Biaxial Flexural Strength of Printed Splint Materials
Abstract
:1. Introduction
2. Materials and Methods
2.1. Printing
2.2. Cleaning
2.3. Post-Polymerization
2.4. Processing
2.5. Storage
2.6. Testing
- σ = biaxial flexural strength (MPa);
- P = fracture force (N);
- d = sample thickness at fracture origin (mm).
- v = Poisson’s ratio (0.3) [32];
- r1 = radius of the supporting bearing;
- r2 = radius of the loaded area;
- r3 = radius of the sample.
2.7. Statistics
3. Results
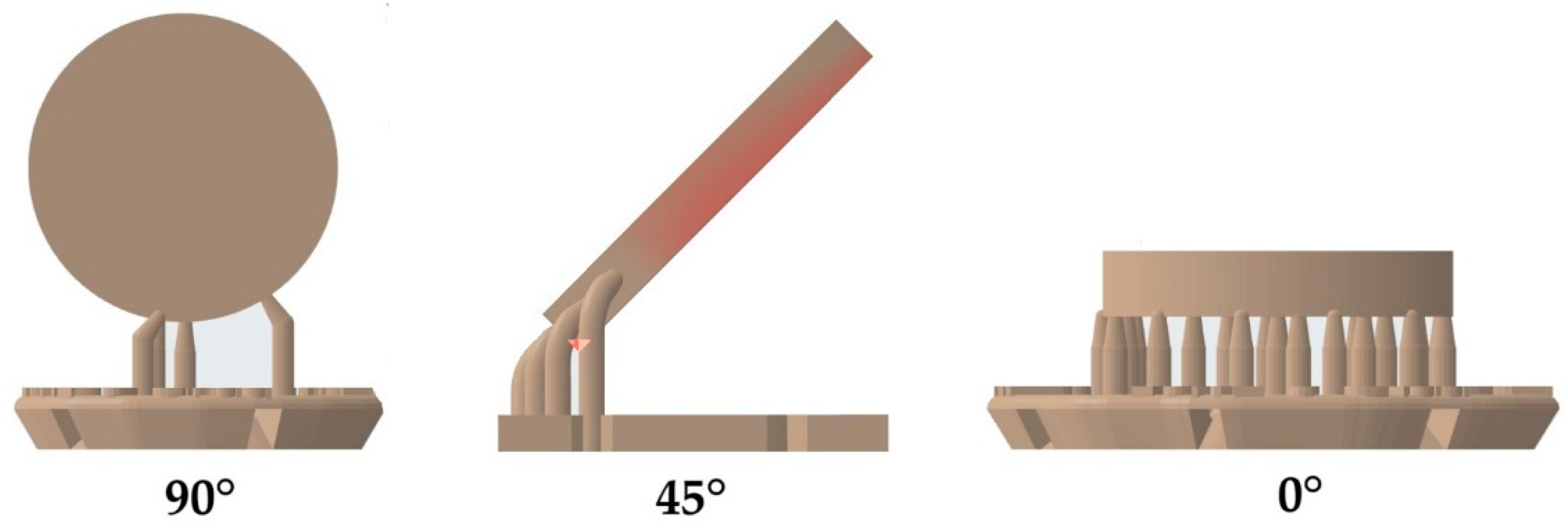
3.1. Build Orientation
3.2. Cleaning
3.3. Post-Polymerization
3.4. Storage
3.5. Statistics
4. Discussion
4.1. Build Orientation
4.2. Cleaning
4.3. Post-Polymerization
4.4. Storage
5. Conclusions
- Samples printed at a build angle of 90° showed the highest biaxial flexural strength values in comparison with those printed at either 0° or 45°.
- Samples cured with an LED device showed higher biaxial strength values than those cured with Xenon light.
