Does Migrant Status and Household Registration Matter? Examining the Effects of City Size on Self-Rated Health
Abstract
:1. Introduction
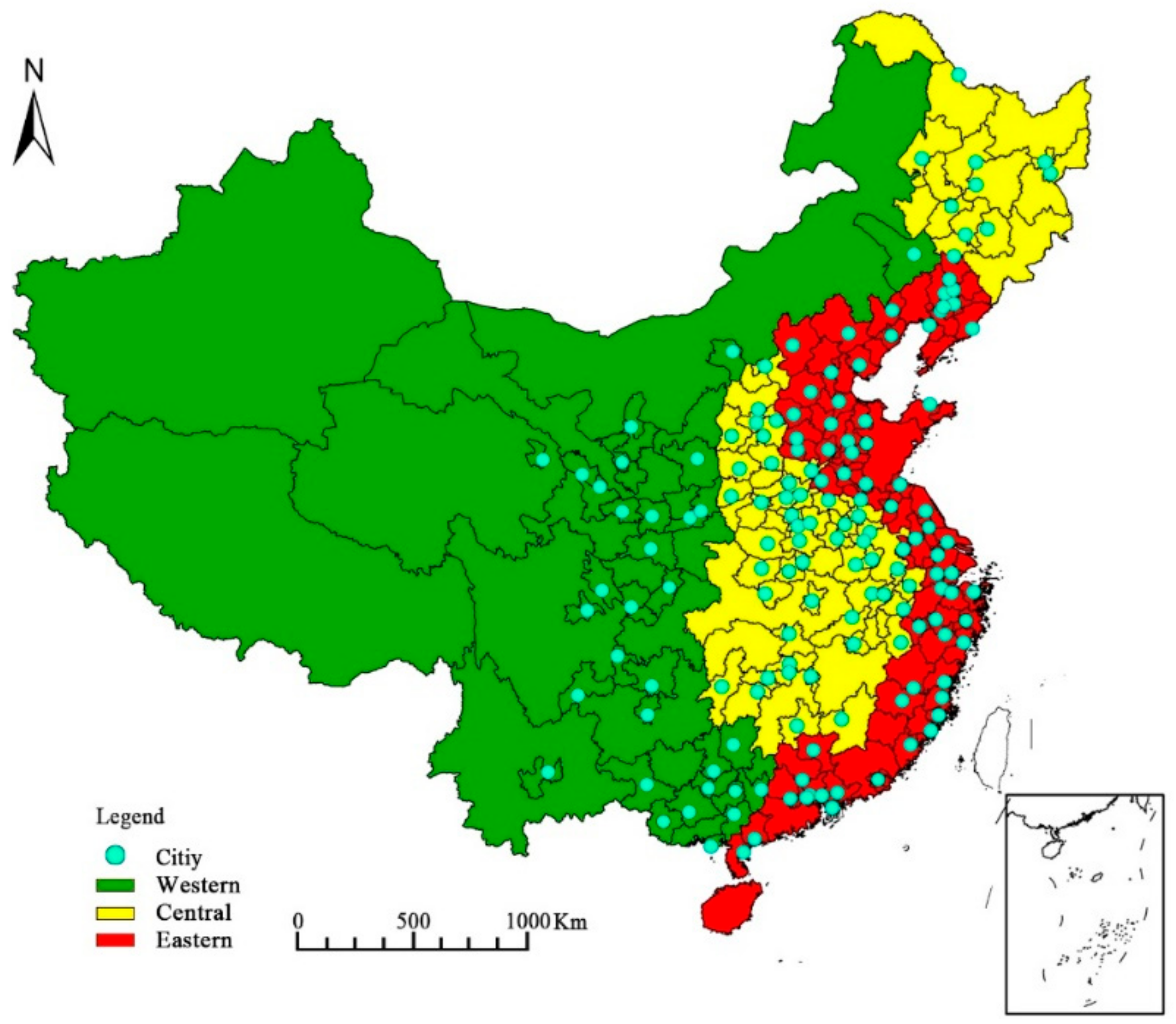
2. Methodology and Data
2.1. Data and Data Sources
2.1.1. Dependent Variables
2.1.2. Key Variables
2.1.3. Control Variables
2.2. Methods
2.3. Statistical Analysis
3. Results and Discussion
3.1. The Proportional Distribution of SRH
3.2. Factors Influencing SRH Status
4. Conclusions and Policy Implications
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Chen, M.; Zhang, H.; Liu, W.; Zhang, W. The global pattern of urbanization and economic growth: Evidence from the last three decades. PLoS ONE 2014, 9, e103799. [Google Scholar] [CrossRef] [PubMed]
- Sun, S.B.; Huang, W.; Hong, J.J.; Wang, C.H. City size, happiness and spatial optimization of migration. Econ. Res. J. 2014, 1, 97–110. (In Chinese) [Google Scholar]
- Miao, L.J.; Wang, Y.L. Analysis on effect of industry cluster from urbanization economy. Urban Stud. 2007, 4, 64–69. [Google Scholar]
- Gao, J.; Wu, P.L. The effect of urban population scale on urban economic growth. Urban Probl. 2016, 6, 4–13. (In Chinese) [Google Scholar]
- Lu, M.; Gao, H.; Zuo, T.H. On urban size and Inclusive Employment. Soc. Sci. China 2012, 10, 47–66. (In Chinese) [Google Scholar]
- Gao, H. On urban size and labor income. J. World Econ. 2014, 10, 145–163. (In Chinese) [Google Scholar]
- Stone, B. Urban sprawl and air quality in large US cities. J. Environ. Manag. 2008, 86, 688–698. [Google Scholar] [CrossRef] [PubMed]
- Bettencourt, L.M.A.; Lobo, J.; Helbing, D.; Kuhnert, C.; West, G.B. Growth, innovation, scaling, and the pace of life in cities. PNAS 2007, 104, 7301–7306. [Google Scholar] [Green Version]
- D’Acci, L. Simulating future societies in Isobenefit Cities: Social isobenefit scenarios. Futures 2013, 54, 3–18. [Google Scholar] [CrossRef] [Green Version]
- De Ridder, K.; Lefebre, F.; Adriaensen, S.; Arnold, U.; Beckroege, W.; Bronner, C.; IntPanis, L. Simulating the impact of urban sprawl on air quality and population exposure in the German Ruhr area. Part I: Reproducing the base state. Atmos. Environ. 2008, 42, 7059–7069. [Google Scholar] [CrossRef]
- Jaana, I.H.; Timo, L.; Tarja, Y.; Anu, W.T.; Jaana, P.; MSC Mika, K.; Jussi, V. Associations of traffic noise with self-rated health and psychotropic medication use. Scand. J. Work. Environ. Health 2014, 40, 235–243. [Google Scholar]
- Reile, R.; Helakorpi, S.; Klumbiene, J.; Tekkel, M.; Leinsalu, M. The recent economic recession and self-rated health in Estonia, Lithuania and Finland: A comparative cross-sectional study in 2004–2010. J. Epidemiol. Community Health 2014, 68, 1072–1079. [Google Scholar] [CrossRef] [PubMed]
