Hot Isostatically Pressed Nano 3 mol% Yttria Partially Stabilised Zirconia: Effect on Mechanical Properties
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Specimen Preparation
2.3. Flexural Strength Testing
- P is the breaking load, in N;
- l is the test span, in mm;
- w is the width of the specimen, in mm;
- b is the thickness of the specimen, in mm.
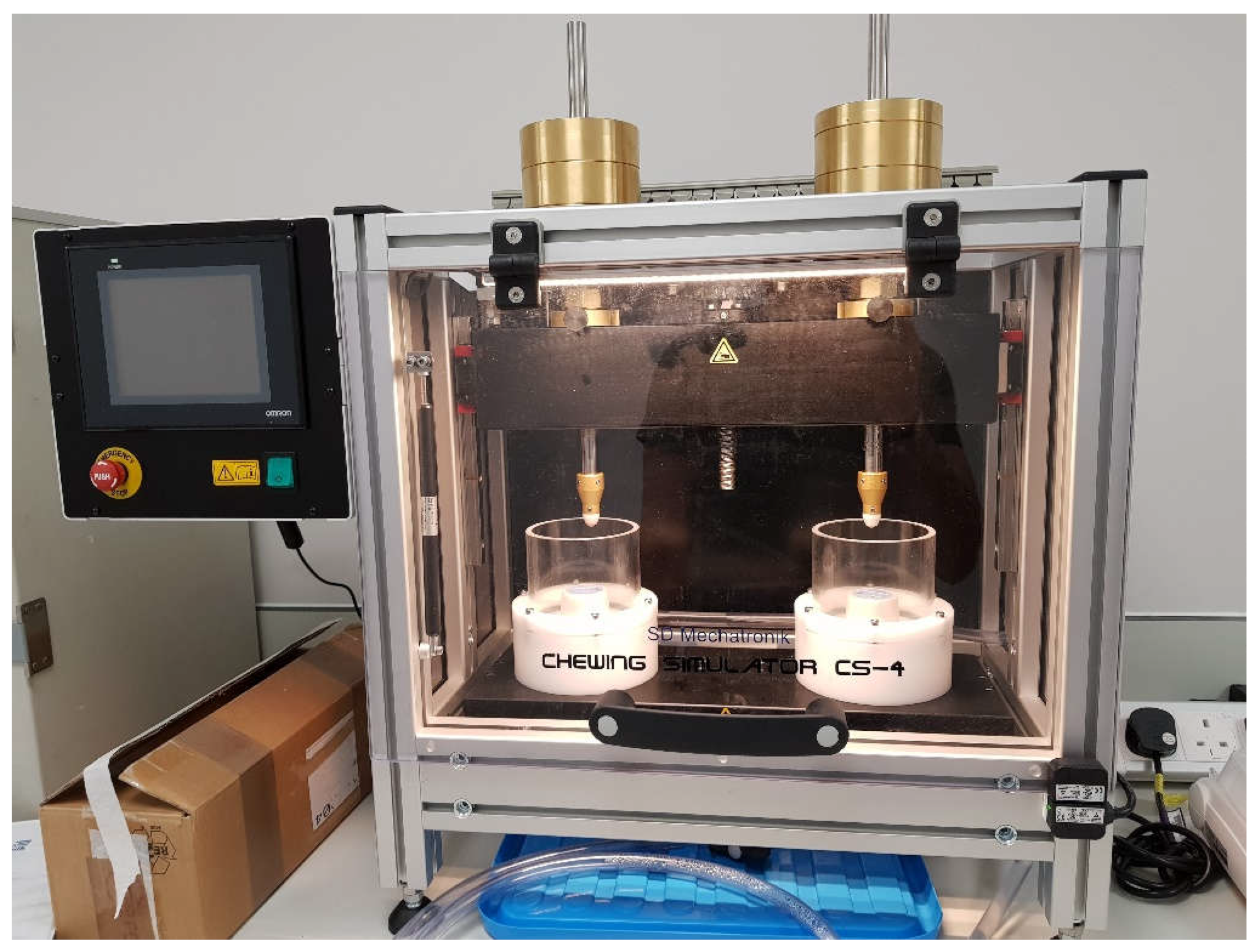
2.4. Chewing Simulation
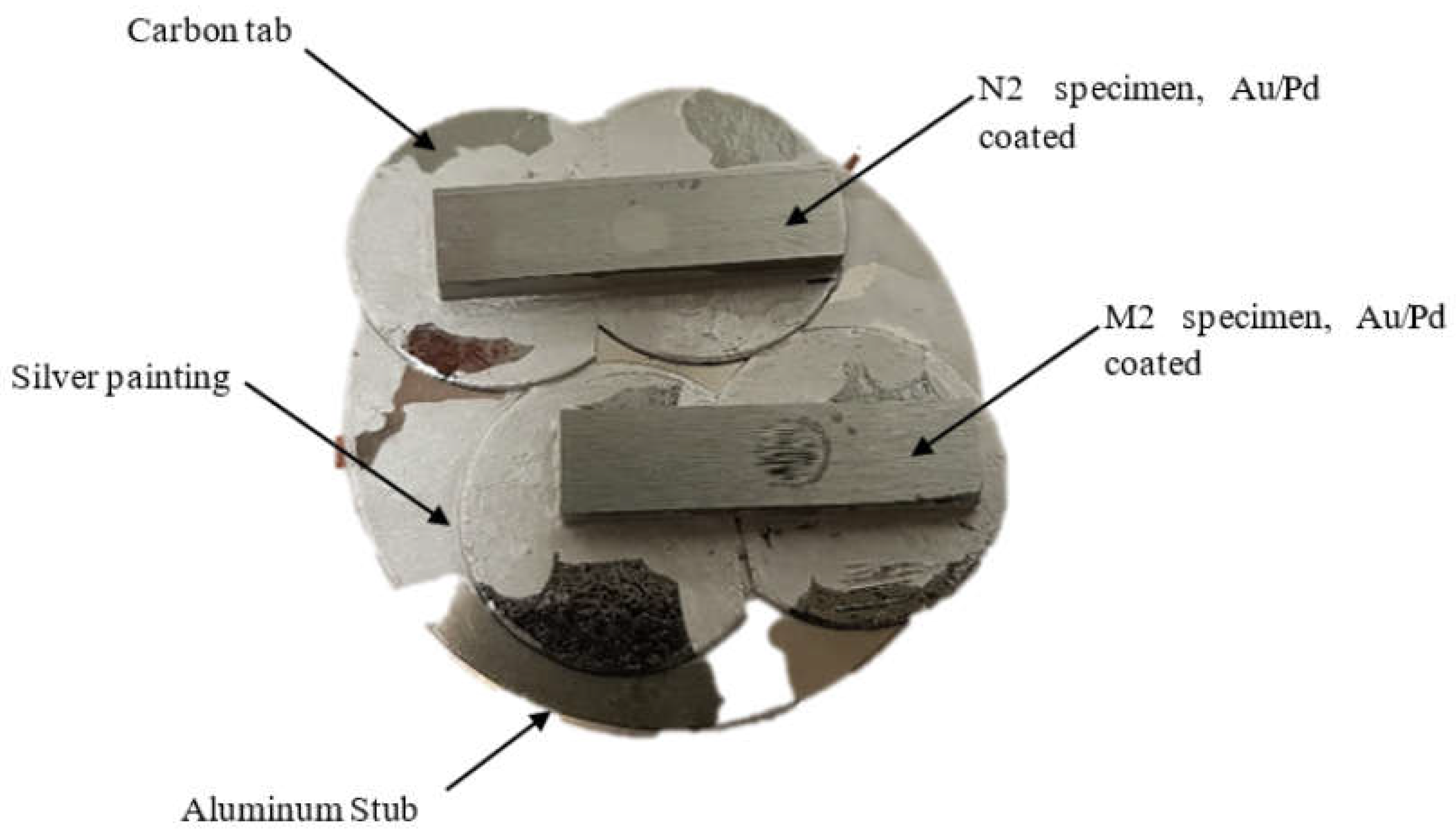
2.5. Scanning Electron Microscopy
2.6. Statistical Analysis