- The aging of the samples significantly decreased the mechanical properties of the materials.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- List, T.; Jensen, R.H. Temporomandibular disorders: Old ideas and new concepts. Cephalalgia 2017, 37, 692–704. [Google Scholar] [CrossRef]
- Zhang, S.-H.; He, K.-X.; Lin, C.-J.; Liu, X.-D.; Wu, L.; Chen, J.; Rausch-Fan, X. Efficacy of occlusal splints in the treatment of temporomandibular disorders: A systematic review of randomized controlled trials. Acta Odontol. Scand. 2020, 78, 580–589. [Google Scholar] [CrossRef]
- LeResche, L. Epidemiology of temporomandibular disorders: Implications for the investigation of etiologic factors. Crit. Rev. Oral Biol. Med. 1997, 8, 291–305. [Google Scholar] [CrossRef]
- Lobbezoo, F.; Ahlberg, J.; Raphael, K.G.; Wetselaar, P.; Glaros, A.G.; Kato, T.; Santiago, V.; Winocur, E.; de Laat, A.; de Leeuw, R.; et al. International consensus on the assessment of bruxism: Report of a work in progress. J. Oral Rehabil. 2018, 45, 837–844. [Google Scholar] [CrossRef]
- Ainoosah, S.; Farghal, A.E.; Alzemei, M.S.; Saini, R.S.; Gurumurthy, V.; Quadri, S.A.; Okshah, A.; Mosaddad, S.A.; Heboyan, A. Comparative analysis of different types of occlusal splints for the management of sleep bruxism: A systematic review. BMC Oral Health 2024, 24, 29. [Google Scholar] [CrossRef]
- Patzelt, S.B.M.; Krügel, M.; Wesemann, C.; Pieralli, S.; Nold, J.; Spies, B.C.; Vach, K.; Kohal, R.-J. In Vitro Time Efficiency, Fit, and Wear of Conventionally- versus Digitally-Fabricated Occlusal Splints. Materials 2022, 15, 85. [Google Scholar] [CrossRef]
- Perea-Lowery, L.; Gibreel, M.; Garoushi, S.; Vallittu, P.; Lassila, L. Evaluation of flexible three-dimensionally printed occlusal splint materials: An in vitro study. Dent. Mater. 2023, 39, 957–963. [Google Scholar] [CrossRef]
- Kuzmanovic Pficer, J.; Dodic, S.; Lazic, V.; Trajkovic, G.; Milic, N.; Milicic, B. Occlusal stabilization splint for patients with temporomandibular disorders: Meta-analysis of short and long term effects. PLoS ONE 2017, 12, e0171296. [Google Scholar] [CrossRef]
- Lutz, A.-M.; Hampe, R.; Roos, M.; Lümkemann, N.; Eichberger, M.; Stawarczyk, B. Fracture resistance and 2-body wear of 3-dimensional-printed occlusal devices. J. Prosthet. Dent. 2019, 121, 166–172. [Google Scholar] [CrossRef]
- Dedem, P.; Türp, J.C. Digital Michigan splint—From intraoral scanning to plasterless manufacturing. Int. J. Comput. Dent. 2016, 19, 63–76. [Google Scholar]
- Methani, M.M.; Cesar, P.F.; de Paula Miranda, R.B.; Morimoto, S.; Özcan, M.; Revilla-León, M. Additive Manufacturing in Dentistry: Current Technologies, Clinical Applications, and Limitations. Curr. Oral Health Rep. 2020, 7, 327–334. [Google Scholar] [CrossRef]
- Benli, M.; Al-Haj Husain, N.; Ozcan, M. Mechanical and chemical characterization of contemporary occlusal splint materials fabricated with different methods: A systematic review. Clin. Oral Investig. 2023, 27, 7115–7141. [Google Scholar] [CrossRef]
- Berli, C.; Thieringer, F.M.; Sharma, N.; Müller, J.A.; Dedem, P.; Fischer, J.; Rohr, N. Comparing the mechanical properties of pressed, milled, and 3D-printed resins for occlusal devices. J. Prosthet. Dent. 2020, 124, 780–786. [Google Scholar] [CrossRef]
- Alharbi, N.; Osman, R.; Wismeijer, D. Effects of build direction on the mechanical properties of 3D-printed complete coverage interim dental restorations. J. Prosthet. Dent. 2016, 115, 760–767. [Google Scholar] [CrossRef]
