Stress Distribution within the Peri-Implant Bone for Different Implant Materials Obtained by Digital Image Correlation
Abstract
:1. Introduction
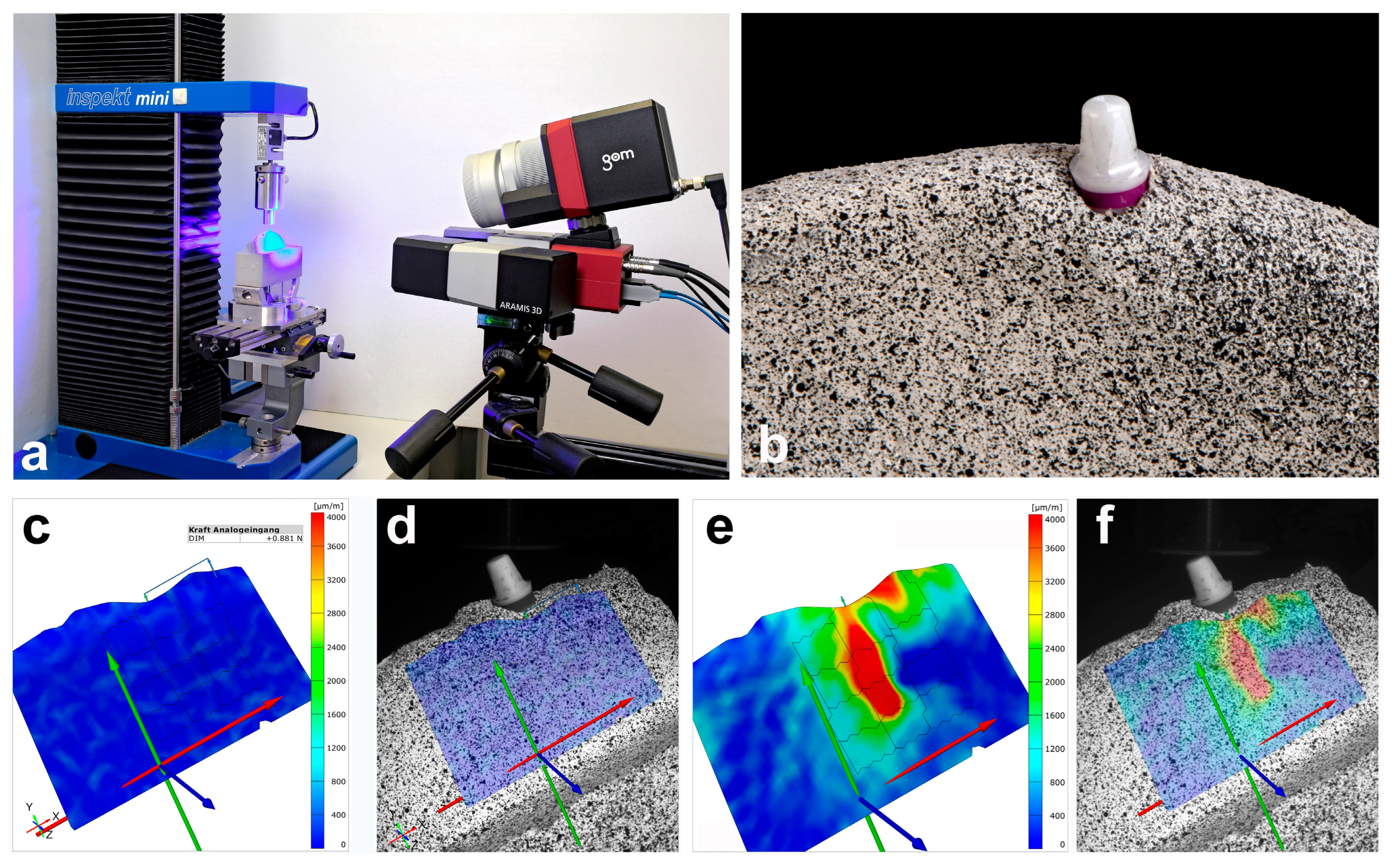
2. Materials and Methods
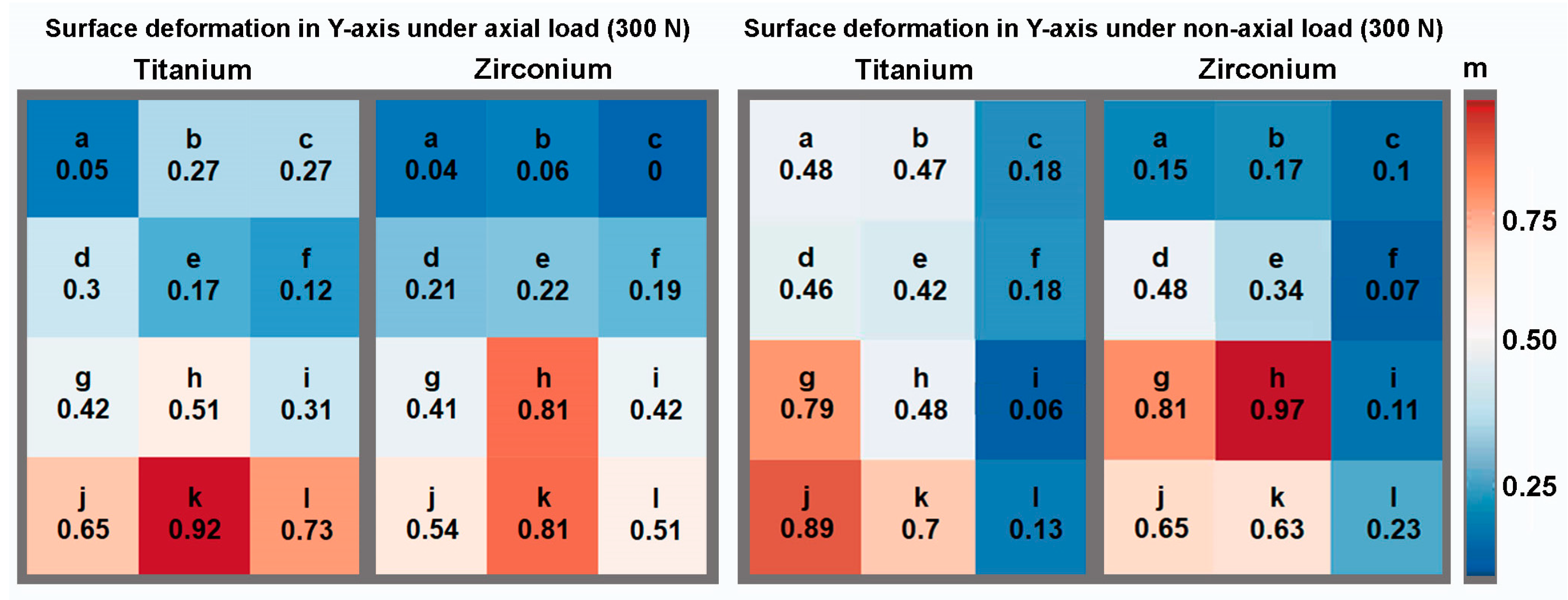
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Branemark, P.I.; Adell, R.; Breine, U.; Hansson, B.O.; Lindstrom, J.; Ohlsson, A. Intra-osseous anchorage of dental prostheses. I. Experimental studies. Scand. J. Plast. Reconstr. Surg. 1969, 3, 81–100. [Google Scholar] [CrossRef] [PubMed]
- Assif, D.; Marshak, B.; Horowitz, A. Analysis of load transfer and stress distribution by an implant-supported fixed partial denture. J. Prosthet. Dent. 1996, 75, 285–291. [Google Scholar] [CrossRef] [PubMed]
- Frost, H.M. Wolff’s Law and bone’s structural adaptations to mechanical usage: An overview for clinicians. Angle Orthod. 1994, 64, 175–188. [Google Scholar] [CrossRef] [PubMed]
- Wiskott, H.W.; Belser, U.C. Lack of integration of smooth titanium surfaces: A working hypothesis based on strains generated in the surrounding bone. Clin. Oral Implants Res. 1999, 10, 429–444. [Google Scholar] [CrossRef] [PubMed]
- Frost, H.M. A 2003 update of bone physiology and Wolff’s Law for clinicians. Angle Orthod. 2004, 74, 3–15. [Google Scholar] [CrossRef] [PubMed]
- Cehreli, M.C.; Iplikcioglu, H.; Bilir, O.G. The influence of the location of load transfer on strains around implants supporting four unit cement-retained fixed prostheses: In vitro evaluation of axial versus off-set loading. J. Oral Rehabil. 2002, 29, 394–400. [Google Scholar] [CrossRef]
