A Hybrid MCDM Model for Improving the Electronic Health Record to Better Serve Client Needs
Abstract
:1. Introduction
2. Literature Review on EHR and the TOE Framework
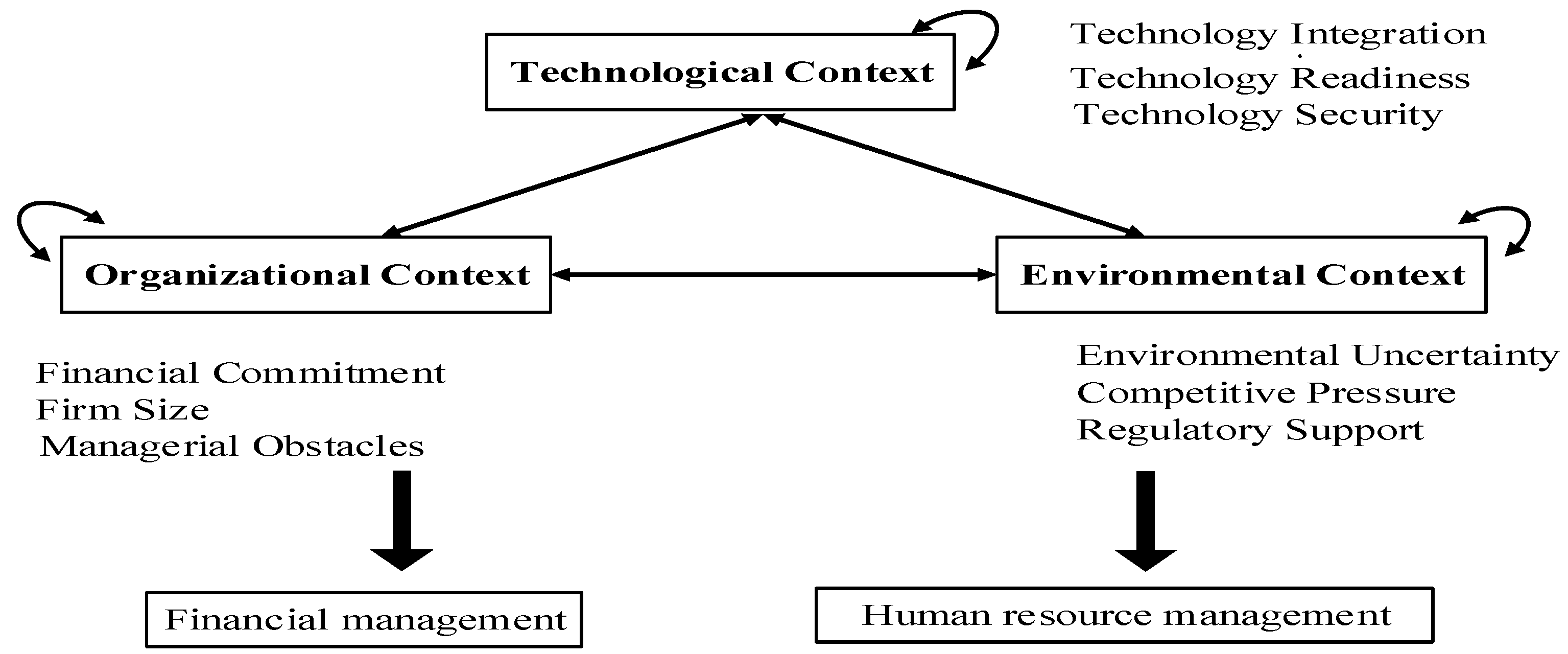
2.1. The TOE Dimensions of EHR
2.2. Technological Dimension
2.3. Organizational Dimension
2.4. Environmental Dimension
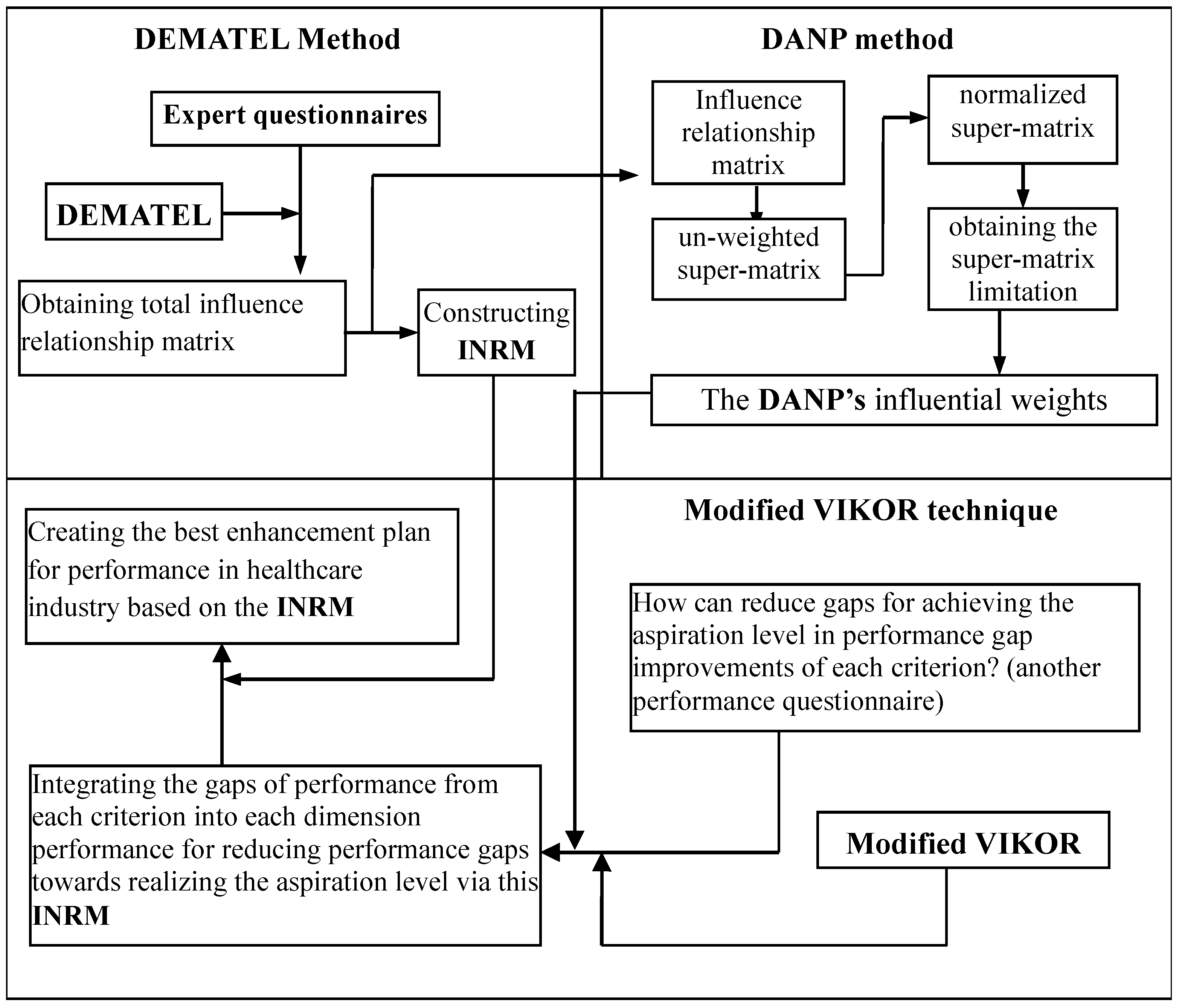
3. Method: DEMATEL-DANP-mVIKOR Model
3.1. DEMATEL Technique
3.2. DANP Technique