- Kessler, A.; Reymus, M.; Hickel, R.; Kunzelmann, K.-H. Three-body wear of 3D printed temporary materials. Dent. Mater. 2019, 35, 1805–1812. [Google Scholar] [CrossRef] [PubMed]
- Wedekind, L.; Güth, J.-F.; Schweiger, J.; Kollmuss, M.; Reichl, F.-X.; Edelhoff, D.; Högg, C. Elution behavior of a 3D-printed, milled and conventional resin-based occlusal splint material. Dent. Mater. 2021, 37, 701–710. [Google Scholar] [CrossRef]
- Alifui-Segbaya, F.; Bowman, J.; White, A.R.; George, R.; Fidan, I. Characterization of the Double Bond Conversion of Acrylic Resins for 3D Printing of Dental Prostheses. Compend. Contin. Educ. Dent. 2019, 40, e7–e11. [Google Scholar]
- Perea-Lowery, L.; Gibreel, M.; Vallittu, P.K.; Lassila, L. Evaluation of the mechanical properties and degree of conversion of 3D printed splint material. J. Mech. Behav. Biomed. Mater. 2021, 115, 104254. [Google Scholar] [CrossRef]
- Nestler, N.; Wesemann, C.; Spies, B.C.; Beuer, F.; Bumann, A. Dimensional accuracy of extrusion- and photopolymerization-based 3D printers: In vitro study comparing printed casts. J. Prosthet. Dent. 2020, 125, 103–110. [Google Scholar] [CrossRef]
- Park, G.-S.; Kim, S.-K.; Heo, S.-J.; Koak, J.-Y.; Seo, D.-G. Effects of Printing Parameters on the Fit of Implant-Supported 3D Printing Resin Prosthetics. Materials 2019, 12, 2533. [Google Scholar] [CrossRef]
- Reymus, M.; Fabritius, R.; Keßler, A.; Hickel, R.; Edelhoff, D.; Stawarczyk, B. Fracture load of 3D-printed fixed dental prostheses compared with milled and conventionally fabricated ones: The impact of resin material, build direction, post-curing, and artificial aging-an in vitro study. Clin. Oral Investig. 2020, 24, 701–710. [Google Scholar] [CrossRef]
- Park, S.-M.; Park, J.-M.; Kim, S.-K.; Heo, S.-J.; Koak, J.-Y. Flexural Strength of 3D-Printing Resin Materials for Provisional Fixed Dental Prostheses. Materials 2020, 13, 3970. [Google Scholar] [CrossRef]
- Nold, J.; Wesemann, C.; Rieg, L.; Binder, L.; Witkowski, S.; Spies, B.C.; Kohal, R.J. Does Printing Orientation Matter? In-Vitro Fracture Strength of Temporary Fixed Dental Prostheses after a 1-Year Simulation in the Artificial Mouth. Materials 2021, 14, 259. [Google Scholar] [CrossRef]
- Hada, T.; Kanazawa, M.; Iwaki, M.; Arakida, T.; Soeda, Y.; Katheng, A.; Otake, R.; Minakuchi, S. Effect of Printing Direction on the Accuracy of 3D-Printed Dentures Using Stereolithography Technology. Materials 2020, 13, 3405. [Google Scholar] [CrossRef]
- Marcel, R.; Reinhard, H.; Andreas, K. Accuracy of CAD/CAM-fabricated bite splints: Milling vs 3D printing. Clin. Oral Investig. 2020, 24, 4607–4615. [Google Scholar] [CrossRef]
- Grymak, A.; Aarts, J.M.; Ma, S.; Waddell, J.N.; Choi, J.J.E. Comparison of hardness and polishability of various occlusal splint materials. J. Mech. Behav. Biomed. Mater. 2021, 115, 104270. [Google Scholar] [CrossRef]
- Puebla, K.; Arcaute, K.; Quintana, R.; Wicker, R.B. Effects of environmental conditions, aging, and build orientations on the mechanical properties of ASTM type I specimens manufactured via stereolithography. Rapid Prototyp. J. 2012, 18, 374–388. [Google Scholar] [CrossRef]
- Calderon, P.d.S.; Kogawa, E.M.; Lauris, J.R.P.; Conti, P.C.R. The influence of gender and bruxism on the human maximum bite force. J. Appl. Oral Sci. 2006, 14, 448–453. [Google Scholar] [CrossRef]
- Nishigawa, K.; Bando, E.; Nakano, M. Quantitative study of bite force during sleep associated bruxism. J. Oral Rehabil. 2001, 28, 485–491. [Google Scholar] [CrossRef]
