Maintaining Traditions: A Qualitative Study of Early Childhood Caries Risk and Protective Factors in an Indigenous Community
Abstract
:1. Introduction
2. Materials and Methods
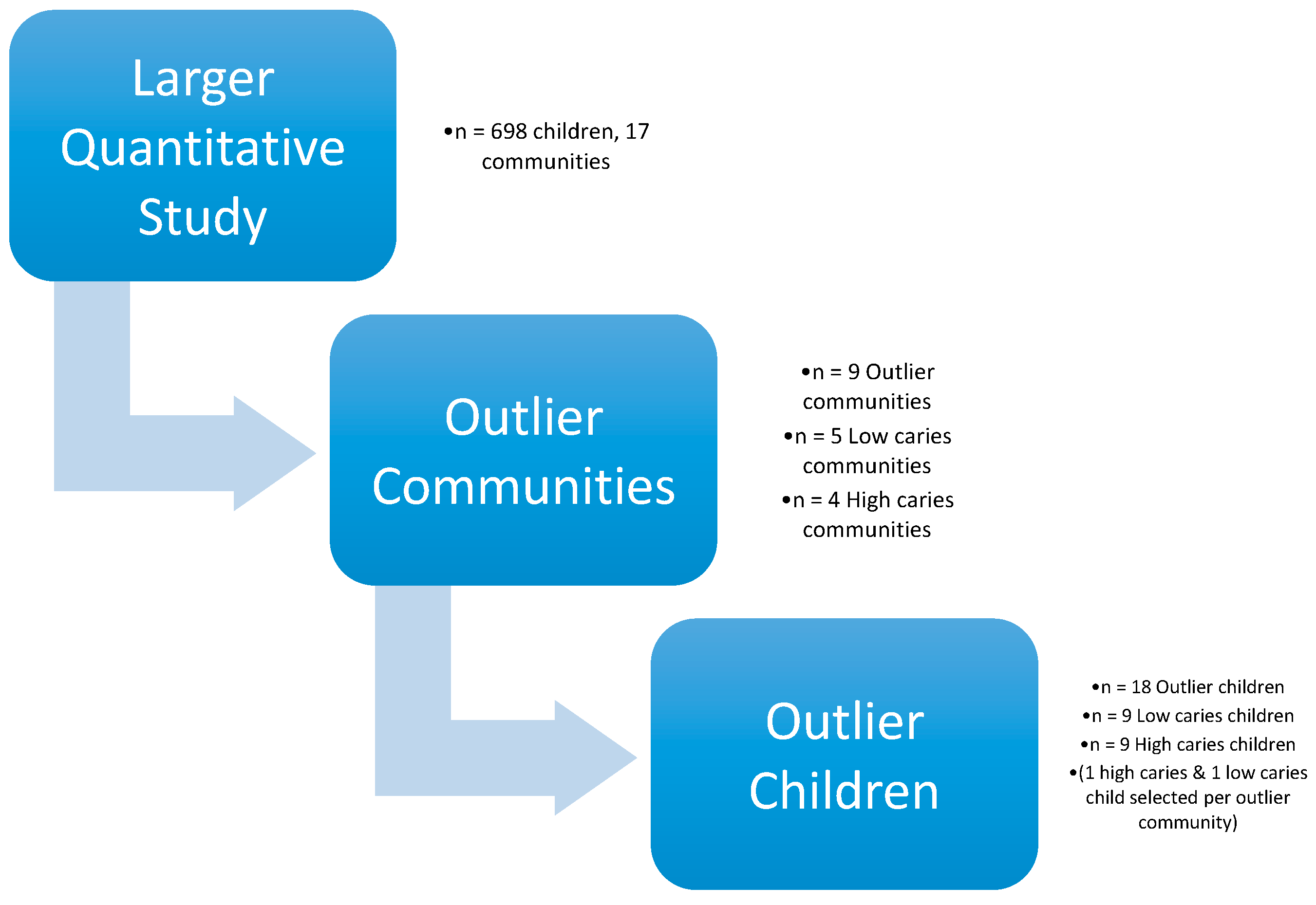
2.1. Study Design
2.2. Study Population
2.3. Data Collection
2.4. Data Analysis
3. Results
3.1. Demographics and Dental Status
3.2. Nutrition
3.2.1. Nutrition Risk Factors
The first time he tried cola he must have been really small still, because sometimes we would take the little ones into town with us. But we wouldn’t bring enough chicha to last through the day and they’d get thirsty. So we would have to buy them cola and we’d put it in his bottle. I’m not sure how old he was—Maybe six months?—High-caries parent
I remember when I was a girl, we would eat together as a family. But today, we can’t. I leave early for work and my husband too. My babies leave early for school. Maybe on the weekends we’ll all sit down, but during the work week, we almost never see each other. It’s a total change. On the other hand, for the families that live in the [interior] communities, they don’t have three meals a day... maybe only once a day. But they eat the food from out there [their farms]. Those of us who live closer [to the city], we eat what there is. We rush around and for one reason or another we don’t eat. Since children don’t eat at home, they eat other things outside of the house. So, health is really suffering.—High-caries parent
Maybe because I’m not there, or I’m not paying attention—sometimes due to my work—I try to make it better by giving them treats. I’m not there in the house to be with them and care for them.—High-caries parent
3.2.2. Nutrition Protective Factors
I’m mostly committed to my chacra. Plantain, if I want to buy it in Archidona [the nearby city], it’s so expensive. I can barely buy three or four. I prefer to go to the farm, work, bring back a few plantains, a few bananas, papayas….that way it’s way cheaper. That’s why I’m more committed to the chacra. You know, instead of buying [at the store], I harvest at the chacra. So, with that it’s enough, I mean, I can make a soup with all that.—Low-caries parent
I decide what they eat because I know what things are good for them. So sometimes, well I have to lie a bit. I’ve said to my kids “If you don’t eat your food I won’t give you money to buy sweets.” Well, then they eat it all up! Later when they ask me about the money for their sweets I tell them that of course we don’t have money to spend on sweets. I say to them, “But there are apples and mandarins in the fridge. Grab one and leave me alone!”—Low-caries parent
My parents were not educated about these things. So then they also weren’t able to educate us, we would always eat candy, chocolates, popsicles, soda. We had no idea what could damage our teeth. And they didn’t know to tell us that we should brush our teeth. If we wanted to brush, great; if not, that was fine too. So, that’s why my generation, we have such damaged teeth and so many caries, and even mouth pain. It’s taught me, and that’s why now I say “no” to my own kids [about candy]. When my kids have tooth pain, they are so miserable. Sometimes they won’t be able to sleep all night [because of the pain]. So I say “you kids aren’t going to eat candy.” There are rare times that I’ll bring them home sweets. Not every time I go into town like so many of the other moms.—Low-caries parent