3.3. Modified VIKOR
4. Empirical Study: EHR Implementation in the Healthcare Industry
4.1. Description of Data Collection
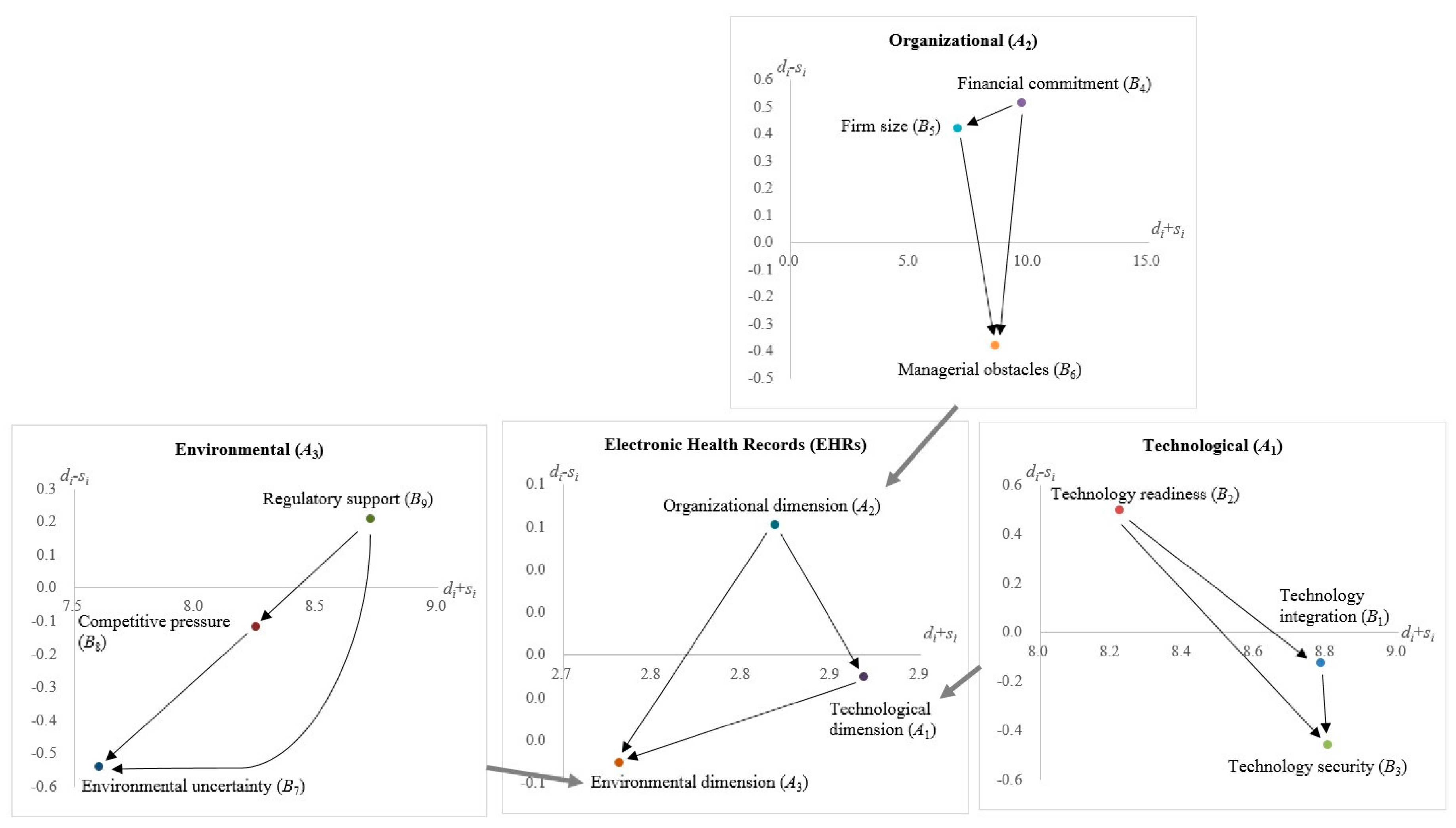
4.2. Assembling the Influence Network via the DEMATEL Method
4.3. Finding the DANP’s Influential Weights
4.4. Integrating/Evaluating the Gaps by the Modified VIKOR Method
4.5. Discussion and Implications
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Heart, T.; Ben-Assuli, O.; Shabtai, I. A review of PHR, EMR and EHR integration: A more personalized healthcare and public health policy. Health Policy Technol. 2017, 6, 20–25. [Google Scholar] [CrossRef]
- Office of the National Coordinator for Health Information Technology (ONC). Defining Key Health Information Technology Terms April 28, 2008. Available online: http://www.hitechanswers.net/wp-content/uploads/2013/05/NAHIT-Definitions2008.pdf (accessed on 30 June 2017).