- Hickl, V.; Strasser, T.; Schmid, A.; Rosentritt, M. Pull-off behavior of hand-cast, thermoformed, milled and 3D printed splints. Int. J. Prosthodont. 2022, preprint. [Google Scholar] [CrossRef]
- Rosentritt, M.; Behr, M.; Strasser, T.; Schmid, A. Pilot in-vitro study on insertion/removal performance of hand-cast, milled and 3D printed splints. J. Mech. Behav. Biomed. Mater. 2021, 121, 104612. [Google Scholar] [CrossRef]
- Lee, H.; Wang, J.; Park, S.-M.; Hong, S.; Kim, N. Analysis of excessive deformation behavior of a PMMA-touch screen panel laminated material in a high temperature condition. Korea-Aust. Rheol. J. 2011, 23, 195–204. [Google Scholar] [CrossRef]
- Dizon, J.R.C.; Espera, A.H.; Chen, Q.; Advincula, R.C. Mechanical characterization of 3D-printed polymers. Addit. Manuf. 2018, 20, 44–67. [Google Scholar] [CrossRef]
- Zohdi, N.; Yang, R.C. Material Anisotropy in Additively Manufactured Polymers and Polymer Composites: A Review. Polymers 2021, 13, 3368. [Google Scholar] [CrossRef]
- Monzón, M.; Ortega, Z.; Hernández, A.; Paz, R.; Ortega, F. Anisotropy of Photopolymer Parts Made by Digital Light Processing. Materials 2017, 10, 64. [Google Scholar] [CrossRef]
- Garcia, J.; Yang, Z.; Mongrain, R.; Leask, R.L.; Lachapelle, K. 3D printing materials and their use in medical education: A review of current technology and trends for the future. BMJ Simul. Technol. Enhanc. Learn. 2018, 4, 27–40. [Google Scholar] [CrossRef]
- Xu, Y.; Xepapadeas, A.B.; Koos, B.; Geis-Gerstorfer, J.; Li, P.; Spintzyk, S. Effect of post-rinsing time on the mechanical strength and cytotoxicity of a 3D printed orthodontic splint material. Dent. Mater. 2021, 37, e314–e327. [Google Scholar] [CrossRef]
- Hwangbo, N.-K.; Nam, N.-E.; Choi, J.-H.; Kim, J.-E. Effects of the Washing Time and Washing Solution on the Biocompatibility and Mechanical Properties of 3D Printed Dental Resin Materials. Polymers 2021, 13, 4410. [Google Scholar] [CrossRef]
- Wulff, J.; Schweikl, H.; Rosentritt, M. Cytotoxicity of printed resin-based splint materials. J. Dent. 2022, 120, 104097. [Google Scholar] [CrossRef]
- Lohbauer, U.; Rahiotis, C.; Krämer, N.; Petschelt, A.; Eliades, G. The effect of different light-curing units on fatigue behavior and degree of conversion of a resin composite. Dent. Mater. 2005, 21, 608–615. [Google Scholar] [CrossRef]
- Barszczewska-Rybarek, I.M. A Guide through the Dental Dimethacrylate Polymer Network Structural Characterization and Interpretation of Physico-Mechanical Properties. Materials 2019, 12, 4057. [Google Scholar] [CrossRef]
- Wulff, J.; Schmid, A.; Huber, C.; Rosentritt, M. Dynamic fatigue of 3D-printed splint materials. J. Mech. Behav. Biomed. Mater. 2021, 124, 104885. [Google Scholar] [CrossRef]
- Kim, D.; Shim, J.-S.; Lee, D.; Shin, S.-H.; Nam, N.-E.; Park, K.-H.; Shim, J.-S.; Kim, J.-E. Effects of Post-Curing Time on the Mechanical and Color Properties of Three-Dimensional Printed Crown and Bridge Materials. Polymers 2020, 12, 2762. [Google Scholar] [CrossRef]
- Rosentritt, M.; Krifka, S.; Preis, V.; Strasser, T. Dynamic fatigue of composite CAD/CAM materials. J. Mech. Behav. Biomed. Mater. 2019, 98, 311–316. [Google Scholar] [CrossRef]
- Huang, W.; Ren, L.; Cheng, Y.; Xu, M.; Luo, W.; Zhan, D.; Sano, H.; Fu, J. Evaluation of the Color Stability, Water Sorption, and Solubility of Current Resin Composites. Materials 2022, 15, 6710. [Google Scholar] [CrossRef]
- Lohbauer, U.; Belli, R.; Ferracane, J.L. Factors involved in mechanical fatigue degradation of dental resin composites. J. Dent. Res. 2013, 92, 584–591. [Google Scholar] [CrossRef]