- Narumasa, T.; Lzuru, S.; Masayuki, M.; Reiichiro, I. Addressing urban expansion using feature-oriented spatial data in a peripheral area of Ulaanbaatar, Mongolia. Habitat Int. 2015, 47, 196–204. [Google Scholar] [Green Version]
- Meng, W.; Aleksandra, K.; Hisako, K. Effects of urban planning on urban expansion control in Yinchuan City, Western China. Habitat Int. 2017, 64, 85–97. [Google Scholar]
- Wang, S.; Liu, X. China’s city-level energy-related CO2 emissions: Spatiotemporal patterns and driving forces. Appl. Energy 2017, 200, 204–214. [Google Scholar] [CrossRef]
- Louf, R.; Barthelemy, M. Scaling: Lost in the smog. Environ. Plan. B Plan. Des. 2014, 41, 767–769. [Google Scholar] [CrossRef] [Green Version]
- Brian, J.L.B.; Okulicz-Kozaryn, A. An Urban-Rural Happiness Gradient. Urban Geogr. 2011, 32, 871–883. [Google Scholar]
- Adam, O.-K. Unhappy Metropolis (when American city is too big). Cities 2015, 61, 144–155. [Google Scholar]
- Sørensen, J.F.L. Rural-Urban Differences in Life Satisfaction: Evidence from the European Union. Reg. Stud. 2014, 48, 1451–1466. [Google Scholar] [CrossRef]
- Ke, S.N.; Zhao, Y. Industrial Structure, City Size and Urban Productivity in China. Econ. Res. J. 2014, 4, 76–88. (In Chinese) [Google Scholar]
- Chen, J.; Zhou, Q. City size and urban labor productivity in China: New evidence from spatial city-level panel data analysis. Econ. Syst. 2017, 41, 165–178. [Google Scholar] [CrossRef]
- Mossey, J.M.; Shapiro, E. Self-rated health: A predictor of mortality among the elderly. Am. J. Public Health 1982, 72, 800–808. [Google Scholar] [CrossRef] [PubMed]
- Bobak, M.; Pikhart, H.; Rose, R.; Hertzman, C.; Marmot, M. Socioeconomic factors, material inequalities, and perceived control in self-rated health: Cross-sectional data from seven post-communist countries. Soc. Sci. Med. 2000, 51, 1343–1350. [Google Scholar] [CrossRef]
- Pei, X.; Rodriguez, E. Provincial income inequality and self-reported health status in China during 1991–1997. J. Epidemiol. Community Health 2006, 60, 1065–1069. [Google Scholar] [CrossRef] [PubMed]
- Pickett, K.E.; Wilkinson, R.G. Income inequality and health: A causal review. Soc. Sci. Med. 2015, 128, 316–326. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Liu, Y.; Li, Z.; Xue, D. Urbanization, economic development and health: Evidence from China’s labor-force dynamic survey. Int. J. Equity Health 2017, 16, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Van de Poel, E.; O’Donnell, O.; Van Doorslaer, E. Is there a health penalty of China’s rapid urbanization? Health Econ. 2012, 21, 367–385. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Chen, S.; Landry, P.F.; Davis, D.S. How dynamics of urbanization affect physical and mental health in urban China. China Q. 2014, 220, 988–1011. [Google Scholar] [CrossRef]