- Ben-Zion, R.; Pliskin, N.; Fink, L. Critical Success Factor for Adoption of Electronic Health Record Systems: Literature Review and Prescriptive Analysis. Inf. Syst. Manag. 2014, 31, 296–312. [Google Scholar] [CrossRef]
- Miller, A.R.; Tucker, C. Privacy protection and technology diffusion: The case of electronic medical records. Manag. Sci. 2007, 55, 1077–1093. [Google Scholar] [CrossRef]
- Jha, A.; Ferris, T.; Donelan, K.; DesRoches, C.; Shields, A.; Rosenbaum, S.; Blumenthal, D. How common are electronic health records in the United States? A summary of the evidence. Health Aff. 2006, 25, 496–507. [Google Scholar] [CrossRef] [PubMed]
- Miller, R.H.; Sim, I. Physicians’ Use of electronic medical records: Barriers and solutions. Health Aff. 2004, 23, 116–126. [Google Scholar] [CrossRef]
- Behkami, N.A.; Daim, T.U. Research Forecasting for Health Information Technology (HIT), using technology intelligence. Technol. Forecast. Soc. Chang. 2012, 79, 498–508. [Google Scholar] [CrossRef]
- Jones, S.S.; Rudin, R.S.; Perry, T.; Shekelle, P.G. Health information technology: An updated systematic review with a focus on meaningful use. Ann. Intern. Med. 2014, 160, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Shanafelt, T.D.; Dyrbye, L.N.; Sinsky, C.; Hasan, O.; Satele, D.; Sloan, J.; West, C.P. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin. Proc. 2016, 91, 836–848. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, G.S.; Payne, T.H. Selection and Implementation of an Electronic Health Record. PMR 2017, 9, S4–S12. [Google Scholar] [CrossRef] [PubMed]
- Penrod, E.L. Electronic Health Record Transition Considerations. PMR 2017, 9, S13–S18. [Google Scholar] [CrossRef] [PubMed]
- Lau, F.; Price, M.; Boyd, J.; Partridge, C.; Bell, H.; Raworth, R. Impact of electronic medical record on physician practice in office settings: A systematic review. BMC Med. Inform. Decis. Mak. 2012, 12, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Boonstra, A.; Broekhuis, M. Barriers to the acceptance of electronic medical records by physicians from systematic review to taxonomy and interventions. BMC Health Serv. Res. 2010, 10, 231–247. [Google Scholar] [CrossRef] [PubMed]
- Chang, I.C.; Hwang, H.G.; Hung, M.C.; Kuo, K.M.; Yen, D.C. Factor affecting cross-hospital exchange of Electronic Medical Records. Inf. Manag. 2009, 46, 109–115. [Google Scholar] [CrossRef]
- Tornatzky, L.G.; Fleischer, M. The Processes of Technological Innovation; Lexington Books: Lexington, MA, USA, 1990. [Google Scholar]
- Corrocher, N. The diffusion of Internet telephony among consumers and firms: Current issues and future prospects. Technol. Forecast. Soc. Chang. 2003, 70, 525–544. [Google Scholar] [CrossRef]
- Zhu, K.; Kraemer, K.L.; Xu, S.; Dedrick, J. Information technology payoff in e-business environments: An international perspective on value creation of e-business in the financial services industry. J. Manag. Inf. Syst. 2004, 21, 17–54. [Google Scholar] [CrossRef]
- Chau, P.Y.K.; Tam, K.Y. Factor affecting the adoption of open systems: An exploratory study. MIS Q. 1997, 21, 1–24. [Google Scholar] [CrossRef]