3. Results
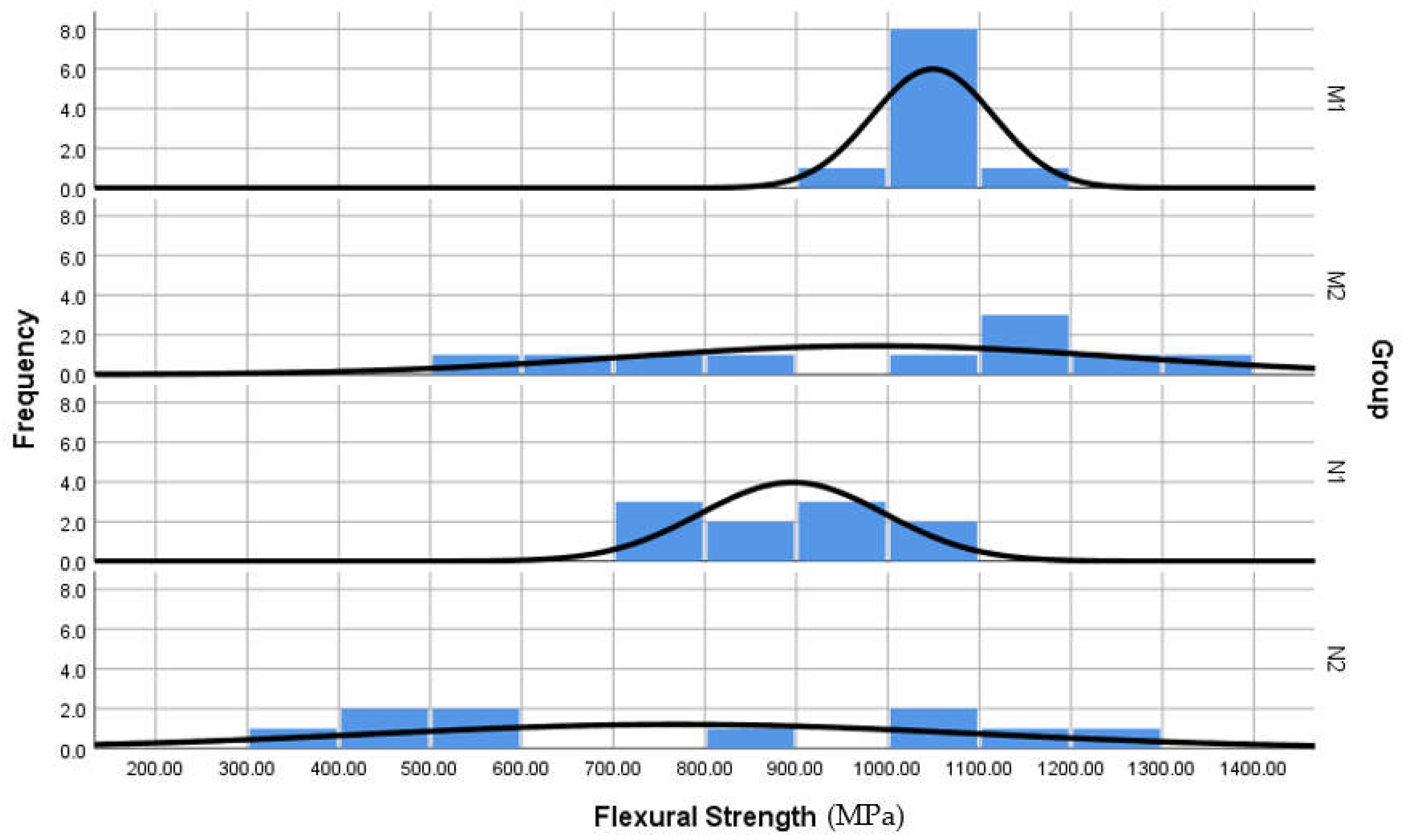
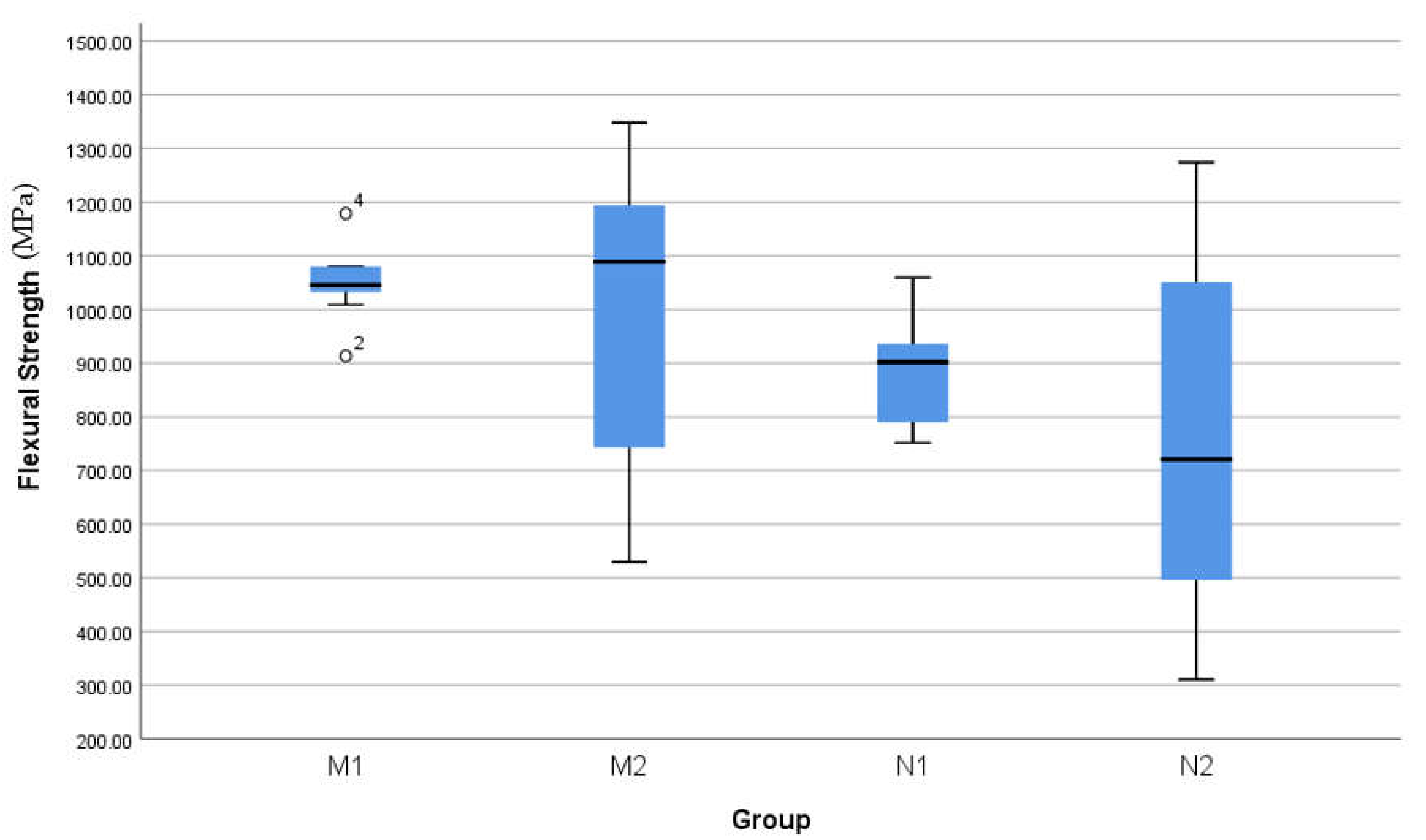
3.1. Flexural Strength
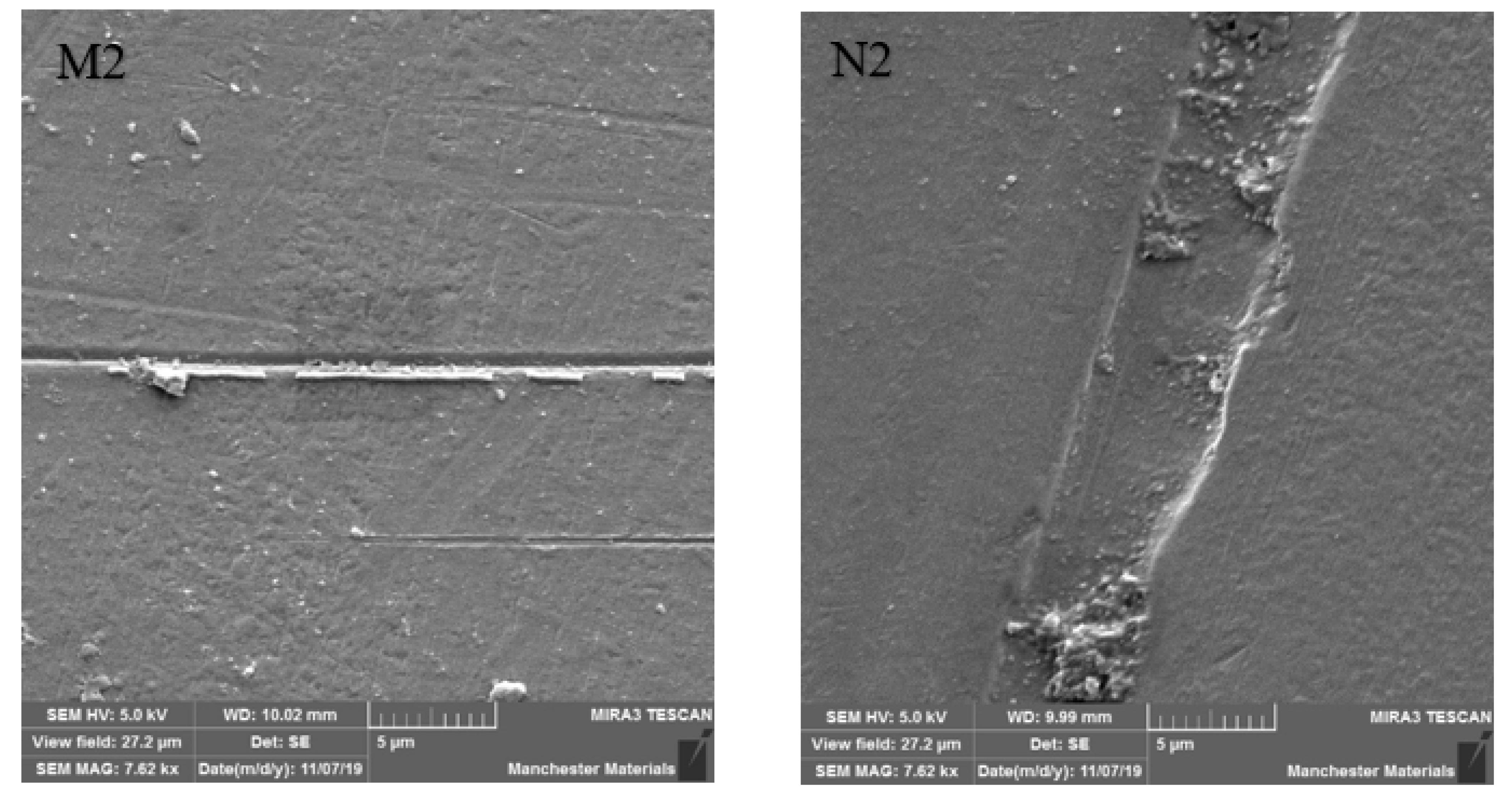
