pregnant women with suspected Zika virus infection | AnxA1 is involved in modulating inflammation in response to ZIKV infection | [93] |
| Hepatitis C virus (HCV) | Human hepatoma cell line Li23 and Li23-derived D7 cells | AnxA1 negatively regulates the step of viral RNA replication, but does not regulate viral entry | [94] |
| Human papillomavirus (HPV) | Analysis of clinic-based samples: tissue sections from penile squamous cell carcinoma | AnxA1 is overexpressed in high-risk HPV-positive penile carcinoma patients | [95] |
| Analysis of clinic-based samples: tumor and adjacent mucosa from patients with squamous cell carcinoma of the oropharynx | Increased expression of AnxA1 in HPV+ samples suggests that the protein is involved in the early stages of HPV-driven carcinogenesis | [96] | |
| Simian immunodeficiency virus (SIV) | Rhesus macaques | During early stages of infection, AnxA1 expression decreased in the gut and increased in the blood, while during chronic infection, AnxA1 expression increased in both compartments | [97] |
| Human immunodefiency virus (HIV) | NP-2 cells; C8166 cells; T CD4+ cells obtained from human donors | HIV strains used FPR2 efficiently as a co-receptor; 22 envelope proteins can bind to FPR2 | [98,99,100,101] |
| Herpes simplex virus 1 (HSV-1) | AnxA1-KO and WT mice; A549 cells | Similar to IAV, viral particles of HSV-1 hijack the AnxA1/FPR2 pathway to increase endocytosis by the cells via FPR2 receptor | [20] |
| Human T-lymphotropic virus 1 (HTLV-1) | Analysis of clinic-based samples: blood | An imbalance in the expression of ANXA1 may contribute to the development of chronic neurodegenerative diseases caused by HTLV-1 | [102] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Resende, F.; Araújo, S.d.; Tavares, L.P.; Teixeira, M.M.; Costa, V.V. The Multifaceted Role of Annexin A1 in Viral Infections. Cells 2023, 12, 1131. https://doi.org/10.3390/cells12081131
Resende F, Araújo Sd, Tavares LP, Teixeira MM, Costa VV. The Multifaceted Role of Annexin A1 in Viral Infections. Cells. 2023; 12(8):1131. https://doi.org/10.3390/cells12081131
Chicago/Turabian StyleResende, Filipe, Simone de Araújo, Luciana Pádua Tavares, Mauro Martins Teixeira, and Vivian Vasconcelos Costa. 2023. "The Multifaceted Role of Annexin A1 in Viral Infections" Cells 12, no. 8: 1131. https://doi.org/10.3390/cells12081131