- Lee, J.H.; Frias, V.; Lee, K.W.; Wright, R.F. Effect of implant size and shape on implant success rates: A literature review. J. Prosthet. Dent. 2005, 94, 377–381. [Google Scholar] [CrossRef]
- Nishioka, R.S.; Nishioka, L.N.; Abreu, C.W.; de Vasconcellos, L.G.; Balducci, I. Machined and plastic copings in three-element prostheses with different types of implant-abutment joints: A strain gauge comparative analysis. J. Appl. Oral Sci. 2010, 18, 225–230. [Google Scholar] [CrossRef]
- de Vasconcellos, L.G.; Nishioka, R.S.; de Vasconcellos, L.M.; Balducci, I.; Kojima, A.N. Microstrain around dental implants supporting fixed partial prostheses under axial and non-axial loading conditions, in vitro strain gauge analysis. J. Craniofacial Surg. 2013, 24, e546–e551. [Google Scholar] [CrossRef]
- Kheiralla, L.S.; Younis, J.F. Peri-implant biomechanical responses to standard, short-wide, and mini implants supporting single crowns under axial and off-axial loading (an in vitro study). J. Oral Implantol. 2014, 40, 42–52. [Google Scholar] [CrossRef]
- Fabris, D.; Moura, J.P.A.; Fredel, M.C.; Souza, J.C.M.; Silva, F.S.; Henriques, B. Biomechanical analyses of one-piece dental implants composed of titanium, zirconia, PEEK, CFR-PEEK, or GFR-PEEK: Stresses, strains, and bone remodeling prediction by the finite element method. J. Biomed. Mater. Res. B Appl. Biomater. 2022, 110, 79–88. [Google Scholar] [CrossRef] [PubMed]
- Osman, R.B.; Swain, M.V. A Critical Review of Dental Implant Materials with an Emphasis on Titanium versus Zirconia. Materials 2015, 8, 932–958. [Google Scholar] [CrossRef] [PubMed]