- Jeyaraj, A.; Rottman, J.; Lacity, M.J. A review of the predictors, linkages, and biases in IT innovation adoption research. J. Inf. Technol. 2006, 21, 1–23. [Google Scholar] [CrossRef]
- Jia, Q.; Guo, Y.; Barnes, S.J. Enterprise 2.0 post-adoption: Extending the information system continuance model based on the technology-Organization-environment framework. Comput. Hum. Behav. 2017, 67, 95–105. [Google Scholar] [CrossRef]
- He, C.; Fan, X.; Li, Y. Toward ubiquitous healthcare services with a novel efficient cloud platform. IEEE Trans. Biomed. Eng. 2013, 60, 230–234. [Google Scholar] [CrossRef] [PubMed]
- Scheurwegs, E.; Luyckx, K.; Luyten, L.; Daelemans, W.; Vanden Bulcke, T. Data integration of structured and unstructured sources forassigning clinical codes to patient stays. J. Am. Med. Inform. Assoc. 2016, 23, e11–e19. [Google Scholar] [CrossRef] [PubMed]
- Damanpour, F. Organizational size and innovation. Organ. Stud. 1992, 13, 375–402. [Google Scholar] [CrossRef]
- Iacovou, C.L.; Benbasat, I.; Dexter, A.S. Electronic data interchange and small organizations: Adoption and impact of technology. MIS Q. 1995, 19, 465–485. [Google Scholar] [CrossRef]
- Ramamurthy, K.; Premkumar, G.; Crum, M.R. Organizational and interorganizational determinants of EDI diffusion and organizational performance: A cause model. J. Organ. Comput. Electron. Commer. 1999, 9, 253–285. [Google Scholar] [CrossRef]
- Chatterjee, D.; Grewal, R.; Sambamurthy, V. Shaping up for e-commerce: Institutional enablers of the organizational assimilation of Web technologies. MIS Q. 2002, 26, 65–89. [Google Scholar] [CrossRef]
- Zhu, K.; Kraemer, K.L.; Xu, S. The process of innovation assimilation by firms in different countries: A technology diffusion perspective on e-business. Manag. Sci. 2006, 52, 1557–1576. [Google Scholar] [CrossRef]
- Lu, M.T.; Lin, S.W.; Tzeng, G.H. Improving RFID adoption in Taiwan’s healthcare industry based on a DEMATEL technique with a hybrid MCDM model. Decis. Support Syst. 2013, 56, 259–269. [Google Scholar] [CrossRef]
- Mata, F.; Fuerst, W.; Barney, J. Information technology and sustained competitive advantage: A resource-based analysis. MIS Q. 1995, 19, 487–505. [Google Scholar] [CrossRef]
- Duncan, R.B. Characteristics of organizational environments and perceived environmental uncertainty. Adm. Sci. Q. 1972, 17, 313–327. [Google Scholar] [CrossRef]
- Downey, H.K.; Hellriegel, D.; Slocum, J.W. Environmental uncertainty: The construct and its application. Adm. Sci. Q. 1975, 20, 613–629. [Google Scholar] [CrossRef]
- Gatignon, H.; Robertson, T.S. Technology Diffusion: An Empirical Test of Competitive Effects. J. Mark. 1989, 53, 35–49. [Google Scholar] [CrossRef]
- Umanath, N.S.; Campbell, T.L. Differential diffusion of information systems technology in multinational enterprises: A research model. Inf. Resour. Manag. J. 1994, 7, 6–18. [Google Scholar] [CrossRef]
- Hatch, M.J. Organizational Theory Modern, Symbolic, and Postmodern Perspectives; Oxford University Press: Oxford, UK, 1997. [Google Scholar]