3.3. Health
3.3.1. Health Risk Factors
Sometimes my girls don’t want to brush and I have to make them. They say “No, no, I didn’t eat anything bad. I don’t want to brush.”—Low-caries parent
The medical attention we get is from the Ministry of Health, and the government says that the care there is equal for everyone, but it’s eye opening. The public [health] employees, supposedly responsible for caring for the public, aren’t supposed to give anyone priority. However, Kichwa people are always given poorer care. In contrast, mestizo people, for them, they attend to them more quickly.—Low-caries parent
3.3.2. Health Protective Factors
So then I say “You have to brush. The bugs [bacteria] are gonna come after you. And my kids will say, “Where are they? Bring me a mirror so I can see if the bugs are there.” So I tell them, “Brush first and then you’ll see. If you don’t, the bugs are gonna go to school to learn with you.” My kids say “Okay fine! I’ll brush so the bugs don’t come after me.”—Low-caries parent
If you have bad teeth it can get to the point where you’re embarrassed to even talk because of the bad state of your teeth and because of bad breath, you know? Having good teeth gives one a good self-image as well.—Low-caries parent
4. Discussion
4.1. Implications for Policy and Practice
4.2. Strengths and Limitations
5. Conclusions
Supplementary Materials
Supplementary File 1Acknowledgments
Author Contributions
Conflicts of Interest
References
- Popkin, B.M. Relationship between shifts in food system dynamics and acceleration of the global nutrition transition. Nutr. Rev. 2017, 75, 73–82. [Google Scholar] [CrossRef] [PubMed]
- Bagramian, R.A.; Garcia-Godoy, F.; Volpe, A.R. The global increase in dental caries. A pending public health crisis. Am. J. Dent. 2009, 22, 3–8. [Google Scholar] [PubMed]
- Sheiham, A. Dental caries affects body weight, growth and quality of life in pre-school children. Br. Dent. J. 2006, 201, 625–626. [Google Scholar] [CrossRef] [PubMed]
- Casamassimo, P.S.; Thikkurissy, S.; Edelstein, B.L.; Maiorini, E. Beyond the DMFT: The human and economic cost of early childhood caries. J. Am. Dent. Assoc. 2009, 140, 650–657. [Google Scholar] [CrossRef] [PubMed]
- Featherstone, J. The continuum of dental caries—Evidence for a dynamic disease process. J. Dent. Res. 2004, 83, C39–C42. [Google Scholar] [CrossRef] [PubMed]
- Mattos-Graner, R.O.; Klein, M.I.; Smith, D.J. Lessons learned from clinical studies: Roles of mutans streptococci in the pathogenesis of dental caries. Curr. Oral Health Rep. 2014, 1, 70–78. [Google Scholar] [CrossRef]
- Silk, H. Diseases of the mouth. Prim. Care Clin. Off. Pract. 2014, 41, 75–90. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Pediatric Dentistry. Policy on Early Childhood Caries (ecc): Unique Challenges and Treatment Options; American Academy of Pediatric Dentistry: Chicago, IL, USA, 2007. [Google Scholar]