- Khaohoen, A.; Sornsuwan, T.; Chaijareenont, P.; Poovarodom, P.; Rungsiyakull, C.; Rungsiyakull, P. Biomaterials and Clinical Application of Dental Implants in Relation to Bone Density-A Narrative Review. J. Clin. Med. 2023, 12, 6924. [Google Scholar] [CrossRef] [PubMed]
- Albrektsson, T.; Jacobsson, M. Bone-metal interface in osseointegration. J. Prosthet. Dent. 1987, 57, 597–607. [Google Scholar] [CrossRef] [PubMed]
- Palmquist, A.; Omar, O.M.; Esposito, M.; Lausmaa, J.; Thomsen, P. Titanium oral implants: Surface characteristics, interface biology and clinical outcome. J. R. Soc. Interface 2010, 7 (Suppl. S5), S515–S527. [Google Scholar] [CrossRef]
- Hoque, M.E.; Showva, N.N.; Ahmed, M.; Rashid, A.B.; Sadique, S.E.; El-Bialy, T.; Xu, H. Titanium and titanium alloys in dentistry: Current trends, recent developments, and future prospects. Heliyon 2022, 8, e11300. [Google Scholar] [CrossRef]
- Binon, P.P. Implants and components: Entering the new millennium. Int. J. Oral Maxillofac. Implants 2000, 15, 76–94. [Google Scholar] [PubMed]
- Jung, R.E.; Sailer, I.; Hammerle, C.H.; Attin, T.; Schmidlin, P. In vitro color changes of soft tissues caused by restorative materials. Int. J. Periodontics Restor. Dent. 2007, 27, 251–257. [Google Scholar]
- Sevimay, M.; Turhan, F.; Kilicarslan, M.A.; Eskitascioglu, G. Three-dimensional finite element analysis of the effect of different bone quality on stress distribution in an implant-supported crown. J. Prosthet. Dent. 2005, 93, 227–234. [Google Scholar] [CrossRef]