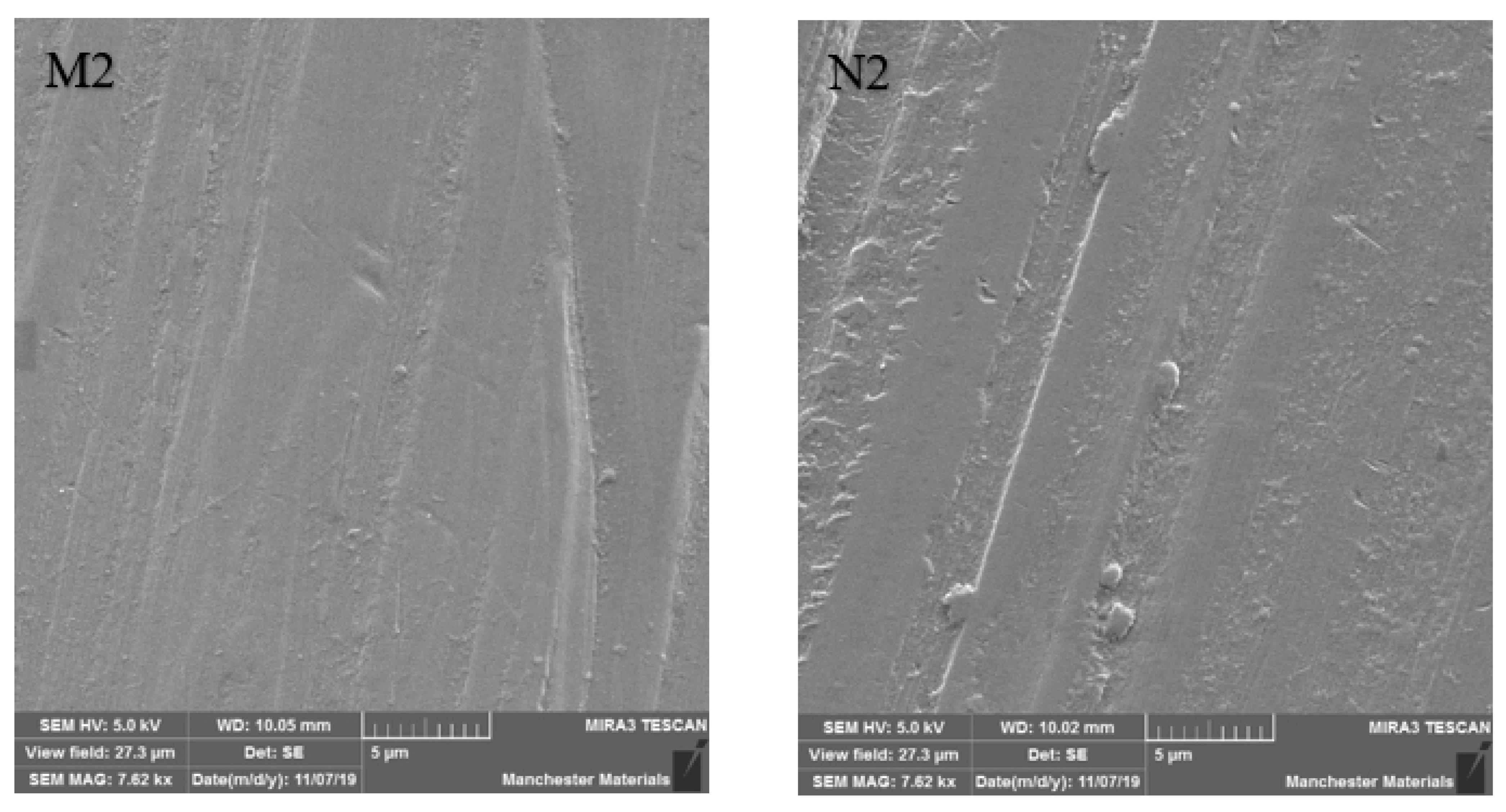
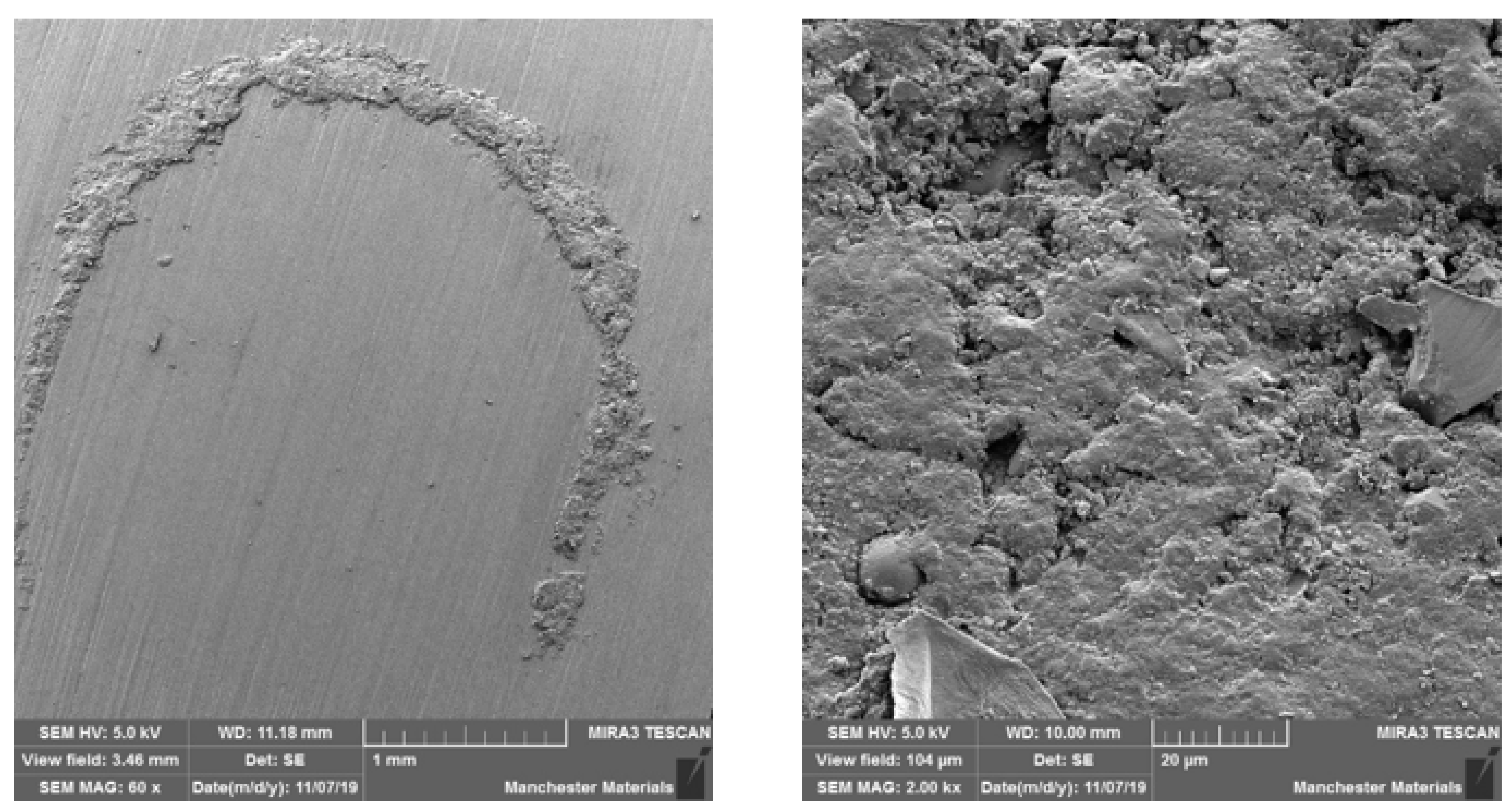
3.2. SEM Imaging
4. Discussion
5. Conclusions
- Conventional micro zirconia exhibited high flexural strength.
