No-Cap Flowable Bulk-Fill Composite: Physico-Mechanical Assessment
Abstract
:1. Introduction
2. Materials and Methods
2.1. Flexural Strength Evaluation
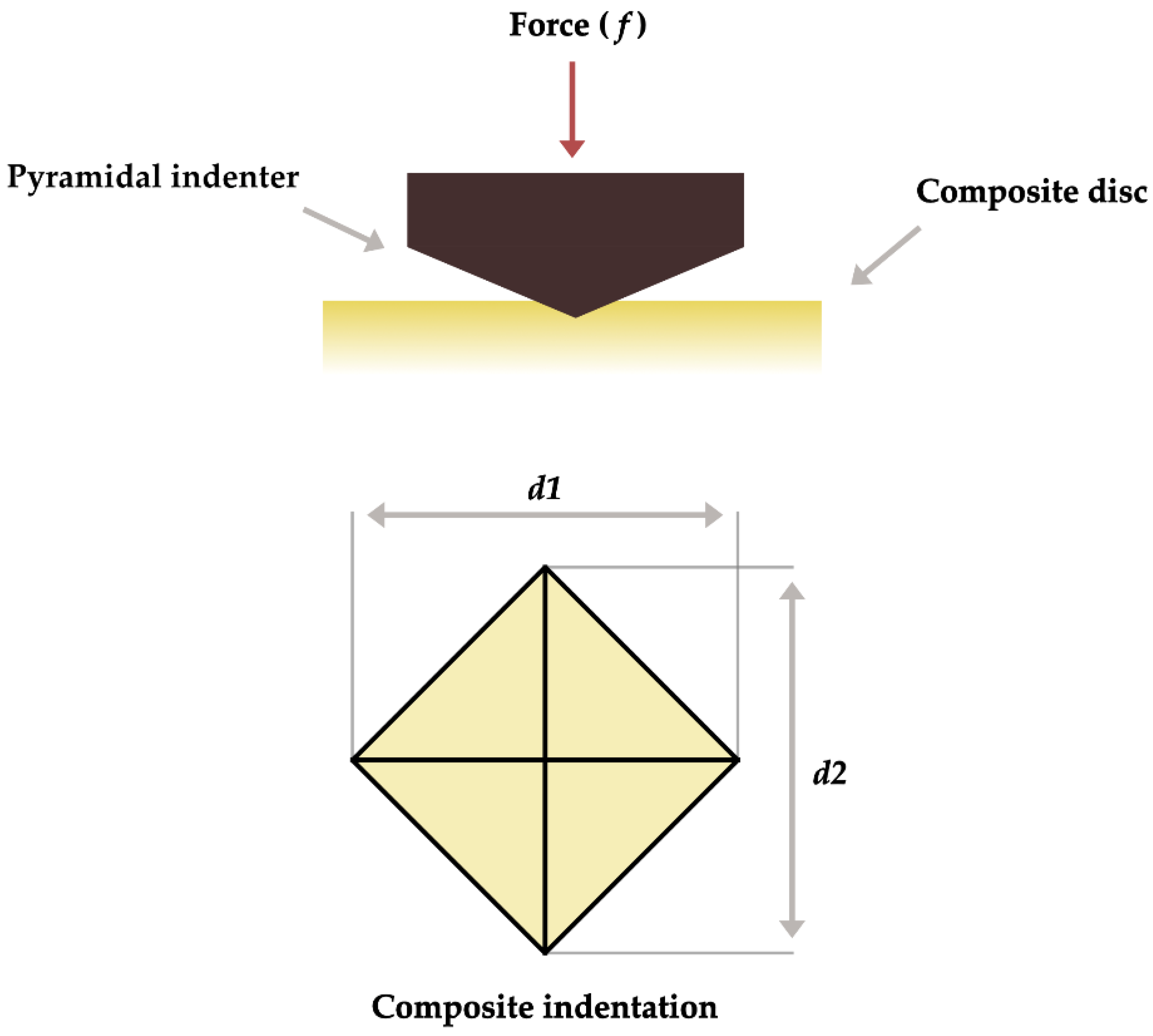
2.2. Vicker’s Microhardness (VMH) Evaluation
2.3. Surface Roughness (Ra) Evaluation
2.4. Assessment of Color Change
2.5. Statistical Analysis
3. Results
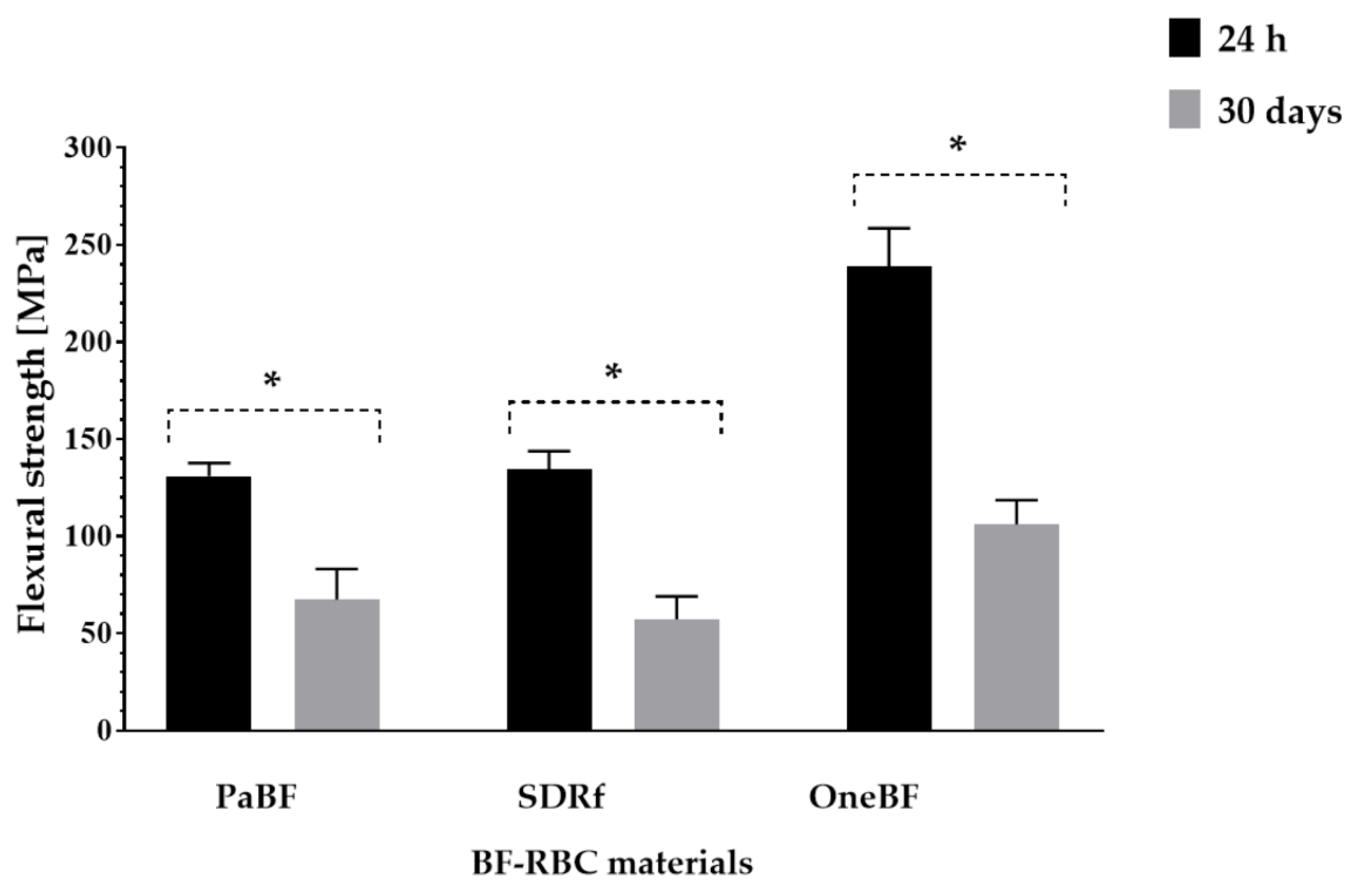
3.1. Flexural Strength
3.2. Vicker’s Microhardness (VMH)
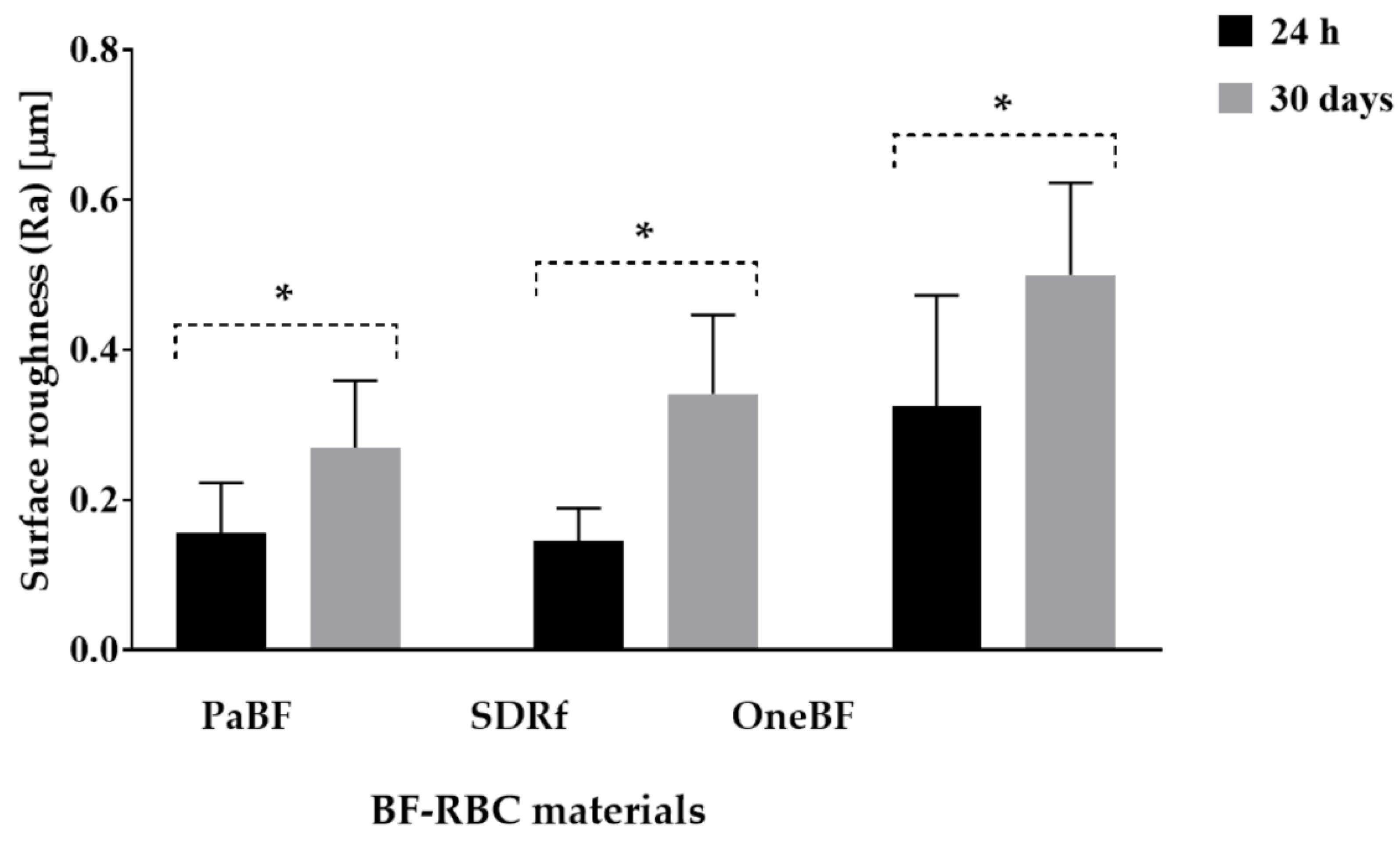
3.3. Surface Roughness (Ra)
3.4. Color Change
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Lynch, C.D.; Opdam, N.J.; Hickel, R.; Brunton, P.A.; Gurgan, S.; Kakaboura, A.; Shearer, A.C.; Vanherle, G.; Wilson, N.H. Guidance on posterior resin composites: Academy of Operative Dentistry-European Section. J. Dent. 2014, 42, 377–383. [Google Scholar] [CrossRef] [PubMed]
- Yadav, R.; Kumar, M. Dental restorative composite materials: A review. J. Oral Biosci. 2019, 61, 78–83. [Google Scholar] [CrossRef]