- Manzano, G.; Herrero, L.R.; Montero, J. Comparison of clinical performance of zirconia implants and titanium implants in animal models: A systematic review. Int. J. Oral Maxillofac. Implants 2014, 29, 311–320. [Google Scholar] [CrossRef]
- Wenz, H.J.; Bartsch, J.; Wolfart, S.; Kern, M. Osseointegration and clinical success of zirconia dental implants: A systematic review. Int. J. Prosthodont. 2008, 21, 27–36. [Google Scholar] [PubMed]
- Roehling, S.; Astasov-Frauenhoffer, M.; Hauser-Gerspach, I.; Braissant, O.; Woelfler, H.; Waltimo, T.; Kniha, H.; Gahlert, M. In Vitro Biofilm Formation on Titanium and Zirconia Implant Surfaces. J. Periodontol. 2017, 88, 298–307. [Google Scholar] [CrossRef] [PubMed]
- Happe, A.; Schulte-Mattler, V.; Strassert, C.; Naumann, M.; Stimmelmayr, M.; Zoller, J.E.; Rothamel, D. In vitro color changes of soft tissues caused by dyed fluorescent zirconia and nondyed, nonfluorescent zirconia in thin mucosa. Int. J. Periodontics Restor. Dent. 2013, 33, e1–e8. [Google Scholar] [CrossRef] [PubMed]
- Kohal, R.J.; Knauf, M.; Larsson, B.; Sahlin, H.; Butz, F. One-piece zirconia oral implants: One-year results from a prospective cohort study. 1. Single tooth replacement. J. Clin. Periodontol. 2012, 39, 590–597. [Google Scholar] [CrossRef] [PubMed]
- Jung, R.E.; Grohmann, P.; Sailer, I.; Steinhart, Y.N.; Feher, A.; Hammerle, C.; Strub, J.R.; Kohal, R. Evaluation of a one-piece ceramic implant used for single-tooth replacement and three-unit fixed partial dentures: A prospective cohort clinical trial. Clin. Oral Implants Res. 2016, 27, 751–761. [Google Scholar] [CrossRef] [PubMed]