- Conventional micro zirconia has shown less particle debris around the impact point after loading, indicating higher structural integrity and a smoother surface, suggesting higher polishability.
- Nano HIP zirconia and conventional micro zirconia were affected significantly after cyclic loading, and are not recommended for use in bruxists.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alfawaz, Y.; Patil, S. Zirconia Crown as Single Unit Tooth Restoration: A Literature Review. J. Contemp. Dent. Pract. 2016, 17, 418–422. [Google Scholar] [CrossRef] [PubMed]
- Della Bona, A.; Pecho, O.E.; Alessandretti, R. Zirconia as a Dental Biomaterial. Materials 2015, 8, 4978–4991. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pilathadka, S.; Vahalová, D.; Vosáhlo, T. The Zirconia: A new dental ceramic material. An overview. Prague Med. Rep. 2007, 108, 5–12. [Google Scholar] [PubMed]
- Koutayas, S.O.; Kern, M. All-ceramic posts and cores: The state of the art. Quintessence Int. 1999, 30, 383–392. [Google Scholar] [PubMed]
- Agustin-Panadero, R.; Roman-Rodriguez, J.; Ferreiroa, A.; Sola-Ruiz, M.; Fons-Font, A. Zirconia in fixed prosthesis. A literature review. J. Clin. Exp. Dent. 2014, 6, e66–e73. [Google Scholar] [CrossRef]
- Helvey, G.A. Classification of Dental Ceramics. Inside Dent. 2013, 13, 62–76. [Google Scholar]
- Wood, D.L.; Nassau, K. Refractive index of cubic zirconia stabilized with yttria. Appl. Opt. 1982, 21, 2978–2981. [Google Scholar] [CrossRef]
- Burgess, J.O. Zirconia: The Material, Its Evolution, and Composition. Compend. Contin. Educ. Dent. 2018, 39, 4–8. [Google Scholar]
- Zhang, Y.; Lawn, B. Novel Zirconia Materials in Dentistry. J. Dent. Res. 2018, 97, 140–147. [Google Scholar] [CrossRef]
- Sedda, M.; Vichi, A.; Del Siena, F.; Louca, C.; Ferrari, M. Flexural resistance of Cerec CAD/CAM system ceramic blocks. Part 2: Outsourcing materials. Am. J. Dent. 2014, 27, 17–22. [Google Scholar]
- Denry, I.; Kelly, J.R. State of the art of zirconia for dental applications. Dent. Mater. 2008, 24, 299–307. [Google Scholar] [CrossRef]
- Aboushelib, M.N.; Kleverlaan, C.J.; Feilzer, A.J. Microtensile bond strength of different components of core veneered all-ceramic restorations: Part II: Zirconia veneering ceramics. Dent. Mater. 2006, 22, 857–863. [Google Scholar] [CrossRef]
- Vagkopoulou, T.; Koutayas, S.O.; Koidis, P.; Strub, J.R. Zirconia in dentistry: Part 1. Discovering the nature of an upcoming bioceramic. Eur. J. Esthet. Dent. 2009, 4, 130–151. [Google Scholar]
- Lucas, T.J.; Lawson, N.C.; Janowski, G.M.; Burgess, J.O. Effect of grain size on the monoclinic transformation, hardness, roughness, and modulus of aged partially stabilized zirconia. Dent. Mater. 2015, 31, 1487–1492. [Google Scholar] [CrossRef]
- Swab, J. Low temperature degradation of Y-TZP materials. J. Mater. Sci. 1991, 26, 6706–6714. [Google Scholar] [CrossRef]
- Cattani-Lorente, M.; Durual, S.; Amez-Droz, M.; Wiskott, H.A.; Scherrer, S.S. Hydrothermal degradation of a 3Y-TZP translucent dental ceramic: A comparison of numerical predictions with experimental data after 2 years of aging. Dent. Mater. 2016, 32, 394–402. [Google Scholar] [CrossRef]
- Lascalea, G.; Lamas, D.; Pérez, L.; Cabanillas, E.; de Reca, N.W. Synthesis of ZrO2–15 mol% CeO2 nanopowders by a pH-controlled nitrate–glycine process. Mater. Lett. 2004, 58, 2456–2460. [Google Scholar] [CrossRef]
- León, A.B.; Morikawa, Y.; Kawahara, M.; Mayo, M.J. Fracture toughness of nanocrystalline tetragonal zirconia with low yttria content. Acta Mater. 2002, 50, 4555–4562. [Google Scholar] [CrossRef]
- Meyers, M.A.; Mishra, A.; Benson, D.J. Mechanical properties of nanocrystalline materials. Prog. Mater. Sci. 2006, 51, 427–556. [Google Scholar] [CrossRef]