- Miao, J.; Wu, X. Urbanization, socioeconomic status and health disparity in China. Health Place 2016, 42, 87–95. [Google Scholar] [CrossRef] [PubMed]
- Pope, C.A., III; Burnett, R.T.; Thun, M.J.; Calle, E.E.; Krewski, D.; Ito, K.; Thurston, G.D. Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. Jama 2002, 278, 1132–1141. [Google Scholar] [CrossRef]
- Guo, Y.; Jia, Y.; Pan, X.; Liu, L.; Wichmann, H.E. The association between fine particulate air pollution and hospital emergency room visits for cardiovascular diseases in Beijing, China. Sci. Total. Environ. 2009, 407, 4826–4830. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Deng, F.; Niu, J.; Liu, Y.; Guo, A. Association of heart rate variability in taxi drivers with marked changes in particulate air pollution in Beijing in 2008. Environ. Health Perspect. 2010, 118, 87–91. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Han, Y.Q.; Tang, X.; Zhu, J.; Zhu, T. Estimating adult mortality attributable to PM2.5 exposure in China with assimulated PM2.5 concentrations based on a ground monitoring network. Sci. Total. Environ. 2016, 568, 1253–1262. [Google Scholar] [CrossRef] [PubMed]
- Berkman, L.F.; Syme, S.L. Social network, host resistance and mortality: A nine-year follow-up study of Alameda County residents. Am. J. Epidemiol. 1979, 109, 186–204. [Google Scholar] [CrossRef] [PubMed]
- Kawachi, I.; Berkman, L.F. Social capital, social cohesion, and health. In Social Epidemiology; Berkman, I.F., Kaeachi, I., Glymour, M.M., Eds.; Oxford University Press: New York, NY, USA, 2014; pp. 290–291. [Google Scholar]
- Meng, T.; Chen, H. A multilevel analysis of social capital and self-rated health: Evidence from China. Health Place 2014, 27, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Marmot, M.G.; Bosma, H.; Hemingway, H.; Brunner, E.; Stansfeld, S. Contribution of job control and other risk factors to social variations in coronary heart disease incidence. Lancet 1997, 350, 235–239. [Google Scholar] [CrossRef]
- Lachman, M.E.; Weaver, S.L. The sense of control as a moderator of social class differences in health and well-being. J. Pers. Soc. Psychol. 1998, 74, 763–773. [Google Scholar] [CrossRef] [PubMed]
- Ciccone, D.K.; Vian, T.; Maurer, L.; Bradley, E.H. Linking governance mechanisms to health outcomes: A review of the literature in low- and middle-income countries. Soc. Sci. Med. 2014, 117, 86–95. [Google Scholar] [CrossRef] [PubMed]
- Krueger, P.M.; Dovel, K.; Denney, J.T. Democracy and self-rated health across 67 countries: A multilevel analysis. Soc. Sci. Med. 2015, 143, 137–144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Easterlin, R.A.; Angelescu, L.; Zweig, J.S. The Impact of Modern Economic Growth on Urban Rural Differences in Subjective Well-Being. World Dev. 2011, 39, 2187–2198. [Google Scholar] [CrossRef]