- Abbasi, M.; Moradi, Z.; Mirzaei, M.; Kharazifard, M.J.; Rezaei, S. Polymerization Shrinkage of Five Bulk-Fill Composite Resins in Comparison with a Conventional Composite Resin. J. Dent. 2018, 15, 365–374. [Google Scholar] [CrossRef]
- Parasher, A.; Ginjupalli, K.; Somayaji, K.; Kabbinale, P. Comparative evaluation of the depth of cure and surface roughness of bulk-fill composites: An in vitro study. Dent. Med. Probl. 2020, 57, 39–44. [Google Scholar] [CrossRef]
- Grazioli, G.; Cuevas-Suárez, C.E.; Nakanishi, L.; Francia, A.; de Moraes, R.R. Physicochemical characterization of two bulk fill composites at different depths. Restor. Dent. Endod. 2021, 46, e39. [Google Scholar] [CrossRef]
- de Camargo, E.J.; Moreschi, E.; Baseggio, W.; Cury, J.A.; Pascotto, R.C. Composite depth of cure using four polymerization techniques. J. Appl. Oral Sci. 2009, 17, 446–450. [Google Scholar] [CrossRef] [PubMed]
- Reis, A.F.; Vestphal, M.; Amaral, R.C.D.; Rodrigues, J.A.; Roulet, J.F.; Roscoe, M.G. Efficiency of polymerization of bulk-fill composite resins: A systematic review. Braz. Oral Res. 2017, 31, e59. [Google Scholar] [CrossRef] [Green Version]
- Haugen, H.J.; Marovic, D.; Par, M.; Thieu, M.K.L.; Reseland, J.E.; Johnsen, G.F. Bulk Fill Composites Have Similar Performance to Conventional Dental Composites. Int. J. Mol. Sci. 2020, 21, 5136. [Google Scholar] [CrossRef] [PubMed]
- Tomaszewska, I.M.; Kearns, J.O.; Ilie, N.; Fleming, G.J. Bulk fill restoratives: To cap or not to cap--that is the question? J. Dent. 2015, 43, 309–316. [Google Scholar] [CrossRef] [PubMed]
- Bollen, C.M.; Lambrechts, P.; Quirynen, M. Comparison of surface roughness of oral hard materials to the threshold surface roughness for bacterial plaque retention: A review of the literature. Dent. Mater. 1997, 13, 258–269. [Google Scholar] [CrossRef]
- Paolone, G.; Formiga, S.; De Palma, F.; Abbruzzese, L.; Chirico, L.; Scolavino, S.; Goracci, C.; Cantatore, G.; Vichi, A. Color stability of resin-based composites: Staining procedures with liquids-A narrative review. J. Esthet. Restor. Dent. 2022, 34, 865–887. [Google Scholar] [CrossRef]
- Quek, S.H.Q.; Yap, A.U.J.; Rosa, V.; Tan, K.B.C.; Teoh, K.H. Effect of staining beverages on color and translucency of CAD/CAM composites. J. Esthet. Restor. Dent. 2018, 30, E9–E17. [Google Scholar] [CrossRef]
- Sarafianou, A.; Iosifidou, S.; Papadopoulos, T.; Eliades, G. Color stability and degree of cure of direct composite restoratives after accelerated aging. Oper. Dent. 2007, 32, 406–411. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- PALFIQUE® BULK FLOW Technical Report. Available online: http://www.tokuyama-dental.com/tdc/pdf/technicalreport/PALFIQUE_BULK_FLOW_technical_report_ver1.pdf (accessed on 25 June 2022).
