Optimum Design of a Transportation Scheme for Healthcare Supply Chain Management: The Effect of Energy Consumption
Abstract
:1. Introduction
2. Literature Review
2.1. Healthcare Supply Chain Management
2.2. Sustainable Energy-Efficient Supply Chain Management (SEESCM)
2.3. Green Supply Chain Management
2.4. Traditional Supply Chain Management with a Single Objective
- Not Applicable (NA) means that the concept was not studied in the specified paper;
- Applicable means that the concept was covered by the specified paper.
3. Problem Definition, Notation, and Assumptions
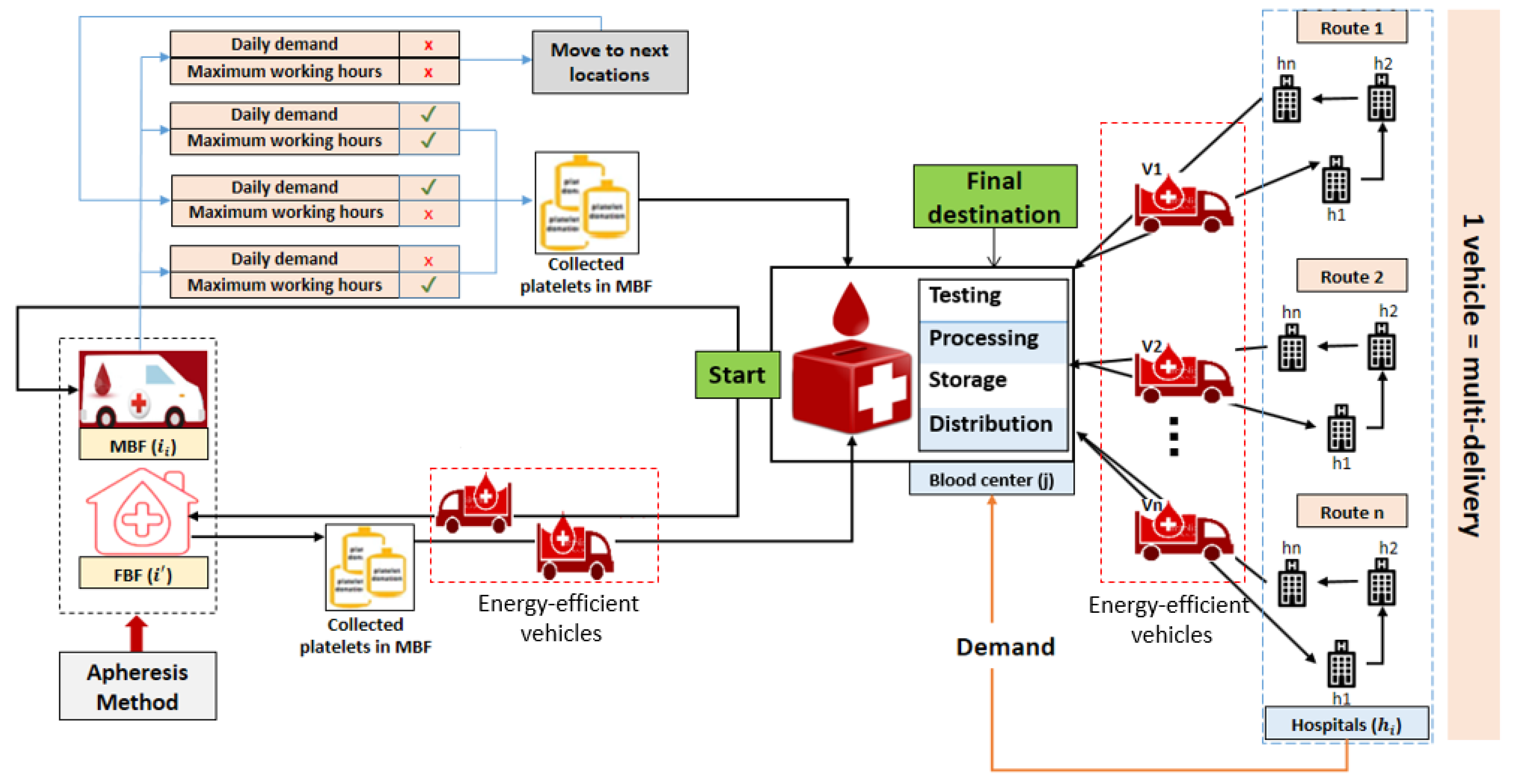
3.1. Problem Definition
3.2. Notation
3.3. Assumptions
- The effect of energy is considered with optimal energy consumption in a healthcare supply chain [51] for blood platelets.
- The speed of each vehicle is considered to be fixed [57]. Thus, energy consumption is maintained, and each vehicle starts and ends its trip at the starting point [58]. The distances between the nodes of the supply chain are known, and the number, locations, and capacities of the MBF, FBF, blood center, and delivery vehicles for optimal energy consumption are known [59].
- Only blood platelets are considered in this study, and their lifetime L is known and limited [60]. The age a of the platelet units is known (less than three days: young; more than three days: old) [61]. Only a mobile blood facility is able to move from one site to another in the next planning period t, and its movement to another site depends on the working hours of the employees and whether the required quantity is achieved [62].
- The transportation costs, including carbon emissions and energy consumption [63], are proportional to the distance traveled.
- Blood wastage refers to the rate of lost blood during the testing process. Thus, wastage costs are incurred. The expired quantity of blood ( and in blood centers and fixed blood facilities, respectively) imposes extra costs. It is assumed that the volume of 1 unit of blood platelets is fixed and equal to 180 mL.