- Muenning, P.; Fahs, M.C. Health status and hospital utilization of recent immigrants to New York City. Prev. Med. 2002, 35, 225–231. [Google Scholar] [CrossRef]
- Newbold, K.B.; Danforth, J. Health status and Canada’s immigrant population. Soc. Sci. Med. 2003, 57, 1981–1995. [Google Scholar] [CrossRef]
- Newbold, K.B. Self-rated health within the Canadian immigrant population: Risk and the healthy immigrant effect. Soc. Sci. Med. 2005, 60, 1359–1370. [Google Scholar] [CrossRef] [PubMed]
- Krause, N.M.; Jay, G.M. What do global self-rated health items measure? Med. Care 1994, 32, 930–942. [Google Scholar] [CrossRef] [PubMed]
- Monica, A.; Guido, D.B.; Gilles, D.; Willam, G.S. Marshallian Labor Market Pooling: Evidence from Italy. Reg. Sci. Urban Econ. 2013, 43, 1008–1022. [Google Scholar]
- Wilkinson, R.G.; Pickett, K.E. Income inequality and population health: A review and explanation of the evidence. Soc. Sci. Med. 2006, 62, 1768–1784. [Google Scholar] [CrossRef] [PubMed]
- Diez Roux, A.V.; Mair, C. Neighborhoods and health. Ann. N. Y. Acad. Sci. 2010, 1186, 125–145. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Doherty, M.G.; French, D.; Steptoe, A.; Kee, F. Social capital, deprivation and self-rated health: Does reporting heterogeneity play a role? Results from the English Longitudinal Study of Ageing. Soc. Sci. Med. 2017, 179, 191–200. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kennedy, B.P.; Kawachi, I.; Glass, R.; Prothrow-Stith, D. Income distribution, socioeconomic status, and self-rated health in the United States: Multilevel analyses. Br. Med. J. 1998, 317, 917–921. [Google Scholar] [CrossRef]
- Berkman, L.F.; Glass, T.; Brissette, I.; Seeman, T.E. From social integration to health: Durkheim in the new millennium. Soc. Sci. Med. 2000, 51, 843–857. [Google Scholar] [CrossRef]
- Eriksson, M. Social capital and health e implications for health promotion. Glob. Health Action 2011, 4, 5611. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, K.L.; Quinn, S.C.; Goodman, R.M.; Butler, J.; Wallace, J. A meta-analysis of social capital and health: A case for needed research. J. Health Psychol. 2013, 18, 1385–1399. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Malin, E.; Nawi, N. Changes in access to structural social capital and its influence on self-rated health over time for middle-aged men and women: A longitudinal study from northern Sweden. Soc. Sci. Med. 2015, 130, 250–258. [Google Scholar]
- Bunker, S.J.; Colquhoun, D.M.; Esler, M.D.; Hickie, I.B.; Hunt, D.; Jelinek, V.M. “Stress” and coronary heart disease: Psychosocial risk factors. National Heart Foundation of Australia position statement update. Med. J. Aust. 2003, 178, 272–276. [Google Scholar] [PubMed]