- Dasgupta, S.; Agarwal, D.; Ioannidis, A.; Gopalakrishnan, S. Determinants of information technology adoption: An extension of existing models to firms in a developing country. J. Glob. Inf. Manag. 1999, 7, 41–49. [Google Scholar] [CrossRef]
- Ronen, J. Organizational Innovation: The Transaction Cost Approach. In Entrepreneurship; Ronen, J. Lexington Books: Lexington, MA, USA, 1983. [Google Scholar]
- Lu, M.T.; Tzeng, G.H.; Cheng, H.; Hsu, C.C. Exploring mobile banking services for user behavior in intention adoption: Using new hybrid MADM model. Serv. Bus. 2015, 9, 541–565. [Google Scholar] [CrossRef]
- Opricovic, S.; Tzeng, G.H. Extended VIKOR method in comparison with outranking methods. Eur. J. Oper. Res. 2007, 178, 514–529. [Google Scholar] [CrossRef]
- Liou, J.J.H.; Tamošaitienė, J.; Zavadskas, E.K.; Tzeng, G.H. New hybrid COPRAS-G MADM Model for improving and selecting suppliers in green supply chain management. Int. J. Prod. Res. 2016, 54, 114–134. [Google Scholar] [CrossRef]
| Criteria | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Technology integration | 0.421 | 0.466 | 0.534 | 0.533 | 0.381 | 0.538 | 0.463 | 0.517 | 0.477 |
| Technology readiness | 0.513 | 0.366 | 0.559 | 0.538 | 0.365 | 0.522 | 0.492 | 0.482 | 0.522 |
| Technology security | 0.493 | 0.436 | 0.423 | 0.538 | 0.355 | 0.480 | 0.455 | 0.466 | 0.529 |
| Financial commitment | 0.629 | 0.529 | 0.639 | 0.515 | 0.463 | 0.636 | 0.550 | 0.566 | 0.593 |
| Firm size | 0.453 | 0.397 | 0.465 | 0.461 | 0.268 | 0.452 | 0.398 | 0.403 | 0.425 |
| Managerial obstacles | 0.484 | 0.419 | 0.505 | 0.508 | 0.378 | 0.404 | 0.449 | 0.484 | 0.486 |
| Environmental uncertainty | 0.419 | 0.368 | 0.434 | 0.456 | 0.329 | 0.442 | 0.314 | 0.393 | 0.378 |
| Competitive pressure | 0.498 | 0.444 | 0.514 | 0.496 | 0.354 | 0.486 | 0.470 | 0.371 | 0.435 |
| Regulatory support | 0.548 | 0.439 | 0.558 | 0.564 | 0.411 | 0.541 | 0.483 | 0.505 | 0.415 |
| Dimensions | Influence Given | Influence Received | Prominence | Net Effect | |||
|---|---|---|---|---|---|---|---|
| Technological dimension | 0.468 | 0.472 | 0.489 | 1.429 | 1.439 | 2.868 | −0.010 |
| Organizational dimension | 0.502 | 0.454 | 0.484 | 1.440 | 1.379 | 2.819 | 0.061 |
| Environmental dimension | 0.469 | 0.453 | 0.418 | 1.340 | 1.391 | 2.731 | −0.051 |
| Dimensions/Criteria | Influence Given | Influence Received | Prominence | Net Effect | Degree of Importance (Global Weights) | |
|---|---|---|---|---|---|---|
| Technological dimension | 0.342 | |||||
| Technology integration | 4.329 | 4.457 | 8.787 | −0.128 | 0.118 | |
| Technology readiness | 4.358 | 3.865 | 8.223 | 0.493 | 0.102 | |
| Technology security | 4.174 | 4.632 | 8.806 | −0.458 | 0.122 | |
| Organizational dimension | 0.328 | |||||
| Financial commitment | 5.120 | 4.607 | 9.727 | 0.513 | 0.122 | |
| Firm size | 3.722 | 3.304 | 7.025 | 0.418 | 0.087 | |
| Managerial obstacles | 4.118 | 4.501 | 8.619 | −0.382 | 0.118 | |
| Environmental dimension | 0.330 | |||||
| Environmental uncertainty | 3.532 | 4.074 | 7.606 | −0.541 | 0.107 | |