4. Model Formulation
4.1. Transportation Costs Due to the Effect of Energy
4.2. Inventory Holding Costs
4.3. Shortage Costs
4.4. Wastage Costs
4.5. Perishable Blood Costs
4.6. Operational Costs
4.7. Establishment Costs
4.8. Constraints
4.9. Objective Function
4.10. Solution Methodology
4.11. Numerical Experiments
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| MBF | Mobile Blood Facility |
| FBF | Fixed Blood Facility |
| BC | Blood Cenetr |
Appendix A
| I | mobile blood facilities, |
| K | fixed blood facilities, |
| J | blood center, |
| H | hospitals, |
| V | vehicles indexed by |
| C | capacities |
| T | planning periods, |
| R | routes indexed by with |
| A | age of platelets, |
| capacity with | |
| i | |
| fixed transportation costs under efficient-energy consumption per km ($/km) | |
| L | lifetime of platelets (days) |
| carbon emission costs ($/gr of CO) | |
| holding costs of the blood with age a in the blood center during the planning | |
| period t ($/unit/unit time) | |
| holding costs at fixed blood facilities during the planning period t ($/unit/unit time) | |
| penalty costs for shortage in blood age a at the blood center during the planning | |
| period t ($/unit/unit time) | |
| unit cost of expired blood at a blood center ($/unit/unit time) | |
| cost of one expired blood unit at a fixed blood facility ($/unit/unit time) | |
| unit production costs of platelets at blood center ($/unit) | |
| operational cost of platelets at mobile blood facility ($/unit) | |
| operating cost of platelets at fixed blood facility ($/unit) | |
| cost of operating the apheresis machine at blood center ($/unit) | |
| establishment costs of a fixed blood facility ($/setup) | |
| establishment costs of a mobile blood facility ($/setup) | |
| setup costs of delivery vehicle with capacity ($/setup) | |
| quantity of carbon emitted by the vehicle per km (gr of CO / km) | |
| distance between a fixed blood facility and blood center (km) | |
| total distance a mobile blood facility travel during the planning period t to collect the platelets (km) | |
| and deliver them to the blood center (km) | |
| total distance a vehicle travel during the planning period t in order to diffuse the platelets to all the | |
| demand points (km) | |
| distance between location and location (km) | |
| wasted blood platelets rate at blood center during production process | |
| outdated blood platelets rate at blood center | |
| expired blood platelets rate at a fixed blood facility | |
| quantity of demand of hospitals (unit/unit time) | |
| demand of blood center (unit/unit time) | |
| M | very large number |
| transported quantity of blood from a fixed blood facility to a blood center in period t (unit/unit time) | |
| collected quantity of blood in a fixed blood facility in period t (unit/unit time) | |
| shipped quantity of blood from a mobile blood facility to a blood center (unit/unit time) | |
| collected quantity of blood in a blood center in period t (unit/unit time) | |
| quantity of blood to be transported from the blood center to the demand points (unit/unit time) | |
| shortage quantity of blood age a at the blood center during the planning period t (unit/unit time) | |
| maximum quantity of shortage allowed (unit/unit time) | |
| wasted quantity of blood (unit/unit time) | |
| expired quantity of blood at blood center (unit/unit time) | |
| quantity of expired blood units at fixed blood facility (unit/unit time) | |
| produced quantity of blood at the blood center during the planning period t (unit/unit time) | |
| inventory level at a fixed blood facility during the planning period t (unit/unit time) | |