- Kohal, R.J.; Finke, H.C.; Klaus, G. Stability of prototype two-piece zirconia and titanium implants after artificial aging: An in vitro pilot study. Clin. Implant Dent. Relat. Res. 2009, 11, 323–329. [Google Scholar] [CrossRef] [PubMed]
- Sannino, G.; Gloria, F.; Ottria, L.; Barlattani, A. Influence of finish line in the distribution of stress trough an all ceramic implant-supported crown.: A 3D Finite Element Analysis. Oral Implantol. 2009, 2, 14–27. [Google Scholar]
- Lopez, C.A.V.; Vasco, M.A.A.; Ruales, E.; Bedoya, K.A.; Benfatti, C.M.; Bezzon, O.L.; Deliberador, T.M. Three-Dimensional Finite Element Analysis of Stress Distribution in Zirconia and Titanium Dental Implants. J. Oral Implantol. 2018, 44, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Brenner, S.C. The Mathematical Theory of Finite Element Methods, 3rd ed.; Springer: New York, NY, USA, 2008; p. 96. [Google Scholar]
- Matta, R.E.; Riegger, K.; Trägler, H.; Adler, W.; Eitner, S.; Wichmann, M.; Motel, C. Establishment of a New Biomechanical Measurement Method for Surface Deformation of Bone by Force Application via Dental Implants—A Pilot Study. Appl. Sci. 2021, 11, 7568. [Google Scholar] [CrossRef]
- Bakalarz, M.M.; Tworzewski, P.P. Application of Digital Image Correlation to Evaluate Strain, Stiffness and Ductility of Full-Scale LVL Beams Strengthened by CFRP. Materials 2023, 16, 1309. [Google Scholar] [CrossRef]