- Fisher-Owens, S.A.; Gansky, S.A.; Platt, L.J.; Weintraub, J.A.; Soobader, M.-J.; Bramlett, M.D.; Newacheck, P.W. Influences on children’s oral health: A conceptual model. Pediatrics 2007, 120, e510–e520. [Google Scholar] [CrossRef] [PubMed]
- Schulz, A.; Northridge, M.E. Social determinants of health: Implications for environmental health promotion. Health Educ. Behav. 2004, 31, 455–471. [Google Scholar] [CrossRef] [PubMed]
- Patrick, D.L.; Lee, R.S.Y.; Nucci, M.; Grembowski, D.; Jolles, C.Z.; Milgrom, P. Reducing oral health disparities: A focus on social and cultural determinants. BMC Oral Health 2006, 6. [Google Scholar] [CrossRef] [PubMed]
- Northridge, M.E.; Schrimshaw, E.W.; Estrada, I.; Greenblatt, A.P.; Metcalf, S.S.; Kunzel, C. Intergenerational and social interventions to improve children’s oral health. Dent. Clin. N. Am. 2017, 61, 533–548. [Google Scholar] [CrossRef] [PubMed]
- Weintraub, J.A.; Ramos-Gomez, F.; Jue, B.; Shain, S.; Hoover, C.I.; Featherstone, J.D.; Gansky, S.A. Fluoride varnish efficacy in preventing early childhood caries. J. Dent. Res. 2006, 85, 172–176. [Google Scholar] [CrossRef] [PubMed]
- Petersen, P.E. World health organization global policy for improvement of oral health-world health assembly 2007. Int. Dent. J. 2008, 58, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Colchero, M.A.; Popkin, B.M.; Rivera, J.A.; Ng, S.W. Beverage purchases from stores in Mexico under the excise tax on sugar sweetened beverages: Observational study. BMJ 2016, 352, h6704. [Google Scholar] [CrossRef] [PubMed]
- Falbe, J.; Thompson, H.R.; Becker, C.M.; Rojas, N.; McCulloch, C.E.; Madsen, K.A. Impact of the berkeley excise tax on sugar-sweetened beverage consumption. J. Inf. 2016, 106, 1865–1871. [Google Scholar] [CrossRef] [PubMed]
- Irvine, J.; Holve, S.; Krol, D.; Schroth, R. Early childhood caries in indigenous communities: A joint statement with the american academy of pediatrics. Paediatr. Child Health 2011, 16, 351–357. [Google Scholar] [PubMed]
- Normando, A.D.C.; Araújo, I.C.D. Prevalence of dental caries in a school population of the Amazonian region. Rev. Saúde Pública 1990, 24, 294–299. [Google Scholar] [CrossRef] [PubMed]
- Medina, W.; Hurtig, A.-K.; San Sebastián, M.; Quizhpe, E.; Romero, C. Dental caries in 6–12-year-old indigenous and non-indigenous schoolchildren in the Amazon basin of Ecuador. Braz. Dent. J. 2008, 19, 83–86. [Google Scholar] [CrossRef] [PubMed]
- Lanfranco, L.P.; Eggers, S. Caries through Time: An Anthropological Overview; INTECH Open Access Publisher: Rijeka, Croatia, 2012. [Google Scholar]
- Niswander, J.D. Further studies on the xavante indians. VII. The oral status of the xavantes of simões lopes. Am. J. Hum. Genet. 1967, 19, 543. [Google Scholar] [PubMed]
- Rigonatto, D.D.L.; Antunes, J.L.F.; Frazao, P. Dental caries experience in indians of the upper Xingu, Brazil. Rev. Inst. Med. Trop. S. Paulo 2001, 43, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Sokal-Gutierrez, K.; Turton, B.; Husby, H.; Paz, C.L. Early childhood caries and malnutrition: Baseline and two-year follow-up results of a community-based prevention intervention in rural Ecuador. BMC Nutr. 2016, 2, 73. [Google Scholar] [CrossRef]