| inventory level at a blood center during the period t (unit/unit time) |
References
- Holinstat, M. Normal platelet function. Cancer Metastasis Rev. 2017, 36, 195–198. [Google Scholar] [CrossRef] [PubMed]
- Nahmias, S. Perishable inventory theory: A review. Oper. Res. 1982, 30, 680–708. [Google Scholar] [CrossRef] [PubMed]
- Sha, Y.; Huang, J. The multi-period location-allocation problem of engineering emergency blood supply systems. Syst. Eng. Procedia 2012, 5, 21–28. [Google Scholar] [CrossRef]
- Jabbarzadeh, A.; Fahimnia, B.; Seuring, S. Dynamic supply chain network design for the supply of blood in disasters: A robust model with real world application. Trans. Res. Part E Logist. Transp. Rev. 2014, 70, 225–244. [Google Scholar] [CrossRef]
- Katsaliaki, K.; Mustafee, N.; Kumar, S. A game-based approach towards facilitating decision making for perishable products: An example of blood supply chain. Exp. Syst. Appl. 2014, 41, 4043–4059. [Google Scholar] [CrossRef] [Green Version]
- Duan, Q.; Liao, T.W. Optimization of blood supply chain with shortened shelf lives and ABO compatibility. Int. J. Prod. Econ. 2014, 153, 113–129. [Google Scholar] [CrossRef]
- Arvan, M.; Tavakkoli-Moghaddam, R.; Abdollahi, M. Designing a bi-objective and multi-product supply chain network for the supply of blood. Uncertain Supply Chain Manag. 2015, 3, 57–68. [Google Scholar] [CrossRef]
- Giannakis, M.; Papadopoulos, T. Supply chain sustainability: A risk management approach. Int. J. Prod. Econ. 2016, 171, 455–470. [Google Scholar] [CrossRef]
- Osorio, A.F.; Brailsford, S.C.; Smith, H.K.; Forero-Matiz, S.P.; Camacho-Rodríguez, B.A. Simulation-optimization model for production planning in the blood supply chain. Healthc. Manag. Sci. 2017, 20, 548–564. [Google Scholar] [CrossRef]
- Zahiri, B.; Pishvaee, M.S. Blood supply chain network design considering blood group compatibility under uncertainty. Int. J. Prod. Res. 2017, 55, 2013–2033. [Google Scholar] [CrossRef]
- Ramezanian, R.; Behboodi, Z. Blood supply chain network design under uncertainties in supply and demand considering social aspects. Trans. Res. Part E Logist. Transp. Rev. 2017, 104, 69–82. [Google Scholar] [CrossRef]
- Paydar, M.M.; Babaveisi, V.; Safaei, A.S. An engine oil closed-loop supply chain design considering collection risk. Comput. Chem. Eng. 2017, 104, 38–55. [Google Scholar] [CrossRef]
- Najafi, M.; Ahmadi, A.; Zolfagharinia, H. Blood inventory management in hospitals: Considering supply and demand uncertainty and blood transshipment possibility. Oper. Res. Health Care 2017, 15, 43–56. [Google Scholar] [CrossRef]
- Ensafian, H.; Yaghoubi, S. Robust optimization model for integrated procurement, production and distribution in platelet supply chain. Trans. Res. Part E Logist. Transp. Rev. 2017, 103, 32–55. [Google Scholar] [CrossRef]
- Hosseinifard, Z.; Abbasi, B. The inventory centralization impacts on sustainability of the blood supply chain. Comput. Oper. Res. 2018, 89, 206–212. [Google Scholar] [CrossRef]
- Samani, M.R.G.; Torabi, S.A.; Hosseini-Motlagh, S.M. Integrated blood supply chain planning for disaster relief. Int. J. Disaster Risk Reduct. 2018, 27, 168–188. [Google Scholar] [CrossRef]
- Eskandari-Khanghahi, M.; Tavakkoli-Moghaddam, R.; Taleizadeh, A.A.; Amin, S.H. Designing and optimizing a sustainable supply chain network for a blood platelet bank under uncertainty. Eng. Appl. Artif. Intell. 2018, 71, 236–250. [Google Scholar] [CrossRef]
- Hamdan, B.; Diabat, A. A two-stage multi-echelon stochastic blood supply chain problem. Comput. Oper. Res. 2019, 101, 130–143. [Google Scholar] [CrossRef]