| Competitive pressure | 4.067 | 4.186 | 8.253 | −0.119 | 0.111 | |
| Regulatory support | 4.464 | 4.259 | 8.724 | 0.205 | 0.112 |
| Dimensions/Criteria | Local Weight | Global Weight (DANP) | Performance of EHR Gap () | ||||
|---|---|---|---|---|---|---|---|
| Financial Management | HR Management | ||||||
| Modified | Traditional | Modified | Traditional | ||||
| Technological dimension | 0.342 (1) | 0.134 | 0.000 | 0.220 | 0.228 | ||
| Technology integration | 0.344 | 0.118 (4) | 0.100 | 0.000 | 0.120 | 0.120 | |
| Technology readiness | 0.299 | 0.102 (8) | 0.200 | 0.000 | 0.400 | 0.400 | |
| Technology security | 0.357 | 0.122 (2) | 0.110 | 0.000 | 0.165 | 0.165 | |
| Organizational dimension | 0.328 (3) | 0.404 | 0.657 | 0.377 | 0.390 | ||
| Financial commitment | 0.372 | 0.122 (1) | 0.115 | 0.000 | 0.370 | 0.370 | |
| Firm size | 0.267 | 0.087 (9) | 0.520 | 0.970 | 0.525 | 0.525 | |
| Managerial obstacles | 0.361 | 0.118 (3) | 0.615 | 1.000 | 0.275 | 0.275 | |
| Environmental dimension | 0.330 (2) | 0.352 | 0.393 | 0.374 | 0.375 | ||
| Environmental uncertainty | 0.325 | 0.107 (7) | 0.540 | 1.000 | 0.485 | 0.485 | |
| Competitive pressure | 0.335 | 0.111 (6) | 0.300 | 0.179 | 0.275 | 0.275 | |
| Regulatory support | 0.341 | 0.112 (5) | 0.225 | 0.000 | 0.365 | 0.365 | |
| Total gap | 0.290 | 0.350 | 0.314 | 0.466 | |||
| Scheme | Array of Improvement Priorities | |
|---|---|---|
| F1: Influential relationship network of dimensions | , , | |
| F2: Influential relationship network of criteria within respective dimensions | : , , | |
| : , , | ||
| : , , | ||
| F3: Array of dimension to promote to desired/aspired level in each performance (from low to high by gap value) | In financial management | , , |
| In HR (human resources) management | , , | |
| F4: Array of criteria to promote to desired/aspired level within respective dimension (from low to high by gap value) | In financial management | |
| : , , | ||
| : , , | ||
| : , , | ||
| In HR management | ||
| : , , | ||
| : , , | ||
| : , , | ||
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liou, J.J.H.; Lu, M.-T.; Hu, S.-K.; Cheng, C.-H.; Chuang, Y.-C. A Hybrid MCDM Model for Improving the Electronic Health Record to Better Serve Client Needs. Sustainability 2017, 9, 1819. https://doi.org/10.3390/su9101819
Liou JJH, Lu M-T, Hu S-K, Cheng C-H, Chuang Y-C. A Hybrid MCDM Model for Improving the Electronic Health Record to Better Serve Client Needs. Sustainability. 2017; 9(10):1819. https://doi.org/10.3390/su9101819
Chicago/Turabian StyleLiou, James J. H., Ming-Tsang Lu, Shu-Kung Hu, Chia-Hua Cheng, and Yen-Ching Chuang. 2017. "A Hybrid MCDM Model for Improving the Electronic Health Record to Better Serve Client Needs" Sustainability 9, no. 10: 1819. https://doi.org/10.3390/su9101819
APA StyleLiou, J. J. H., Lu, M.-T., Hu, S.-K., Cheng, C.-H., & Chuang, Y.-C. (2017). A Hybrid MCDM Model for Improving the Electronic Health Record to Better Serve Client Needs. Sustainability, 9(10), 1819. https://doi.org/10.3390/su9101819