- Pearson, P.N.; Palmer, M.R. Atmospheric carbon dioxide concentrations over the past 60 million years. Nature 2000, 406, 695–699. [Google Scholar] [CrossRef] [PubMed]
- Zhou, C.S.; Wang, S.J. Examining the determinants and the spatial nexus of city-level CO2 emissions in China: A dynamic spatial panel analysis of China’s cities. J. Clean. Prod. 2018, 171, 917–926. [Google Scholar] [CrossRef]
- Canadell, J.G. Land use effects on terrestrial carbon sources and sinks. Sci. China (Ser. C) 2002, 45, 1–9. [Google Scholar]
- Xu, Q.; Dong, Y.X.; Yang, R. Influence of different geographical factors on carbon sink functions in the Pearl River Delta. Sci. Rep. 2017, 7, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Hooyman, N.R.; Kiyak, H.A. Social Gerontology: A Multidisciplinary Perspective; Allyn & Bacon: Boston, MA, USA, 2011. [Google Scholar]
- Subramanian, S.V.; Kawachi, I. Income inequality and health: What have we learned so far? Epidemiol. Rev. 2004, 26, 78–91. [Google Scholar] [CrossRef] [PubMed]
- Liang, C.S.; Duan, F.K.; He, K.B.; Ma, Y.L. Review on recent progress in observations, source identifications and countermeasures of PM2.5. Environ. Int. 2016, 86, 150–170. [Google Scholar] [CrossRef] [PubMed]
- Paatero, P.; Hopke, P.K.; Hoppenstock, J.; Eberly, S.L. Advanced factor analysis of spatial distributions of PM2.5 in the eastern United States. Environ. Sci. Technol. 2003, 37, 2460–2476. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.B.; Fang, C.L. Spatial-temporal characteristics and determinants of PM2.5 in the Bo Hai Rim urban agglomeration. Chemosphere 2016, 148, 148–162. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q. Regional Decomposition Study on Efficiency Differences of Community Health Services in China. Chin. Health Econ. 2014, 33, 59–61. (In Chinese) [Google Scholar]
- Li, X.M.; Zhao, X.X.; Zhu, Y.Y. Comparing the Contribution of Urbanization to Economic Growth Among China’s Regions of East, Middle and West. Chongqing Technol. Bus. Univ. 2006, 10, 20. [Google Scholar]
- Mor, V.; Victoria, W.; William, R.; Jeffrey, H. Functional Transitions Among the Elderly: Patterns, Predictors and Related Hospital Use. Am. J. Public Health 1994, 84, 1274–1280. [Google Scholar] [CrossRef] [PubMed]
- Haga, H.; Hiroshi, S.; Yasuo, S.; Kazuo, S.; Kiyoshi, I.; Takao, S.; Seiji, Y. Self-Rated Health as a Predictor of Active Life in the Community Elderly. Jpn. J. Epidemiol. 1995, 5, 11–15. [Google Scholar] [CrossRef]
- Li, S.; Xie, X. A new look at the “Asian disease” problem: A choice between the best possible outcomes or between the worst possible outcomes? Think. Reason. 2006, 12, 129–143. [Google Scholar] [CrossRef]

| Variables | Symbol | Expected Direction | Min. | Max. | Mean | Standard Deviation |