- Algamaiah, H.; Watts, D.C. Post-irradiation surface viscoelastic integrity of photo-polymerized resin-based composites. Dent. Mater. 2021, 37, 1828–1833. [Google Scholar] [CrossRef]
- Ilie, N.; Hickel, R. Investigations on a methacrylate-based flowable composite based on the SDR™ technology. Dent. Mater. 2011, 27, 348–355. [Google Scholar] [CrossRef] [PubMed]
- Gan, J.K.; Yap, A.U.; Cheong, J.W.; Arista, N.; Tan, C. Bulk-Fill Composites: Effectiveness of Cure With Poly- and Monowave Curing Lights and Modes. Oper. Dent. 2018, 43, 136–143. [Google Scholar] [CrossRef] [PubMed]
- Miletic, V.; Marjanovic, J.; Veljovic, D.N.; Stasic, J.N.; Petrovic, V. Color stability of bulk-fill and universal composite restorations with dissimilar dentin replacement materials. J. Esthet. Restor. Dent. 2019, 31, 520–528. [Google Scholar] [CrossRef] [PubMed]
- Marjanovic, J.; Veljovic, D.N.; Stasic, J.N.; Savic-Stankovic, T.; Trifkovic, B.; Miletic, V. Optical properties of composite restorations influenced by dissimilar dentin restoratives. Dent. Mater. 2018, 34, 737–745. [Google Scholar] [CrossRef] [PubMed]
- Roulet, J.F. Is in vitro research in restorative dentistry useless? J. Adhes. Dent. 2012, 14, 103–104. [Google Scholar] [CrossRef] [PubMed]
- Opdam, N.J.; van de Sande, F.H.; Bronkhorst, E.; Cenci, M.S.; Bottenberg, P.; Pallesen, U.; Gaengler, P.; Lindberg, A.; Huysmans, M.C.; van Dijken, J.W. Longevity of posterior composite restorations: A systematic review and meta-analysis. J. Dent. Res. 2014, 93, 943–949. [Google Scholar] [CrossRef] [Green Version]
- Demarco, F.F.; Corrêa, M.B.; Cenci, M.S.; Moraes, R.R.; Opdam, N.J. Longevity of posterior composite restorations: Not only a matter of materials. Dent. Mater. 2012, 28, 87–101. [Google Scholar] [CrossRef]
- Ilie, N.; Hickel, R. Investigations on mechanical behaviour of dental composites. Clin. Oral Investig. 2009, 13, 427–438. [Google Scholar] [CrossRef]
- Say, E.C.; Civelek, A.; Nobecourt, A.; Ersoy, M.; Guleryuz, C. Wear and microhardness of different resin composite materials. Oper. Dent. 2003, 28, 628–634. [Google Scholar]
- Topcu, F.T.; Erdemir, U.; Sahinkesen, G.; Yildiz, E.; Uslan, I.; Acikel, C. Evaluation of microhardness, surface roughness, and wear behavior of different types of resin composites polymerized with two different light sources. J. Biomed. Mater. Res. B Appl. Biomater. 2010, 92, 470–478. [Google Scholar] [CrossRef] [PubMed]
- Francis, N.; Rajan, R.R.; Kumar, V.; Varughese, A.; Karuveetil, V.; Sapna, C.M. Effect of irradiance from curing units on the microhardness of composite—A systematic review. Evid. Based Dent. 2022. [Google Scholar] [CrossRef]
- Rodrigues Junior, S.A.; Zanchi, C.H.; Carvalho, R.V.; Demarco, F.F. Flexural strength and modulus of elasticity of different types of resin-based composites. Braz. Oral Res. 2007, 21, 16–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Asmussen, E.; Peutzfeldt, A. Influence of UEDMA BisGMA and TEGDMA on selected mechanical properties of experimental resin composites. Dent. Mater. 1998, 14, 51–56. [Google Scholar] [CrossRef]
- 3M Oral Care3M™ Filtek™ One Bulk Fill Restorative Technical Product Profile. Available online: https://multimedia.3m.com/mws/media/1317671O/3m-filtek-one-bulk-fill-restorative-technical-product-profile.pdf&fn=Filtek%20One%20Bulk%20Fill%20Technical%20Product%20Profile_NA_R2.pdf (accessed on 3 May 2022).