- Beamon, B.M. Sustainability and the future of supply chain management. Oper. Supply Chain Manag. 2008, 1, 4–18. [Google Scholar] [CrossRef]
- Rentizelas, A.A.; Tolis, A.J.; Tatsiopoulos, I.P. Logistics issues of biomass: The storage problem and the multi-biomass supply chain. Renew. Sustain. Energy Rev. 2009, 13, 887–894. [Google Scholar] [CrossRef] [Green Version]
- Halldórsson, Á.; Kovács, G. The sustainable agenda and energy efficiency: Logistics solutions and supply chains in times of climate change. Int. J. Phys. Distrib. Logist. Manag. 2010, 40, 5–13. [Google Scholar] [CrossRef]
- Gold, S.; Seuring, S. Supply chain and logistics issues of bio-energy production. J. Clean. Prod. 2011, 19, 32–42. [Google Scholar] [CrossRef]
- Pan, S.Y.; Du, M.A.; Huang, I.T.; Liu, I.H.; Chang, E.; Chiang, P.C. Strategies on implementation of waste-to-energy (WTE) supply chain for circular economy system: A review. J. Clean. Prod. 2015, 108, 409–421. [Google Scholar] [CrossRef]
- Luthra, S.; Mangla, S.K.; Xu, L.; Diabat, A. Using AHP to evaluate barriers in adopting sustainable consumption and production initiatives in a supply chain. Int. J. Prod. Econ. 2016, 181, 342–349. [Google Scholar] [CrossRef]
- Hong, J.; Shen, Q.; Xue, F. A multi-regional structural path analysis of the energy supply chain in China’s construction industry. Energy Policy 2016, 92, 56–68. [Google Scholar] [CrossRef]
- Marzband, M.; Ghazimirsaeid, S.S.; Uppal, H.; Fernando, T. A real-time evaluation of energy management systems for smart hybrid home Microgrids. Electr. Power Syst. Res. 2017, 143, 624–633. [Google Scholar] [CrossRef]
- Aziziankohan, A.; Jolai, F.; Khalilzadeh, M.; Soltani, R.; Tavakkoli-Moghaddam, R. Green supply chain management using the queuing theory to handle congestion and reduce energy consumption and emissions from supply chain transportation fleet. J. Ind. Eng. Manag. 2017, 10, 213–236. [Google Scholar] [CrossRef]
- Centobelli, P.; Cerchione, R.; Esposito, E. Environmental sustainability and energy-efficient supply chain management: A review of research trends and proposed guidelines. Energies 2018, 11, 275. [Google Scholar] [CrossRef]
- Singh, R.; Centobelli, P.; Cerchione, R. Evaluating Partnerships in Sustainability-Oriented Food Supply Chain: A Five-Stage Performance Measurement Model. Energies 2018, 11, 3473. [Google Scholar] [Green Version]
- Sarkar, M.; Sarkar, B.; Iqbal, M. Effect of Energy and Failure Rate in a Multi-Item Smart Production System. Energies 2018, 11, 2958. [Google Scholar] [CrossRef]
- Sarkar, B.; Omair, M.; Choi, S.B. A multi-objective optimization of energy, economic, and carbon emission in a production model under sustainable supply chain management. Appl. Sci. 2018, 8, 1744. [Google Scholar] [CrossRef]
- Marchi, B.; Zanoni, S.; Ferretti, I.; Zavanella, L. Stimulating investments in energy efficiency through supply chain integration. Energies 2018, 11, 858. [Google Scholar] [CrossRef]
- Fontes, C.H.d.O.; Freires, F.G.M. Sustainable and renewable energy supply chain: A system dynamics overview. Renew. Sustain. Energy Rev. 2018, 82, 247–259. [Google Scholar]
- Zhu, Q.; Sarkis, J.; Lai, K.h. Green supply chain management: Pressures, practices and performance within the Chinese automobile industry. J. Clean. Prod. 2007, 15, 1041–1052. [Google Scholar] [CrossRef]
- Srivastava, S.K. Green supply-chain management: A state-of-the-art literature review. Int. J. Manag. Rev. 2007, 9, 53–80. [Google Scholar] [CrossRef]
- Yeh, W.C.; Chuang, M.C. Using multi-objective genetic algorithm for partner selection in green supply chain problems. Exp. Syst. Appl. 2011, 38, 4244–4253. [Google Scholar] [CrossRef]