- Goellner, M.; Berthold, C.; Holst, S.; Wichmann, M.; Schmitt, J. Correlations between photogrammetric measurements of tooth mobility and the Periotest method. Acta Odontol. Scand. 2012, 70, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Lezaja, M.; Veljovic, D.; Manojlovic, D.; Milosevic, M.; Mitrovic, N.; Janackovic, D.; Miletic, V. Bond strength of restorative materials to hydroxyapatite inserts and dimensional changes of insert-containing restorations during polymerization. Dent. Mater. 2015, 31, 171–181. [Google Scholar] [CrossRef] [PubMed]
- Miletic, V.; Peric, D.; Milosevic, M.; Manojlovic, D.; Mitrovic, N. Local deformation fields and marginal integrity of sculptable bulk-fill, low-shrinkage and conventional composites. Dent. Mater. 2016, 32, 1441–1451. [Google Scholar] [CrossRef] [PubMed]
- Haseeb, S.A.; Vinaya, K.C.; Vijaykumar, N.; Sree Durga, B.A.; Kumar, A.S.; Sruthi, M.K. Finite element evaluation to compare stress pattern in bone surrounding implant with carbon fiber-reinforced poly-ether-ether-ketone and commercially pure titanium implants. Natl. J. Maxillofac. Surg. 2022, 13, 243–247. [Google Scholar] [CrossRef] [PubMed]
- Wight, C.M.; Schemitsch, E.H. In vitro testing for hip head-neck taper tribocorrosion: A review of experimental methods. Proc. Inst. Mech. Eng. Part H 2022, 236, 9544119221074582. [Google Scholar] [CrossRef]
- Masoomi, F.; Mahboub, F. Stress distribution pattern in all-on-four maxillary restorations supported by porous tantalum and solid titanium implants using three-dimensional finite element analysis. Eur. J. Transl. Myol. 2024, 34. [Google Scholar] [CrossRef] [PubMed]