- Eweis, A.H.; Yap, A.U.; Yahya, N.A. Comparison of Flexural Properties of Bulk-fill Restorative/Flowable Composites and Their Conventional Counterparts. Oper. Dent. 2020, 45, 41–51. [Google Scholar] [CrossRef] [PubMed]
- Braga, R.R.; Ballester, R.Y.; Ferracane, J.L. Factors involved in the development of polymerization shrinkage stress in resin-composites: A systematic review. Dent. Mater. 2005, 21, 962–970. [Google Scholar] [CrossRef] [PubMed]
- Shah, P.K.; Stansbury, J.W.; Bowman, C.N. Application of an addition–fragmentation-chain transfer monomer in di (meth) acrylate network formation to reduce polymerization shrinkage stress. Polym. Chem. 2017, 8, 4339–4351. [Google Scholar] [CrossRef] [PubMed]
- Hasanain, F.A.; Nassar, H.M.; Ajaj, R.A. Effect of Light Curing Distance on Microhardness Profiles of Bulk-Fill Resin Composites. Polymers 2022, 14, 528. [Google Scholar] [CrossRef] [PubMed]
- Yeo, H.W.; Loo, M.Y.; Alkhabaz, M.; Li, K.C.; Choi, J.J.E.; Barazanchi, A. Bulk-Fill Direct Restorative Materials: An In Vitro Assessment of Their Physio-Mechanical Properties. Oral 2021, 1, 75–87. [Google Scholar] [CrossRef]
- Paravina, R.D.; Roeder, L.; Lu, H.; Vogel, K.; Powers, J.M. Effect of finishing and polishing procedures on surface roughness, gloss and color of resin-based composites. Am. J. Dent. 2004, 17, 262–266. [Google Scholar]
- Park, J.W.; Song, C.W.; Jung, J.H.; Ahn, S.J.; Ferracane, J.L. The effects of surface roughness of composite resin on biofilm formation of Streptococcus mutans in the presence of saliva. Oper. Dent. 2012, 37, 532–539. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rigo, L.C.; Bordin, D.; Fardin, V.P.; Coelho, P.G.; Bromage, T.G.; Reis, A.; Hirata, R. Influence of Polishing System on the Surface Roughness of Flowable and Regular-Viscosity Bulk Fill Composites. Int. J. Periodontics Restor. Dent. 2018, 38, e79–e86. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hassan, A.M.; Nabih, S.M.; Mossa, H.M.; Baroudi, K. The effect of three polishing systems on surface roughness of flowable, microhybrid, and packable resin composites. J. Int. Soc. Prev. Community Dent. 2015, 5, 242–247. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lu, H.; Roeder, L.B.; Lei, L.; Powers, J.M. Effect of surface roughness on stain resistance of dental resin composites. J. Esthet. Restor. Dent. 2005, 17, 102–108, discussion 109. [Google Scholar] [CrossRef] [PubMed]
- Shamszadeh, S.; Sheikh-Al-Eslamian, S.M.; Hasani, E.; Abrandabadi, A.N.; Panahandeh, N. Color Stability of the Bulk-Fill Composite Resins with Different Thickness in Response to Coffee/Water Immersion. Int. J. Dent. 2016, 2016, 7186140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, B.; Lee, Y.K. Comparison of the color stability of flowable and universal resin composites. Am. J. Dent. 2009, 22, 160–164. [Google Scholar]