- Hua, G.; Cheng, T.; Wang, S. Managing carbon footprints in inventory management. Int. J. Prod. Econ. 2011, 132, 178–185. [Google Scholar] [CrossRef]
- Kumar, S.; Chattopadhyaya, S.; Sharma, V. Green supply chain management: A case study from Indian electrical and electronics industry. Int. J. Soft Comput. Eng. 2012, 1, 275–281. [Google Scholar]
- Pan, S.; Ballot, E.; Fontane, F. The reduction of greenhouse gas emissions from freight transport by pooling supply chains. Int. J. Prod. Econ. 2013, 143, 86–94. [Google Scholar] [CrossRef]
- Bazan, E.; Jaber, M.Y.; Zanoni, S. Supply chain models with greenhouse gases emissions, energy usage and different coordination decisions. Appl. Math. Model. 2015, 39, 5131–5151. [Google Scholar] [CrossRef]
- Ahmed, W.; Sarkar, B. Impact of carbon emissions in a sustainable supply chain management for a second generation biofuel. J. Clean. Prod. 2018, 186, 807–820. [Google Scholar] [CrossRef]
- Sarkar, B. A production-inventory model with probabilistic deterioration in two-echelon supply chain management. Appl. Math. Model. 2013, 37, 3138–3151. [Google Scholar] [CrossRef]
- Sarkar, B.; Ganguly, B.; Sarkar, M.; Pareek, S. Effect of variable transportation and carbon emission in a three-echelon supply chain model. Trans. Res. Part E Logist. Transp. Rev. 2016, 91, 112–128. [Google Scholar] [CrossRef]
- Habib, M.S.; Sarkar, B. An integrated location-allocation model for temporary disaster debris management under an uncertain environment. Sustainability 2017, 9, 716. [Google Scholar] [CrossRef]
- Sarkar, B.; Shaw, B.K.; Kim, T.; Sarkar, M.; Shin, D. An integrated inventory model with variable transportation cost, two-stage inspection, and defective items. J. Ind. Manag. Opt. 2017, 13, 1975–1990. [Google Scholar] [CrossRef]
- Feng, X.; Moon, I.; Ryu, K. Warehouse capacity sharing via transshipment for an integrated two-echelon supply chain. Trans. Res. Part E Logist. Transp. Rev. 2017, 104, 17–35. [Google Scholar] [CrossRef]
- Sarkar, B.; Ahmed, W.; Kim, N. Joint effects of variable carbon emission cost and multi-delay-in-payments under single-setup-multiple-delivery policy in a global sustainable supply chain. J. Clean. Prod. 2018, 185, 421–445. [Google Scholar] [CrossRef]
- Shi, X.; Zhang, X.; Dong, C.; Wen, S. Economic performance and emission reduction of supply chains in different power structures: Perspective of sustainable investment. Energies 2018, 11, 983. [Google Scholar] [CrossRef]
- Iqbal, M.W.; Sarkar, B. Recycling of lifetime dependent deteriorated products through different supply chains. RAIRO Oper. Res. 2019, 53, 129–156. [Google Scholar] [CrossRef]
- Mishra, U.; Wu, J.Z.; Chiu, A.S.F. Effects of Carbon-Emission and Setup Cost Reduction in a Sustainable Electrical Energy Supply Chain Inventory System. Energies 2019, 12, 1226. [Google Scholar] [CrossRef]
- Sarkar, B.; Mahapatra, A.S. Periodic review fuzzy inventory model with variable lead time and fuzzy demand. Int. Trans. Oper. Res. 2017, 24, 1197–1227. [Google Scholar] [CrossRef]
- Sarkar, B.; Ullah, M.; Kim, N. Environmental and economic assessment of closed-loop supply chain with remanufacturing and returnable transport items. Comput. Ind. Eng. 2017, 111, 148–163. [Google Scholar] [CrossRef]
- Malik, A.I.; Sarkar, B. Coordinating Supply-Chain Management under Stochastic Fuzzy Environment and Lead-Time Reduction. Mathematics 2019, 7, 480. [Google Scholar] [CrossRef]
- Shin, D.; Guchhait, R.; Sarkar, B.; Mittal, M. Controllable lead time, service level constraint, and transportation discounts in a continuous review inventory model. RAIRO Oper. Res. 2016, 50, 921–934. [Google Scholar] [CrossRef]