- Barinov, S.M.; Ponomarev, V.F.; Shevchenko, V.Y.; Skawran, D. Effects of post-hot isostatic pressing on mechanical properties of presintered alumina ceramics. J. Mater. Sci. 1996, 31, 5791–5795. [Google Scholar] [CrossRef]
- Scherrer, S.S.; Cattani-Lorente, M.; Yoon, S.; Karvonen, L.; Pokrant, S.; Rothbrust, F.; Kuebler, J. Post-hot isostatic pressing: A healing treatment for process related defects and laboratory grinding damage of dental zirconia? Dent. Mater. 2013, 29, e180–e190. [Google Scholar] [CrossRef] [PubMed]
- Gupta, T.K. Crack healing and strengthening of thermally shocked alumina. J. Am. Ceram. Soc. 1976, 59, 259–262. [Google Scholar] [CrossRef]
- Jun, L.; Zheng, Z.; Ding, H.; Jin, Z.H. Preliminary study of the crack healing and strength recovery of Al2O3-matrix composites. Fatigue Fract. Eng. Mater. Struct. 2004, 27, 89–97. [Google Scholar] [CrossRef]
- Dakskobler, A.; Jevnikar, P.; Oblak, Č.; Kosmač, T. The processing-related fracture resistance and reliability of root dental posts made from Y-TZP. J. Eur. Ceram. Soc. 2007, 27, 1565–1570. [Google Scholar] [CrossRef]
- Chaim, R.; Levin, M.; Shlayer, A.; Estournès, C. Sintering and densification of nanocrystalline ceramic oxide powders: A review. Adv. Appl. Ceram. 2008, 107, 159–169. [Google Scholar] [CrossRef] [Green Version]
- Piconi, C.; Maccauro, G. Zirconia as a ceramic biomaterial. Biomaterials 1999, 20, 1–25. [Google Scholar] [CrossRef]
- Shukla, S.; Seal, S.; Vij, R.; Bandyopadhyay, S.; Rahman, Z. Effect of Nanocrystallite Morphology on the Metastable Tetragonal Phase Stabilization in Zirconia. Nano Lett. 2002, 2, 989–993. [Google Scholar] [CrossRef]
- Levartovsky, S.; Pilo, R.; Shadur, A.; Matalon, S.; Winocur, E. Complete rehabilitation of patients with bruxism by veneered and non-veneered zirconia restorations with an increased vertical dimension of occlusion: An observational case-series study. J. Prosthodont. Res. 2019, 63, 440–446. [Google Scholar] [CrossRef]
- Koenig, V.; Wulfman, C.; Bekaert, S.; Dupont, N.; Le Goff, S.; Eldafrawy, M.; Vanheusden, A.; Mainjot, A. Clinical behavior of second-generation zirconia monolithic posterior restorations: Two-year results of a prospective study with Ex vivo analyses including patients with bruxism clinical signs. J. Dent. 2019, 91, 103229. [Google Scholar] [CrossRef]
- Lan, T.-H.; Pan, C.-Y.; Liu, P.-H.; Chou, M.M.C. Fracture Resistance of Monolithic Zirconia Crowns in Implant Prostheses in Patients with Bruxism. Materials 2019, 12, 1623. [Google Scholar] [CrossRef] [Green Version]
- Lutz, F.; Krejci, I. Mesio-occlusodistal amalgam restorations: Quantitative in vivo data up to 4 years. A data base for the development of amalgam substitutes. Quintessence Int. 1994, 25, 185–190. [Google Scholar]
- Mundt, T.; Heinemann, F.; Schankath, C.; Schwahn, C.; Biffar, R. Retrospective and clinical evaluation of retrievable, tooth-implant supported zirconia-ceramic restorations. Acta Odontol. Scand. 2013, 71, 1326–1334. [Google Scholar] [CrossRef]
- Masaki, T. Mechanical Properties of Y2O3-Stabilized Tetragonal ZrO2 Polycrystals after Ageing at High Temperature. J. Am. Ceram. Soc. 1986, 69, 519–522. [Google Scholar] [CrossRef]
- Burgess, J.; Janyavula, S.; Lawson, N.; Lucas, T.; Cakir, D. Enamel Wear Opposing Polished and Aged Zirconia. Oper. Dent. 2014, 39, 189–194. [Google Scholar] [CrossRef]
- Passos, S.P.; Torrealba, Y.; Major, P.; Linke, B.; Flores-Mir, C.; Nychka, J.A. In vitro wear behavior of zirconia opposing enamel: A systematic review. J. Prosthodont. 2014, 23, 593–601. [Google Scholar] [CrossRef]
- BSI EN ISO 6872:2015; Dentistry—Ceramic Materials. British Standards Institution (BSI): London, UK, 2015.