- Wishik, S.M.; Vynckt, S. The use of nutritional ‘positive deviants’ to identify approaches for modification of dietary practices. Am. J. Public Health 1976, 66, 38–42. [Google Scholar] [CrossRef] [PubMed]
- Charmaz, K.; Belgrave, L. Qualitative interviewing and grounded theory analysis. In The SAGE Handbook of Interview Research: The Complexity of the Craft; SAGE: Thousand Oaks, CA, USA, 2002; Volume 2. [Google Scholar]
- Dedoose, V. Web Application for Managing, Analyzing, and Presenting Qualitative and Mixed Method Research Data, Version D. 5.0. 11; SocioCultural Research Consultants, LLC: Los Angeles, CA, USA, 2014. [Google Scholar]
- McDade, T.W. Lifestyle incongruity, social integration, and immune function in samoan adolescents. Soc. Sci. Med. 2001, 53, 1351–1362. [Google Scholar] [CrossRef]
- Masood, M.; Masood, Y.; Newton, T. Impact of national income and inequality on sugar and caries relationship. Caries Res. 2012, 46, 581–588. [Google Scholar] [CrossRef] [PubMed]
- Schwendicke, F.; Dörfer, C.; Schlattmann, P.; Page, L.F.; Thomson, W.; Paris, S. Socioeconomic inequality and caries a systematic review and meta-analysis. J. Dent. Res. 2015, 94, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Zeng, X.; Sheiham, A.; Sabbah, W. The association between dental caries and television viewing among chinese adolescents in Guangxi, China. BMC Oral Health 2014, 14, 138. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | High Caries | Low Caries | All |
|---|---|---|---|
| n = 9 | n = 9 | n = 18 | |
| Mean (SD) or % | Mean (SD) or % | Mean (SD) or % | |
| Child Characteristics | |||
| Mean age | 4.6 (1.3) | 3.7 (1.5) | 4.1 (1.5) |
| Male, Female % | 67%, 33% | 44%, 56% | 56%, 44% |
| Mean # Decayed Teeth (range) | 11.4 (1.4) Range = 10–14 | 1.64 (1) Range = 0–2 | 6.4 (5.1) |
| Mean # Child Dental Visits | 3 | 6.8 | 10 |
| Mother and Household Characteristics | |||
| Mean Maternal Age | 34 (8.5) | 28 (3.9) | 31 (6.8) |
| Mean # Children | 3.8 | 3.4 | 5.5 |
| Mean # Years of Education | 11.6 | 8.6 | 10 |
| % Potable water in home | 43% | 50% | 47% |
| % Electricity in home | 86% | 88% | 87% |
| % Cook with gas | 100% | 88% | 94% |
| Living in community located proximal to highway | 12% | 11% | 12% |
| Living within 5-min walk to store | 86% | 75% | 80% |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Levin, A.; Sokal-Gutierrez, K.; Hargrave, A.; Funsch, E.; Hoeft, K.S. Maintaining Traditions: A Qualitative Study of Early Childhood Caries Risk and Protective Factors in an Indigenous Community. Int. J. Environ. Res. Public Health 2017, 14, 907. https://doi.org/10.3390/ijerph14080907
Levin A, Sokal-Gutierrez K, Hargrave A, Funsch E, Hoeft KS. Maintaining Traditions: A Qualitative Study of Early Childhood Caries Risk and Protective Factors in an Indigenous Community. International Journal of Environmental Research and Public Health. 2017; 14(8):907. https://doi.org/10.3390/ijerph14080907
Chicago/Turabian StyleLevin, Ana, Karen Sokal-Gutierrez, Anita Hargrave, Elizabeth Funsch, and Kristin S. Hoeft. 2017. "Maintaining Traditions: A Qualitative Study of Early Childhood Caries Risk and Protective Factors in an Indigenous Community" International Journal of Environmental Research and Public Health 14, no. 8: 907. https://doi.org/10.3390/ijerph14080907