- Sarkar, B.; Tayyab, M.; Kim, N.; Habib, M.S. Optimal production delivery policies for supplier and manufacturer in a constrained closed-loop supply chain for returnable transport packaging through metaheuristic approach. Comput. Ind. Eng. 2019. [Google Scholar] [CrossRef]
- Taleizadeh, A.A.; Babaei, M.S.; Sana, S.S.; Sarkar, B. Pricing Decision within an Inventory Model for Complementary and Substitutable Products. Mathematics 2019, 7, 568. [Google Scholar] [CrossRef]
- Noh, J.; Kim, J.S.; Sarkar, B. Two-echelon supply chain coordination with advertising-driven demand under Stackelberg game policy. Eur. J. Ind. Eng. 2019, 13, 213–244. [Google Scholar] [CrossRef]
- Wook Kang, C.; Ullah, M.; Sarkar, M.; Omair, M.; Sarkar, B. A Single-Stage Manufacturing Model with Imperfect Items, Inspections, Rework, and Planned Backorders. Mathematics 2019, 7, 446. [Google Scholar] [CrossRef]
- Kim, S.J.; Sarkar, B. Supply chain model with stochastic lead time, trade-credit financing, and transportation discounts. Math. Prob. Eng. 2017, 2017, 6465912. [Google Scholar] [CrossRef]
- Sarkar, B.; Tayyab, M.; Choi, S.B. Product Channeling in an O2O Supply Chain Management as Power Transmission in Electric Power Distribution Systems. Mathematics 2019, 7, 4. [Google Scholar] [CrossRef]
- Sarkar, B.; Ullah, M.; Choi, S.B. Joint Inventory and Pricing Policy for an Online to Offline Closed-Loop Supply Chain Model with Random Defective Rate and Returnable Transport Items. Mathematics 2019, 7, 497. [Google Scholar] [CrossRef]
- Bhuniya, S.; Sarkar, B.; Pareek, S. Multi-Product Production System with the Reduced Failure Rate and the Optimum Energy Consumption under Variable Demand. Mathematics 2019, 7, 465. [Google Scholar] [CrossRef]
- Sarkar, B.; Guchhait, R.; Sarkar, M.; Cárdenas-Barrón, L.E. How does an industry manage the optimum cash flow within a smart production system with the carbon footprint and carbon emission under logistics framework? Int. J. Prod. Econ. 2019, 213, 243–257. [Google Scholar] [CrossRef]
- Heidari-Fathian, H.; Pasandideh, S.H.R. Green-blood supply chain network design: Robust optimization, bounded objective function & Lagrangian relaxation. Comput. Ind. Eng. 2018, 122, 95–105. [Google Scholar]


| Authors | SCM and the Optimum Energy (OE) | Blood Collection | Platelets | Location | Perishability |
|---|---|---|---|---|---|
| Nahmias [2] | SCM | NA | NA | NA | Applicable |
| Sha et al. [3] | SCM | NA | NA | NA | NA |
| Sarkar et al. [42] | SCM | NA | NA | NA | Applicable |
| Jabbarzadeh et al. [4] | SCM | Applicable | NA | NA | NA |
| Katsaliaki et al. [5] | SCM | Applicable | NA | NA | Applicable |
| Duan and Liao [6] | SCM | Applicable | NA | NA | NA |
| Bazan et al. [40] | SCM | NA | NA | NA | NA |
| Arvan et al. [7] | SCM | Applicable | NA | NA | NA |
| Hong et al. [25] | SCM | NA | NA | NA | NA |
| Habib and Sarkar [44] | SCM | NA | NA | Allocated | NA |
| Zahiri et al. [10] | SCM | Applicable | NA | Allocated | Applicable |
| Ramezanian et al. [11] | SCM | Applicable | NA | NA | NA |
| Paydar et al. [12] | SCM | Applicable | NA | NA | Applicable |
| Osorio et al. [9] | SCM | Applicable | NA | Allocated | Applicable |
| Najafi et al. [13] | SCM | Applicable | NA | NA | NA |
| Ensafian et al. [14] | SCM | Applicable | Applicable | NA | Applicable |
| Ahmed et al. [41] | SCM | NA | NA | Allocated | NA |
| Sarkar et al. [30] | SCM | NA | NA | NA | NA |
| Hosseinifard and Abbasi [15] | SCM | Applicable | NA | NA | NA |
| Singh et al. [29] | SCM | NA | NA | NA | NA |
| Samani et al. [16] | SCM | Applicable | NA | NA | NA |
| Eskandari et al. [17] | SCM | Applicable | Applicable | NA | NA |