- Tribst, J.P.M.; Dal Piva, A.M.O.; Ozcan, M.; Borges, A.L.S.; Bottino, M.A. Influence of Ceramic Materials on Biomechanical Behavior of Implant Supported Fixed Prosthesis with Hybrid Abutment. Eur. J. Prosthodont. Restor. Dent. 2019, 27, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Boldt, J.; Knapp, W.; Proff, P.; Rottner, K.; Richter, E.J. Measurement of tooth and implant mobility under physiological loading conditions. Ann. Anat. 2012, 194, 185–189. [Google Scholar] [CrossRef] [PubMed]
- Pilliar, R.M.; Lee, J.M.; Maniatopoulos, C. Observations on the effect of movement on bone ingrowth into porous-surfaced implants. Clin. Orthop. Relat. Res. 1986, 208, 108–113. [Google Scholar] [CrossRef]
- Brunski, J.B. Biomechanical factors affecting the bone-dental implant interface. Clin. Mater. 1992, 10, 153–201. [Google Scholar] [CrossRef]
- Kao, H.C.; Gung, Y.W.; Chung, T.F.; Hsu, M.L. The influence of abutment angulation on micromotion level for immediately loaded dental implants: A 3-D finite element analysis. Int. J. Oral Maxillofac. Implants 2008, 23, 623–630. [Google Scholar] [PubMed]
- Sakka, S.; Baroudi, K.; Nassani, M.Z. Factors associated with early and late failure of dental implants. J. Investig. Clin. Dent. 2012, 3, 258–261. [Google Scholar] [CrossRef] [PubMed]
- Duyck, J.; Vandamme, K. The effect of loading on peri-implant bone: A critical review of the literature. J. Oral Rehabil. 2014, 41, 783–794. [Google Scholar] [CrossRef] [PubMed]
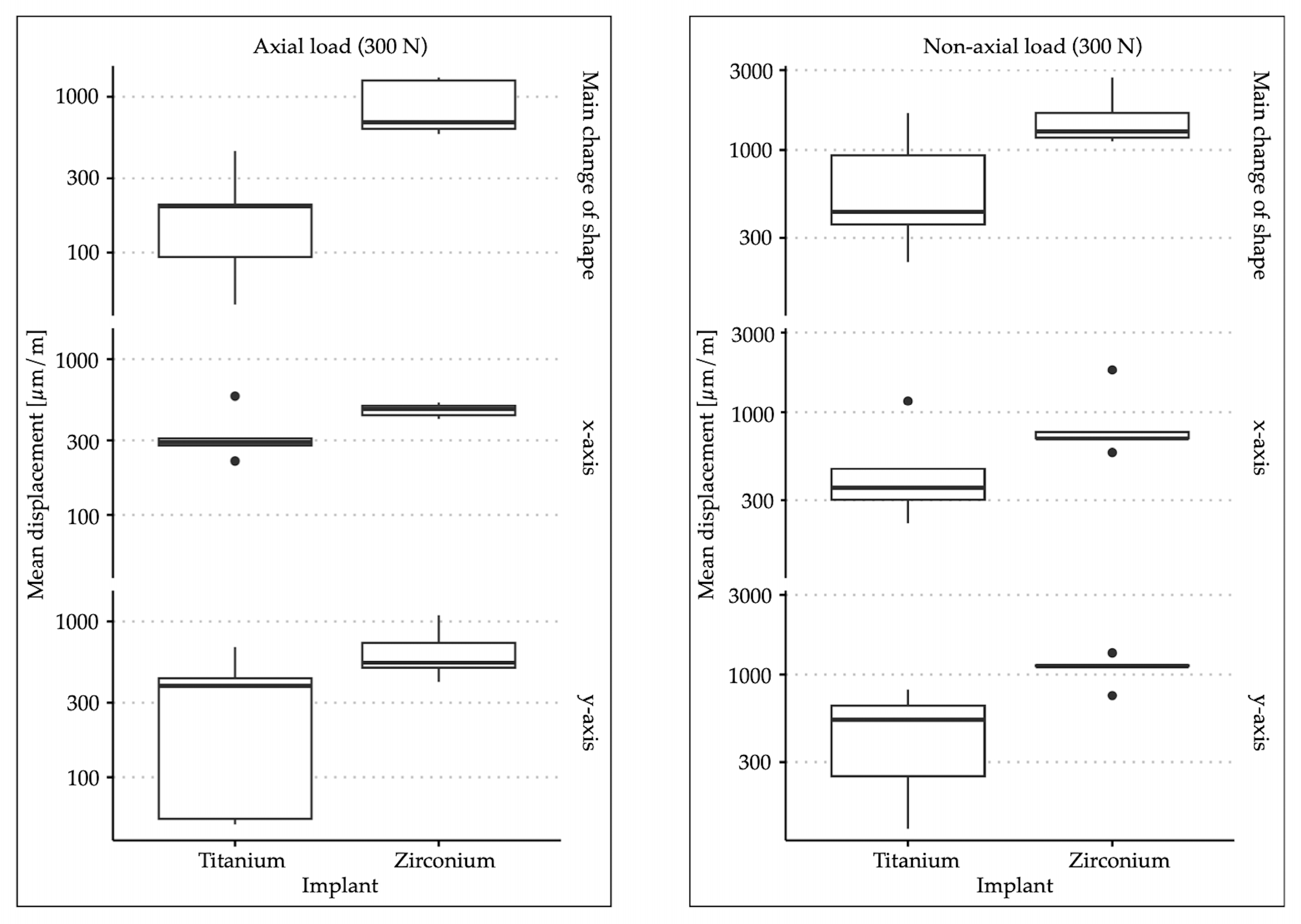
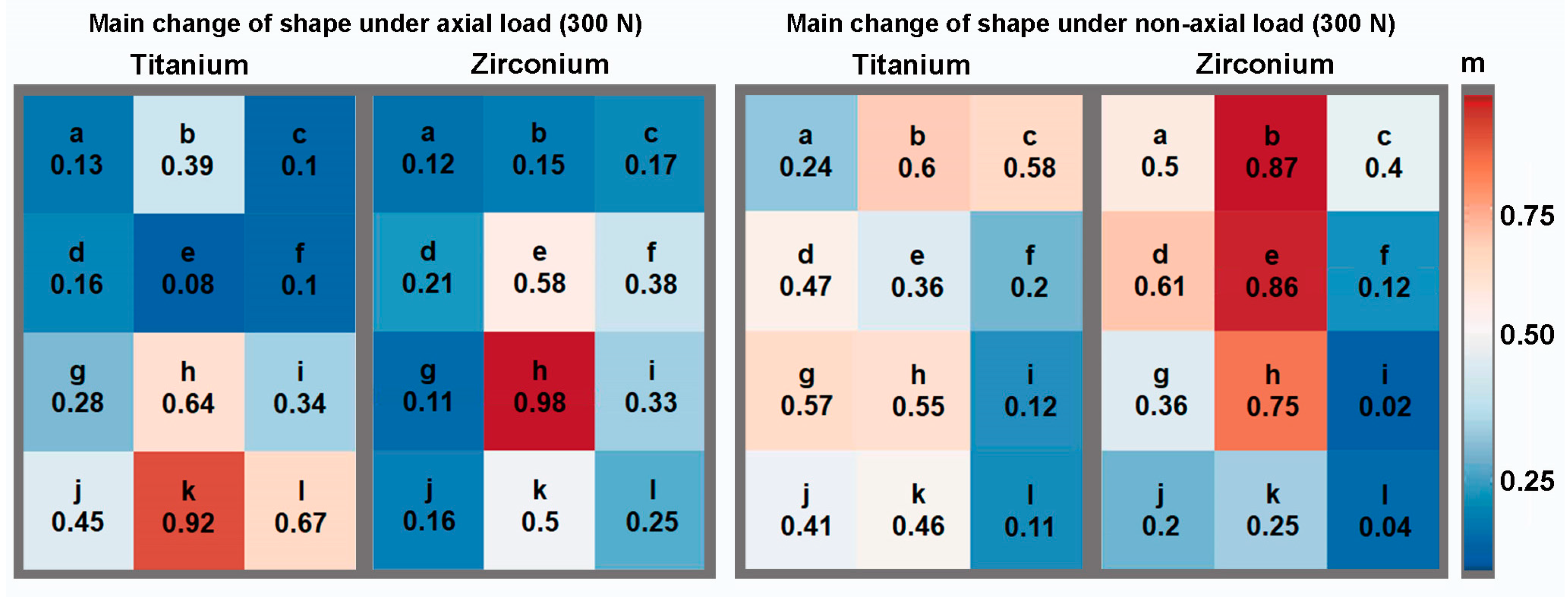
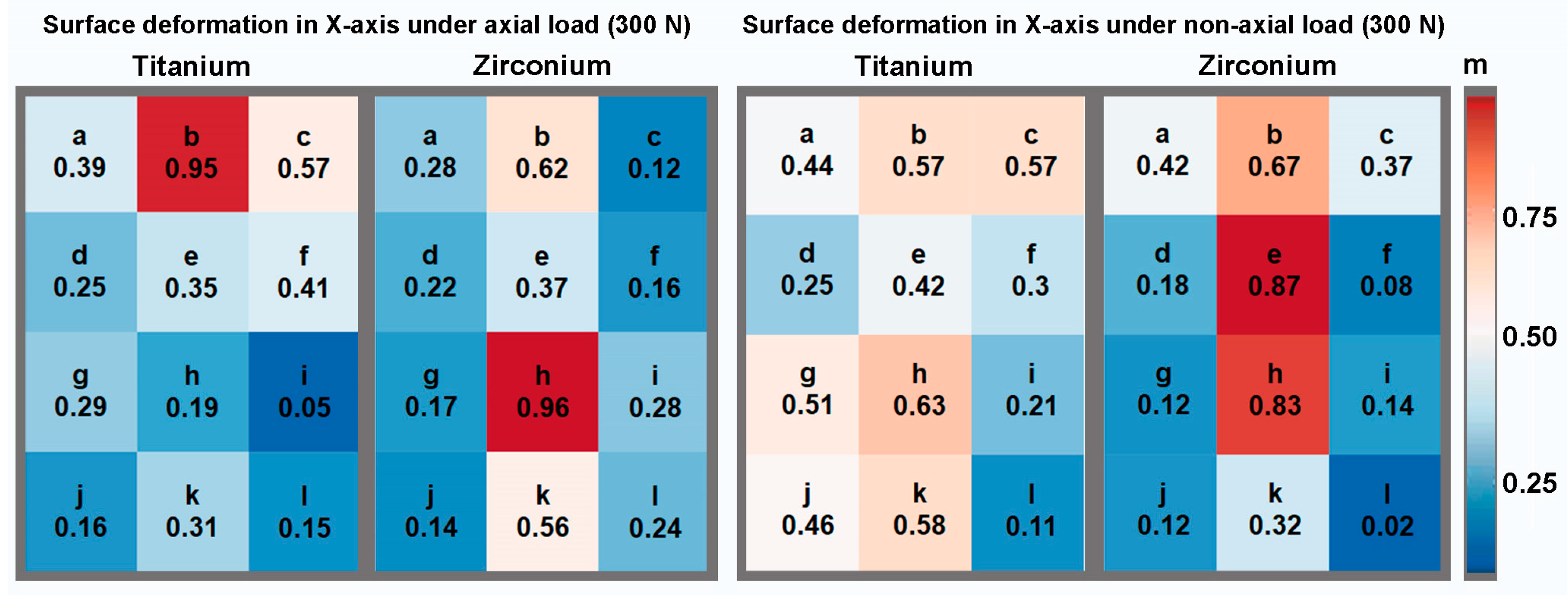