| Material (Manufacturer) | Code | Composition | Filler Load wt%/vol%. |
|---|---|---|---|
| Palfique Bulk flow (Tokuyama Dental, Tokyo, Japan) | PaBF | Bis-GMA, TEGDMA, Bis-MPEPP, Mequinol, Dibutyl hydroxyl toluene and UV absorber | 70/56% |
| SDR Flow composite (Dentsply Sirona Charlotte, NC, USA) | SDRf | Modified UDMA, ethoxylated ethoxylated Bisphenol A dimethacrylate, and TEGDMA, resins. The filler is a combination of Bari-um-alumino-fluoro-borosilicate glass and strontium alumino-fluoro-silicate glass | 68/45% |
| One Bulk fill (3M, St. Paul, MN, USA) | OneBF | Zirconia/ silica cluster, itterbium trifluoride, AUDMA, UDMA, DDDMAA, AFM | 76.5/58.5% |
| Group | Flexural Strength (24 h) (Mean ± SD) | Flexural Strength (30 days) (Mean ± SD) | Flexural Strength Loss (%) |
|---|---|---|---|
| PaBF | 130.97 ± 6.71 a | 67.51 ± 15.69 A | 48.45 |
| SDRf | 134.58 ± 9.26 a | 57.23 ± 11.96 A | 57.47 |
| OneBF | 238.82 ± 19.79 b | 106.17 ± 12.40 B | 55.54 |
| Group | VMH (24 h) (Mean ± SD) | VMH (30 days) (Mean ± SD) | Microhardness Loss (%) |
|---|---|---|---|
| PaBF | 36.2750 ± 0.59 a,b | 36.135 ± 0.37 A,B | 0.38 |
| SDRf | 18.45 ± 0.21 a | 18.41 ± 0.18 A | 0.21 |
| OneBF | 65.51 ± 1.40 b | 68.83 ± 2.35 B | −5.06 |
| Group | Surface Roughness (Ra) [μm] (24 h) | Surface Roughness (Ra) [μm] (30 days) | Surface Roughness Increase |
|---|---|---|---|
| PaBF | 0.16 ± 0.07 a | 0.27 ± 0.09 A | 68.75 |
| SDRf | 0.15 ± 0.04 a | 0.34 ± 0.10 A,B | 126.6 |
| OneBF | 0.33 ± 0.15 a | 0.49 ± 0.124 B | 48.48 |
| Group | Color Change (ΔE) |
|---|---|
| PaBF | 20.72 ± 2.565 A,B |
| SDRf | 11.55 ± 2.803 B |
| OneBF | 5.057 ± 1.664 C |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alshehri, A.; Alhalabi, F.; Robaian, A.; Abuelqomsan, M.A.S.; Alshabib, A.; Ismail, E.; Alzamil, F.; Alotaibi, N.; Algamaiah, H. No-Cap Flowable Bulk-Fill Composite: Physico-Mechanical Assessment. Polymers 2023, 15, 1847. https://doi.org/10.3390/polym15081847
Alshehri A, Alhalabi F, Robaian A, Abuelqomsan MAS, Alshabib A, Ismail E, Alzamil F, Alotaibi N, Algamaiah H. No-Cap Flowable Bulk-Fill Composite: Physico-Mechanical Assessment. Polymers. 2023; 15(8):1847. https://doi.org/10.3390/polym15081847
Chicago/Turabian StyleAlshehri, Abdullah, Feras Alhalabi, Ali Robaian, Mohammed A. S. Abuelqomsan, Abdulrahman Alshabib, Eman Ismail, Faisal Alzamil, Nawaf Alotaibi, and Hamad Algamaiah. 2023. "No-Cap Flowable Bulk-Fill Composite: Physico-Mechanical Assessment" Polymers 15, no. 8: 1847. https://doi.org/10.3390/polym15081847