| Hamdan and Diabat [18] | SCM | Applicable | NA | Allocated | NA |
| Mishra et al. [50] | SCM | NA | NA | NA | NA |
| Iqbal et al. [49] | SCM | NA | NA | NA | Applicable |
| Proposed model | SCM & OE | Applicable | Applicable | Allocated | Applicable |
| MBF | FBF | BC | Hospitals | Vehicles |
|---|---|---|---|---|
| 2 | 2 | 1 | 7 | 5 |
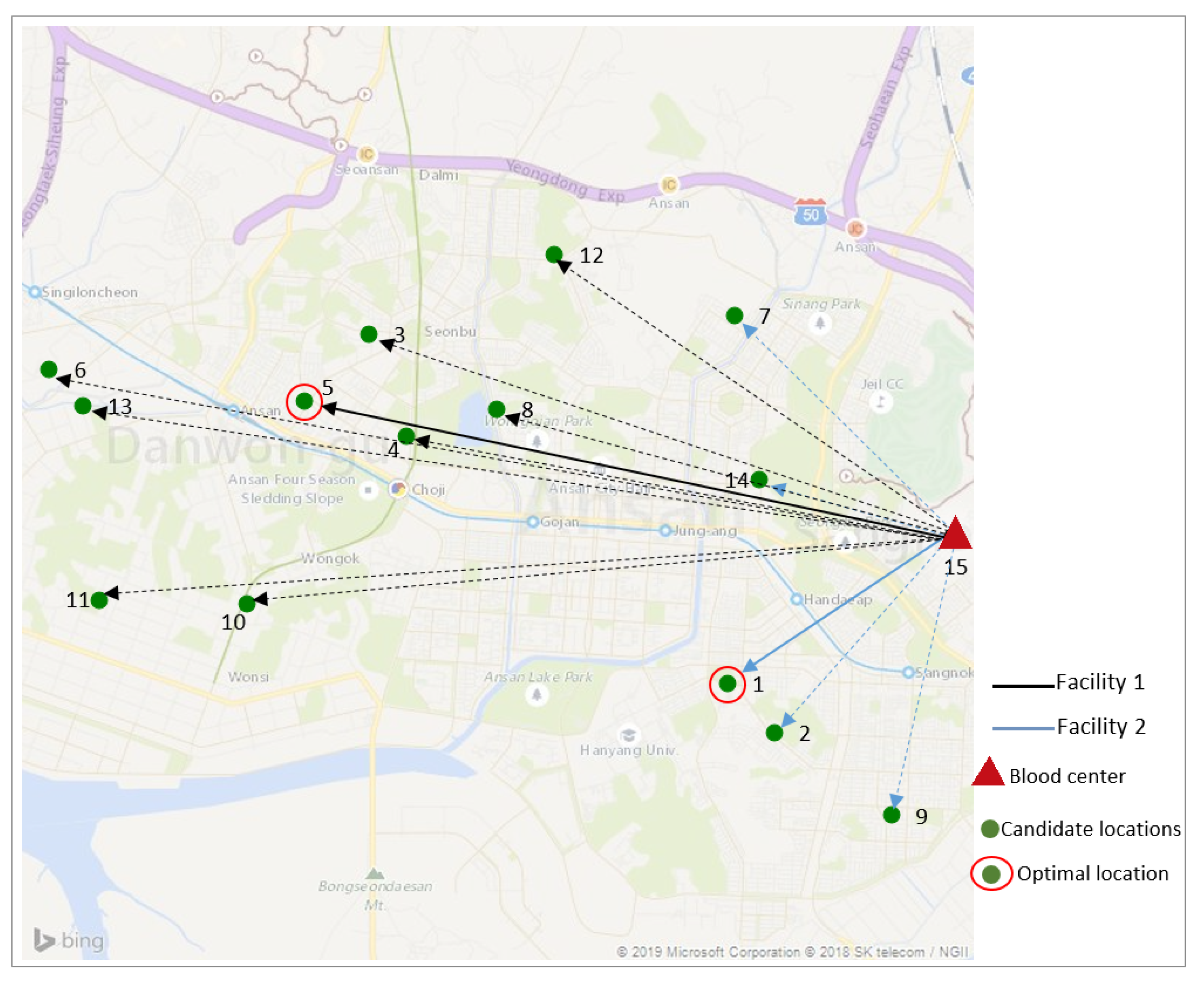
| Candidate Locations of the Blood Facilities (MBFs and FBFs). | |||||
|---|---|---|---|---|---|
| ID | Location | Address | Latitude (x) | Longitude (y) | Demand |
| 1 | L1 | Sangnok-gu, Ansan, South Korea | 37.30 | 126.84 | MBF/FBF |
| 2 | L2 | Sa-dong, Ansan, South Korea | 37.29 | 126.85 | MBF/FBF |
| 3 | L3 | Seonbu-dong, Ansan, South Korea | 37.33 | 126.80 | MBF/FBF |
| 4 | L4 | Choji-dong, Ansan, South Korea | 37.32 | 126.80 | MBF/FBF |
| 5 | L5 | Wongok-dong, Ansan, South Korea | 37.32 | 126.79 | MBF/FBF |
| 6 | L6 | Singil-dong, Ansan, South Korea | 37.33 | 126.76 | MBF/FBF |
| 7 | L7 | Wolpi-dong, Ansan, South Korea | 37.33 | 126.84 | MBF/FBF |
| 8 | L8 | Gojan-dong, Ansan, South Korea | 37.32 | 126.81 | MBF/FBF |
| 9 | L9 | Bono-dong, Ansan, South Korea | 37.28 | 126.86 | MBF/FBF |
| 10 | L10 | Wonsi-dong, Ansan, South Korea | 37.30 | 126.79 | FBF |
| 11 | L11 | Mongnae-dong, Ansan, South Korea | 37.30 | 126.77 | FBF |
| 12 | L12 | Wa-dong, Ansan, South Korea | 37.34 | 126.82 | FBF |
| 13 | L13 | Hosu-dong, Ansan, South Korea | 37.32 | 126.77 | FBF |
| 14 | L14 | Seongpo-dong, Ansan, South Korea | 37.32 | 126.84 | FBF |
| Location of the blood center in Ansan, South Korea. | |||||
| ID | Location | Address | Latitude (x) | Longitude (y) | |
| 15 | L15 | Ansan blood center, Ansan, South Korea | 37.31 | 126.87 | |
| Locations of the hospitals at Ansan, South Korea | |||||
| ID | Location | Address | Latitude (x) | Longitude (y) | |
| 1 | H1 | Danwon Hospital, Choji-dong, Ansan, South Korea | 37.32 | 126.80 | |
| 2 | H2 | Korea University Ansan Hospital, 69 516 Gojan-dong, Danwon-gu, Ansan-si, Gyeonggi-do, South Korea | 37.32 | 126.81 | |
| 3 | H3 | Duson Hospital, Seonbu-dong, Ansan-si, South Korea | 37.33 | 126.80 | |
| 4 | H4 | Sarang Hospital, 69 Yesulgwangjang-ro, Seongpo-dong, Sangnok-gu, Ansan-si, Gyeonggi-do, South Korea | 37.32 | 126.84 | |
| 5 | H5 | Hansarang Hospital, 345 Gwangdeok 1 (il)-ro, I-dong, Sangnok-gu, Ansan-si, Gyeonggi-do, South Korea | 37.30 | 126.84 | |
| 6 | H6 | Anshan 21st Century Hospital, 50 Bohwa-ro, Gojan 1 (il)-dong, Danwon-gu, Ansan-si, Gyeonggi-do, South Korea | 37.33 | 126.83 | |
| 7 | H7 | Ansan Hospital, Korea Labor Welfare Corporation, 95 Il-dong, Sangnok-gu, Ansan-si, Gyeonggi-do, South Korea | 37.30 | 126.86 | |
| Facilities | Candidate Locations | Optimal Location | Distance Between BC and FBF (km) |
|---|---|---|---|
| FBF1 | Location 1 | Location 1 | 5.5 |
| Location 2 | |||
| Location 7 | |||
| Location 9 | |||
| Location 14 | |||
| FBF2 | Location 5 | Location 5 | 9.3 |
| Location 3 | |||
| Location 4 | |||
| Location 6 | |||
| Location 8 | |||
| Location 10 | |||
| Location 11 | |||
| Location 12 | |||
| Location 13 |
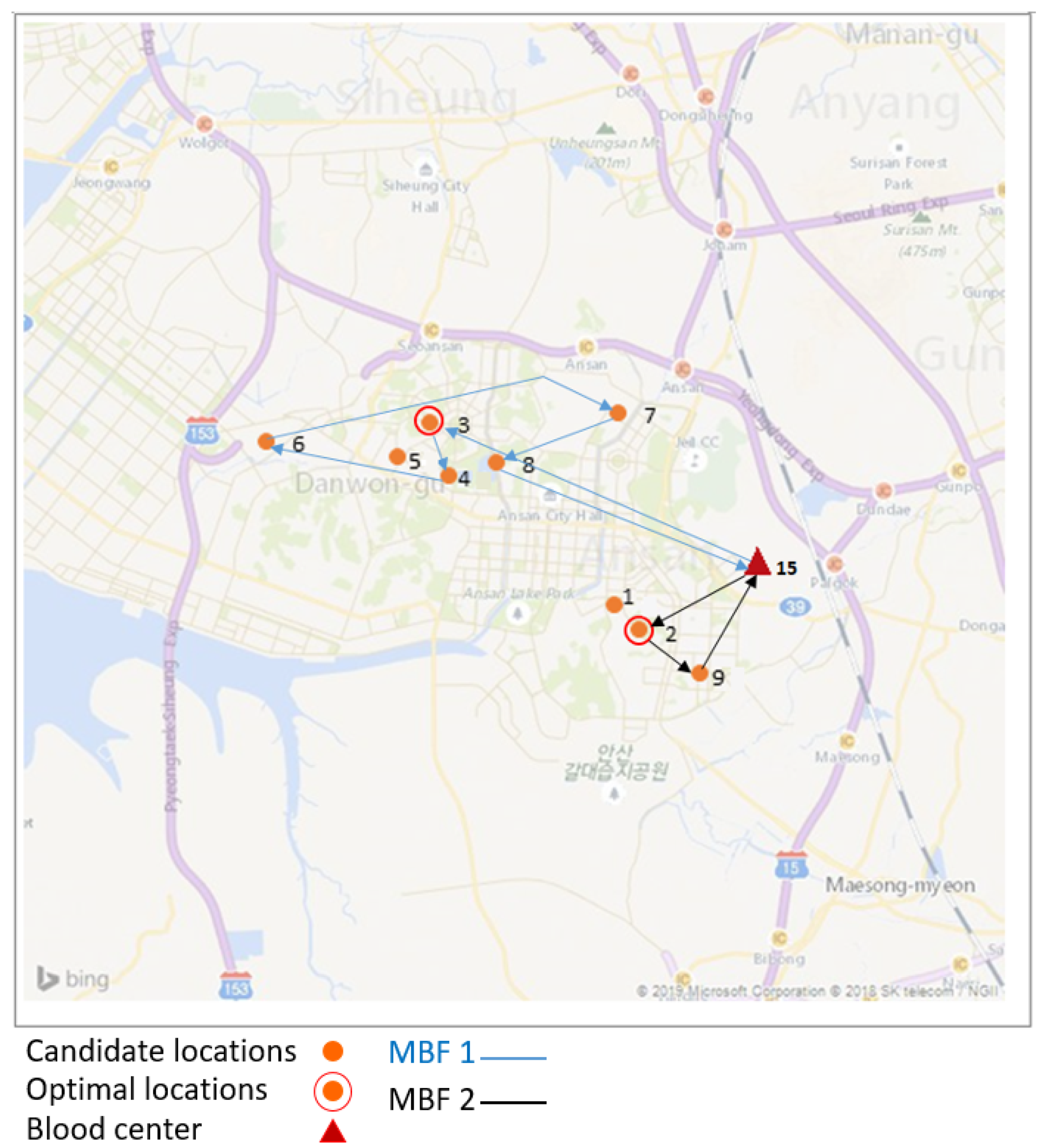
| MBF1 | Optimal Location | Address | Candidate Locations | Possible Visited Locations |
|---|---|---|---|---|
| 1 | Location 3 | Seonbu-dong, Ansan, South Korea | 9 | 6 |
| No. | Path | Distance (km) | Demand | Transportation Costs ($) |
| 1 | BC to Location 3 | 9.4 | 1 | 5.64 |
| 2 | Location 3 to Location 4 | 1.5 | 1 | 0.88 |
| 3 | Location 4 to Location 6 | 5 | 1 | 3 |
| 5 | Location 6 to Location 7 | 9.1 | 1 | 5.47 |
| 6 | Location 7 to Location 8 | 3.2 | 1 | 1.91 |
| 7 | Location 8 to BC | 7 | - | 4.2 |