| Material | Angulation | Main Change in Shape | Change in Shape in X-axis | Change in Shape in Y-axis | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| Titanium | 0° | 198.38 | 155.57 | 336.02 | 139.62 | 320.9 | 270.41 |
| 30° | 720.77 | 594.95 | 501.09 | 383.49 | 475.05 | 287.1 | |
| Zirconium | 0° | 898.95 | 373.53 | 471.83 | 47.25 | 654.69 | 271.02 |
| 30° | 1601.46 | 661.08 | 906.31 | 499.68 | 1095.38 | 216.24 | |
| Angulation | Dimension | p-Value |
|---|---|---|
| 0° | main change in shape | 0.009 |
| X-axis | 0.1172 | |
| Y-axis | 0.0758 | |
| 30° | main change in shape | 0.0472 |
| X-axis | 0.0758 | |
| Y-axis | 0.0163 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matta, R.E.; Berger, L.; Loehlein, M.; Leven, L.; Taxis, J.; Wichmann, M.; Motel, C. Stress Distribution within the Peri-Implant Bone for Different Implant Materials Obtained by Digital Image Correlation. Materials 2024, 17, 2161. https://doi.org/10.3390/ma17092161
Matta RE, Berger L, Loehlein M, Leven L, Taxis J, Wichmann M, Motel C. Stress Distribution within the Peri-Implant Bone for Different Implant Materials Obtained by Digital Image Correlation. Materials. 2024; 17(9):2161. https://doi.org/10.3390/ma17092161
Chicago/Turabian StyleMatta, Ragai Edward, Lara Berger, Moritz Loehlein, Linus Leven, Juergen Taxis, Manfred Wichmann, and Constantin Motel. 2024. "Stress Distribution within the Peri-Implant Bone for Different Implant Materials Obtained by Digital Image Correlation" Materials 17, no. 9: 2161. https://doi.org/10.3390/ma17092161