|---|---|---|---|---|---|---|
| City size (10,000 people) | CS | + | 3.8 | 678.0 | 194.4 | 186.3 |
| Square of city size | SCS | − | 14.4 | 459,684.0 | 72,438.2 | 129,540.2 |
| Income (Yuan) | IN | + | 200.0 | 800,000.0 | 37,686.2 | 51,489.3 |
| Population density (People/km2) | PD | + | 25.3 | 1440.0 | 497.0 | 327.7 |
| Per capita GDP(Yuan) | PCGDP | + | 10,981 | 132,081 | 57,249.1 | 28,252.0 |
| Per capita green area (m2) | PCGA | + | 2 | 130 | 11.48 | 7.8 |
| Hospital beds (per 10,000 people) | HB | + | 9 | 697 | 74.61 | 29.3 |
| Variable | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | Model 7 | Model 8 | Model 9 | Model 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| CS | 0.862 *** | 0.985 *** | 0.708 *** | 0.880 *** | 0.862 *** | 0.087 *** | 0.796 *** | 0.770 *** | 0.883 *** | 0.839 *** |
| SCS | −0.059 *** | −0.068 *** | −0.050 *** | −0.059 *** | −0.059 *** | −0.060 *** | −0.055 *** | −0.54 *** | −0.060 *** | −0.058 *** |
| MS | −0.114 ** | 2.836 | −0.116 *** | −0.115 ** | 0.756 | |||||
| HR | −0.236 *** | −0.350 | −0.203 *** | −0.234 *** | 0.556 | |||||
| IN | 0.066 *** | 0.068 *** | 0.060 *** | 0.068 *** | 0.066 *** | 0.064 *** | 0.065 *** | 0.060 *** | 0.065 *** | 0.064 *** |
| PD | 0.063 ** | 0.038 | ||||||||
| PCGDP | −0.031 | −0.022 | ||||||||
| CS × MS | −0.882 * | |||||||||
| SCS × MS | 0.064 * | |||||||||
| CS × HR | −0.110 ** | |||||||||
| SCS × HR | 0.019 | |||||||||
| Individual heterogeneity | × | × | × | × | √ | × | × | × | × | √ |
| Constant term | −2.512 ** | −2.854 ** | −2.322 ** | −2.212 * | −2.621 ** | −2.524 ** | −2.260 | −2.423 ** | −2.312 * | −2.574 ** |
| Samples | 1349 | 1349 | 1349 | 1349 | 1349 | 1349 | 1349 | 1349 | 1349 | 1349 |
| R2 | 0.324 | 0.325 | 0.327 | 0.324 | 0.326 | 0.328 | 0.329 | 0.329 | 0.328 | 0.328 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, C.; Chen, J.; Wang, S. Does Migrant Status and Household Registration Matter? Examining the Effects of City Size on Self-Rated Health. Sustainability 2018, 10, 2204. https://doi.org/10.3390/su10072204
Zhou C, Chen J, Wang S. Does Migrant Status and Household Registration Matter? Examining the Effects of City Size on Self-Rated Health. Sustainability. 2018; 10(7):2204. https://doi.org/10.3390/su10072204
Chicago/Turabian StyleZhou, Chunshan, Jing Chen, and Shaojian Wang. 2018. "Does Migrant Status and Household Registration Matter? Examining the Effects of City Size on Self-Rated Health" Sustainability 10, no. 7: 2204. https://doi.org/10.3390/su10072204
APA StyleZhou, C., Chen, J., & Wang, S. (2018). Does Migrant Status and Household Registration Matter? Examining the Effects of City Size on Self-Rated Health. Sustainability, 10(7), 2204. https://doi.org/10.3390/su10072204