| MBF2 | Optimal Location | Address | Candidate Locations | Possible Visited Locations |
|---|---|---|---|---|
| 1 | Location 2 | Sa-dong, Ansan, South Korea | 9 | 3 |
| No. | Path | Distance (km) | Demand | Transportation Costs ($) |
| 1 | BC to Location 2 | 5 | 1 | 3 |
| 2 | Location 2 to Location 9 | 2.4 | 1 | 1.44 |
| 4 | Location 9 to BC | 3.5 | - | 2.1 |
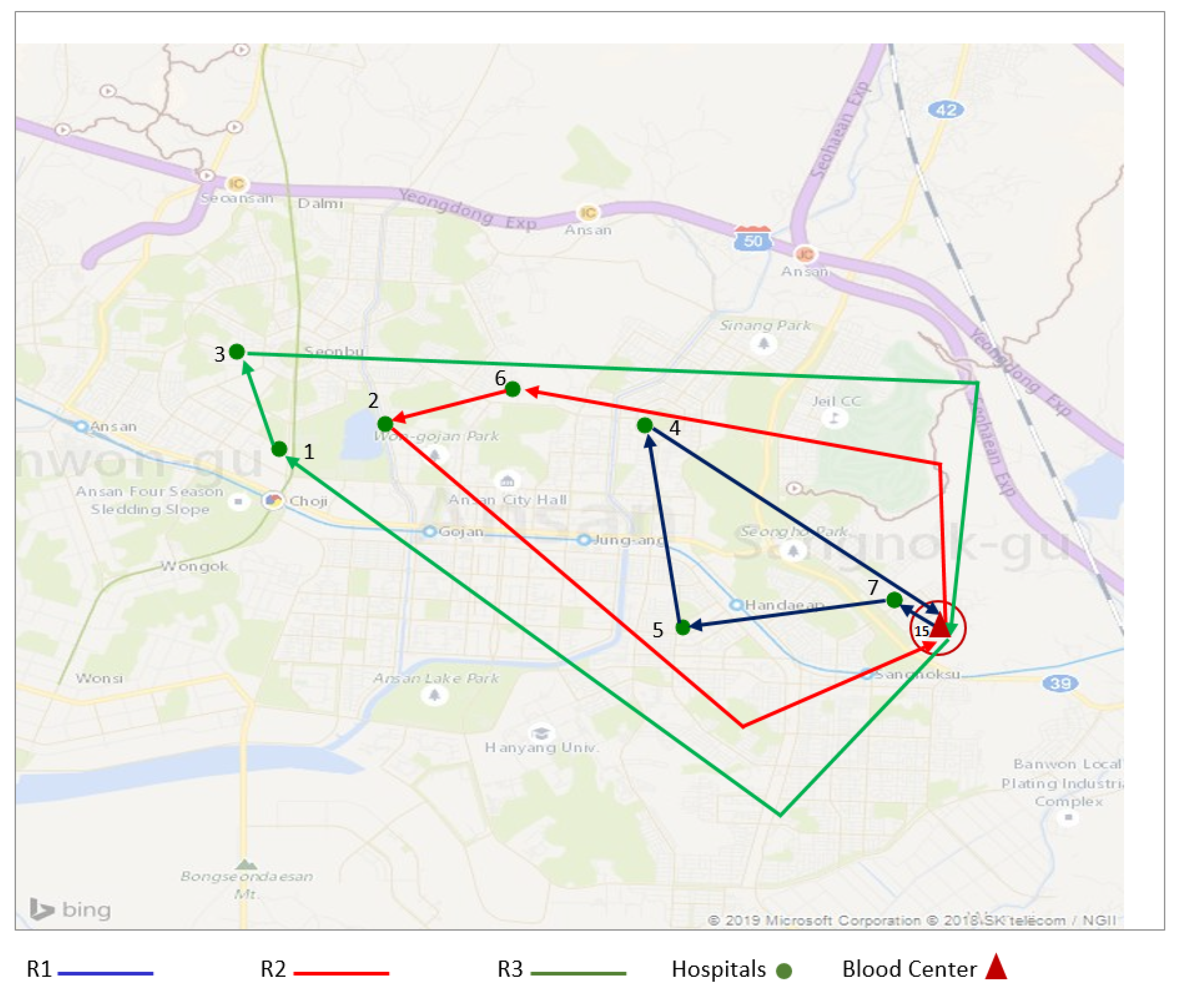
| Route | Path | Locations | Distance (km) | Total Distance (km) |
|---|---|---|---|---|
| R1 | BC to h1 h1 to h2 h2 to h3 h3 to BC | L15 to L7 L7 to L5 L5 to L4 L4 to L15 | 2.4 4 2.6 5.8 | 14.8 |
| R2 | BC to h1 h1 to h2 h2 to BC | L15 to L6 L6 to L2 L2 to L15 | 5.9 1.6 6.4 | 13.9 |
| R3 | BC to h1 h1 to h2 h2 to BC | L15 to L1 L1 to L3 L3 to L15 | 7.6 4.5 7.2 | 19.3 |
| Parameters | Values | Parameters | Values |
|---|---|---|---|
| [300, 400] | [1, 2] | ||
| [1000, 2000] | [20,000, 40,000] | ||
| [3000, 8000] | [15,000, 30,000] | ||
| [300, 400] | [10,000, 15,000] | ||
| Tc | [0.5, 0.7] | [60, 150] | |
| L | [5, 7] | d_{kj} | [1, 20] |
| d_{i_njt} | [1, 20] | ||
| d_{jh_it} | [1, 60] | ||
| d_{i_{n-1}i_n} | [0, 10] | ||
| [0.01, 0.05] | [0.1, 0.2] | ||
| [0.1, 0.2] | [0.5, 0.8] | ||
| Cu | [0.015, 0.018] | [1, 2] | |
| Uc | [0.01, 0.02] | [1, 210] | |
| [1, 2] | [1, 30] |
| Facilities | Scenario 1A | Scenario 2A | Scenario 3A | Scenario 4A | Scenario 5A |
|---|---|---|---|---|---|
| MBF1 | BC to L3 to BC | BC to L3 to L4 to BC | BC to L3 to L4 to L6 to BC | BC to L3 to L4 to L6 to L7 to BC | BC to L3 to L4 to L6 to L7 to L8 to BC |
| Scenario 1B | Scenario 2B | ||||
| MBF2 | BC to L2 to BC | BC to L2 to L9 to BC | |||
| FBF1 | Scenario 1C: BC to L1 to BC | ||||
| FBF2 | Scenario 1D: BC to L5 to BC | ||||
| Routes | R1: BC to L7’ to L5’ to L4’ to BC | R2: BC to L6’ to L2’ to BC | R2: BC to L1’ to L3’ to BC | ||
| TEST | |||||
| Scenarios | Runs | Path | Total costs ($/cycle) | ||
| Scenario 1 | Run 1 | Scenario 1A + Scenario 1B + Scenario 1C + Scenario 1D + R1 +R2 +R3 | 145245.37 | ||
| Scenario 2 | Run 2 | Scenario 2A + Scenario 1B + Scenario 1C + Scenario 1D + R1 +R2 +R3 | 144787.76 | ||
| Scenario 3 | Run 3 | Scenario 3A + Scenario 1B + Scenario 1C + Scenario 1D + R1 +R2 +R3 | 145746.94 | ||
| Scenario 4 | Run 4 | Scenario 4A + Scenario 1B + Scenario 1C + Scenario 1D + R1 +R2 +R3 | 146874.67 | ||
| Scenario 5 | Run 5 | Scenario 5A + Scenario 1B + Scenario 1C + Scenario 1D + R1 +R2 +R3 | 147379.21 | ||
| Scenario 6 | Run 6 | Scenario 1A + Scenario 2B + Scenario 1C + Scenario 1D + R1 +R2 +R3 | 145188.31 | ||
| Scenario 7 * | Run 7 * | Scenario 2A + Scenario 2B + Scenario 1C + Scenario 1D + R1 +R2 +R3 | 144687.69 * | ||
| Scenario 8 | Run 8 | Scenario 3A + Scenario 2B + Scenario 1C + Scenario 1D + R1 +R2 +R3 | 145471.87 | ||
| Scenario 9 | Run 9 | Scenario 4A + Scenario 2B + Scenario 1C + Scenario 1D + R1 +R2 +R3 | 146793.61 | ||
| Scenario 10 | Run 10 | Scenario 5A + Scenario 2B + Scenario 1C + Scenario 1D + R1 +R2 +R3 | 147196.15 | ||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jemai, J.; Sarkar, B. Optimum Design of a Transportation Scheme for Healthcare Supply Chain Management: The Effect of Energy Consumption. Energies 2019, 12, 2789. https://doi.org/10.3390/en12142789
Jemai J, Sarkar B. Optimum Design of a Transportation Scheme for Healthcare Supply Chain Management: The Effect of Energy Consumption. Energies. 2019; 12(14):2789. https://doi.org/10.3390/en12142789
Chicago/Turabian StyleJemai, Jihed, and Biswajit Sarkar. 2019. "Optimum Design of a Transportation Scheme for Healthcare Supply Chain Management: The Effect of Energy Consumption" Energies 12, no. 14: 2789. https://doi.org/10.3390/en12142789