- Prpic, V.; Spehar, F.; Stajdohar, D.; Bjelica, R.; Cimic, S.; Par, M. Mechanical Properties of 3D-Printed Occlusal Splint Materials. Dent. J. 2023, 11, 199. [Google Scholar] [CrossRef]

| Abbr. Text | Device/Material Protocol | Manufacturer LOT | |
|---|---|---|---|
| Printer | P30+ (digital light processing) | Straumann, Basel, Switzerland | |
| Orientation | 0° | ||
| 45° | |||
| 90° | |||
| Cleaning | AUTO | P Wash (isopropanol): pre-cleaning 3:10 min, cleaning 2:20 min, drying 1:30 min | Straumann, Basel, Switzerland |
| MAN | Pre-/Main-Clean (isopropanol): pre-cleaning 3:00 min, ultrasonic: 2:00 min, air-drying: 1:00 min | VOCO, Cuxhaven, Germany | |
| Post-polymerization | LED | P Cure: LED, 10 min, vacuum, UV-A: 400–315 nm; UV-B: 315–280 nm, heating | Straumann, Basel, Switzerland |
| XEN | Otoflash G171: 2 × 2000 Xenon flashes, 280–700 nm, maximum between 400–500 nm | NK-OPTIK, Baierbrunn, Germany | |
| Materials | M1 | Luxaprint OrthoPlus: >90% bisphenol A dimethacrylate, 385/405 nm, flexural strength ≥ 70 MPa, flexural modulus ≥ 1 GPa, Shore D ≥ 60 | DMG, Hamburg, Germany LOT 218479 |
| M2 | V-Print Splint: acrylate, Bis-EMA, TEGDMA, hydroxypropyl methacrylate, butylated hydroxytoluene, diphenyl(2,4,6-trimethylbenzoyl) phosphine oxide, 385 nm, flexural strength 75 MPa, flexural modulus ≥ 2.1 GPa, water uptake 27.7 μg/mm3, solubility < 0.1 μg/mm3 | VOCO, Cuxhaven, Germany LOT 2023138 |
| F | p-Value | |
|---|---|---|
| material | 2.668 | 0.103 |
| orientation | 100.342 | <0.001 |
| cleaning | 0.984 | 0.321 |
| polymerization | 356.934 | <0.001 |
| aging | 228.539 | <0.001 |
| material × position | 36.020 | <0.001 |
| material × cleaning | 8.985 | 0.003 |
| material × polymerization | 2.966 | 0.085 |
| material × aging | 92.072 | <0.001 |
| position × cleaning | 46.331 | <0.001 |
| position × polymerization | 6.678 | 0.001 |
| position × aging | 2.904 | 0.056 |
| cleaning × polymerization | 0.542 | 0.462 |
| cleaning × aging | 5.412 | 0.020 |
| polymerization × aging | 0.124 | 0.724 |
| material × position × cleaning | 28.301 | <0.001 |
| material × position × polymerization | 10.567 | <0.001 |
| material × position × aging | 2.274 | 0.104 |
| material × cleaning × polymerization | 25.823 | <0.001 |
| material × cleaning × aging | 0.650 | 0.420 |
| material × polymerization × aging | 0.026 | 0.872 |
| position × cleaning × polymerization | 1.688 | 0.186 |
| position × cleaning × aging | 3.345 | 0.036 |
| position × polymerization × aging | 4.367 | 0.013 |
| cleaning × polymerization × aging | 0.000 | 0.988 |
| material × position × cleaning × polymerization | 3.557 | 0.029 |
| material × position × cleaning × aging | 0.318 | 0.727 |
| material × position × polymerization × aging | 4.161 | 0.016 |
| material × cleaning × polymerization × aging | 0.945 | 0.331 |
| position × cleaning × polymerization × aging | 0.222 | 0.801 |
| material × position × cleaning × polymerization × aging | 1.055 | 0.349 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wulff, J.; Rauch, A.; Schmidt, M.B.; Rosentritt, M. Biaxial Flexural Strength of Printed Splint Materials. Materials 2024, 17, 1112. https://doi.org/10.3390/ma17051112
Wulff J, Rauch A, Schmidt MB, Rosentritt M. Biaxial Flexural Strength of Printed Splint Materials. Materials. 2024; 17(5):1112. https://doi.org/10.3390/ma17051112
Chicago/Turabian StyleWulff, Johann, Angelika Rauch, Michael Benno Schmidt, and Martin Rosentritt. 2024. "Biaxial Flexural Strength of Printed Splint Materials" Materials 17, no. 5: 1112. https://doi.org/10.3390/ma17051112