- Philipp, A.; Fischer, J.; Hämmerle, C.H.F.; Sailer, I. Novel ceria-stabilized tetragonal zirconia/alumina nanocomposite as framework material for posterior fixed dental prostheses: Preliminary results of a prospective case series at 1 year of function. Quintessence Int. 2010, 41, 313–319. [Google Scholar]
- Pelaez, J.; Cogolludo, P.G.; Serrano, B.; Serrano, J.F.L.; Suarez, M.J. A four-year prospective clinical evaluation of zirconia and metal-ceramic posterior fixed dental prostheses. Int. J. Prosthodont. 2012, 25, 451–458. [Google Scholar]
- Rinke, S.; Gersdorff, N.; Lange, K.; Roediger, M. Prospective Evaluation of Zirconia Posterior Fixed Partial Dentures: 7-Year Clinical Results. Int. J. Prosthodont. 2013, 26, 164–171. [Google Scholar] [CrossRef] [Green Version]
- Rinke, S.; Wehle, J.; Schulz, X.; Bürgers, R.; Rödiger, M. Prospective Evaluation of Posterior Fixed Zirconia Dental Prostheses: 10-Year Clinical Results. Int. J. Prosthodont. 2018, 31, 35–42. [Google Scholar] [CrossRef]
- Roediger, M.; Gersdorff, N.; Huels, A.; Rinke, S. Prospective evaluation of zirconia posterior fixed partial dentures: Four-year clinical results. Int. J. Prosthodont. 2010, 23, 141–148. [Google Scholar]
- Burke, F.; Crisp, R.; Cowan, A.; Lamb, J.; Thompson, O.; Tulloch, N. Five-year clinical evaluation of zirconia-based bridges in patients in UK general dental practices. J. Dent. 2013, 41, 992–999. [Google Scholar] [CrossRef] [PubMed]
- Sailer, I.; Balmer, M.; Hüsler, J.; Hämmerle, C.H.F.; Känel, S.; Thoma, D.S. 10-year randomized trial (RCT) of zirconia-ceramic and metal-ceramic fixed dental prostheses. J. Dent. 2018, 76, 32–39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ebeid, K.; Wille, S.; Salah, T.; Wahsh, M.; Zohdy, M.; Kern, M. Bond strength of resin cement to zirconia treated in pre-sintered stage. J. Mech. Behav. Biomed. Mater. 2018, 86, 84–88. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.-K.; Bae, H.E.-K.; Shim, J.-S.; Lee, K.-W. The influence of ceramic surface treatments on the tensile bond strength of composite resin to all-ceramic coping materials. J. Prosthet. Dent. 2005, 94, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Sagen, M.A.; Kvam, K.; Ruyter, E.I.; Rønold, H.J. Debonding mechanism of zirconia and lithium disilicate resin cemented to dentin. Acta Biomater. Odontol. Scand. 2019, 5, 22–29. [Google Scholar] [CrossRef]



| CeramaZirc Nano HIP | CeramaZirc | |
|---|---|---|
| Flexural strength [MPa] | 1400 | 850 |
| Compressive strength [MPa] | 2100 | |
| Fracture toughness Kıᴄ [MPa/m²] | 8 | |
| Thermal expansion coefficient [×10⁻⁶/°C] | 10 | |
| N | Mean (MPa) | Std. Deviation | Std. Error | |
|---|---|---|---|---|
| M1 Group | 10 | 1048.9 | 66.5 | 21 |
| M2 Group | 10 | 985 | 276.2 | 87.3 |
| N1 Group | 10 | 895.8 | 100.3 | 31.7 |
| N2 Group | 10 | 770 | 331.8 | 104.9 |
| Total | 40 | 924.9 | 240 | 37.9 |
| Sig. (2-Tailed) | ||
|---|---|---|
| Paired t | M1-M2 | 0.506 |
| Paired t | N1-N2 | 0.286 |
| Unpaired t | M1-N1 | 0.001 * |
| Unpaired t | M2-N2 | 0.133 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alsulimani, O.; Satterthwaite, J.; Silikas, N. Hot Isostatically Pressed Nano 3 mol% Yttria Partially Stabilised Zirconia: Effect on Mechanical Properties. Materials 2023, 16, 341. https://doi.org/10.3390/ma16010341
Alsulimani O, Satterthwaite J, Silikas N. Hot Isostatically Pressed Nano 3 mol% Yttria Partially Stabilised Zirconia: Effect on Mechanical Properties. Materials. 2023; 16(1):341. https://doi.org/10.3390/ma16010341
Chicago/Turabian StyleAlsulimani, Osamah, Julian Satterthwaite, and Nick Silikas. 2023. "Hot Isostatically Pressed Nano 3 mol% Yttria Partially Stabilised Zirconia: Effect on Mechanical Properties" Materials 16, no. 1: 341. https://doi.org/10.3390/ma16010341





