Prevalence and Associated Factors of Secondhand Smoke Exposure among Internal Chinese Migrant Women of Reproductive Age: Evidence from China’s Labor-Force Dynamic Survey
Abstract
:1. Introduction
2. Methods
2.1. Data and Sampling
2.2. Variable Definitions
2.2.1. Secondhand Smoke
2.2.2. Migration Experience
2.2.3. Demographic Variates
2.2.4. Other Covariates
2.3. Statistical Analysis
3. Results
3.1. Demographics of the Study Population
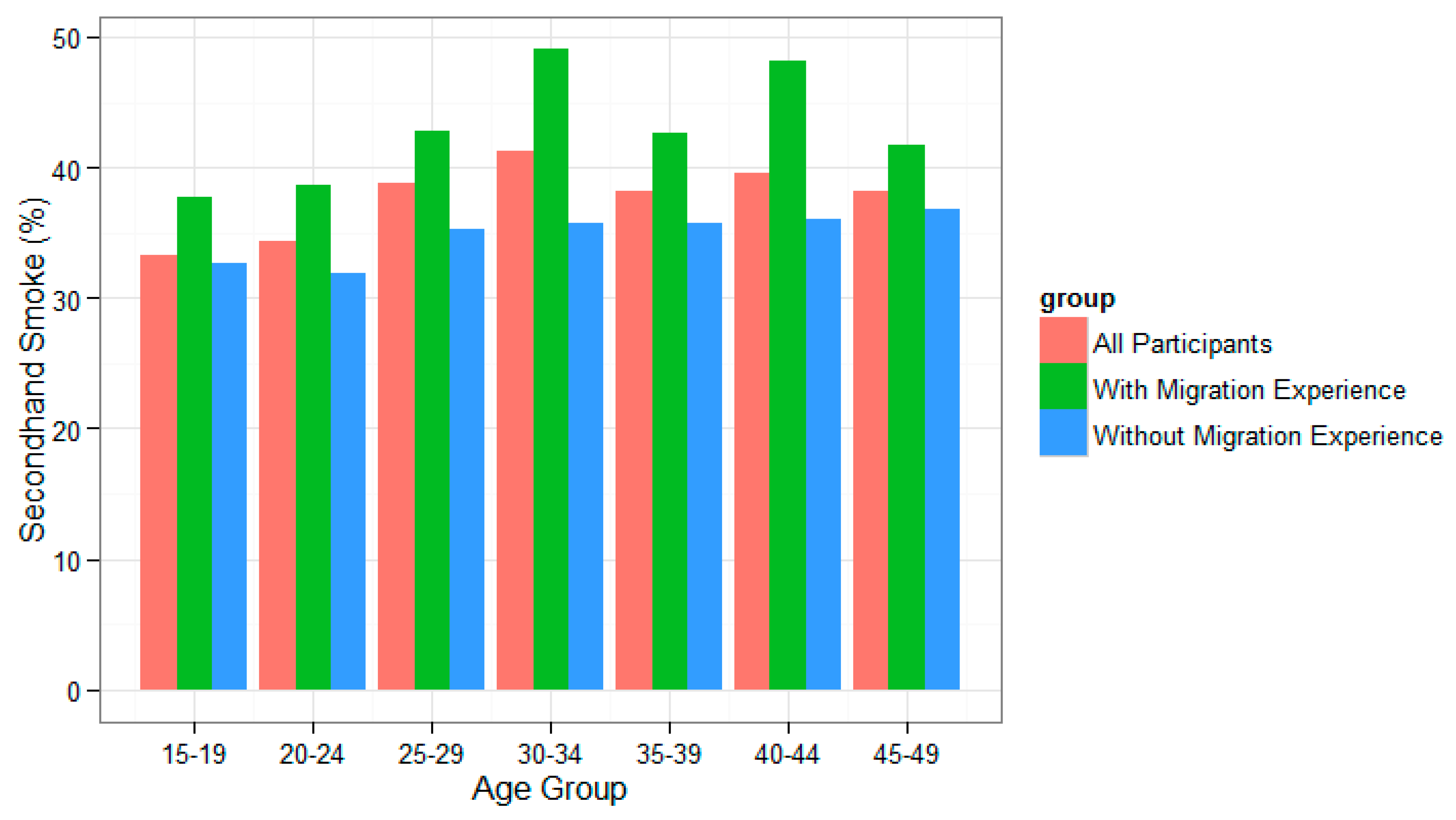
3.2. SHS Exposure Status by Migration Experience
3.3. Associated Factors of SHS Exposure: Results of Univariate and Multivariate Logistic Regressions
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- World Health Organization (WHO). WHO Report on the Global Tobacco Epidemic, 2011: Warning about the Dangers of Tobacco; WHO: Geneva, Switzerland, 2011. [Google Scholar]
- Mathers, C.D.; Loncar, D. Projections of global mortality and burden of disease from 2002 to 2030. PLOS Med. 2006, 3, e442. [Google Scholar]
- Office on Smoking and Health (US). The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General; Centers for Disease Control and Prevention (US): Atlanta, GA, USA, 2006. [Google Scholar]
- Menezes, A.M.; Hallal, P.C. Role of passive smoking on COPD risk in non-smokers. Lancet 2007, 370, 716–717. [Google Scholar] [PubMed]
- Zheng, P.; Li, W.; Chapman, S.; Zhang, Z.; Gao, J.; Fu, H. Workplace exposure to secondhand smoke and its association with respiratory symptoms—A cross-sectional study among workers in Shanghai. Tob. Control 2011, 20, 58–63. [Google Scholar] [CrossRef] [PubMed]
- Meeker, J.D.; Benedict, M.D. Infertility, Pregnancy Loss and Adverse Birth Outcomes in Relation to Maternal Secondhand Tobacco Smoke Exposure. Curr. Womens Health Rev. 2013, 9, 41–49. [Google Scholar] [CrossRef] [PubMed]
- Hyland, A.; Piazza, K.M.; Hovey, K.M.; Ockene, J.K.; Andrews, C.A.; Rivard, C.; Wactawski-Wende, J. Associations of lifetime active and passive smoking with spontaneous abortion, stillbirth and tubal ectopic pregnancy: A cross-sectional analysis of historical data from the Women’s Health Initiative. Tob. Control 2014, 2. [Google Scholar] [CrossRef] [PubMed]
- Rubin, D.H.; Krasilnikoff, P.A.; Leventhal, J.M.; Weile, B.; Berget, A. Effect of passive smoking on birth-weight. Lancet 1986, 2, 415–417. [Google Scholar] [CrossRef]
- Qiu, J.; He, X.; Cui, H.; Zhang, C.; Zhang, H.; Dang, Y.; Han, X.; Chen, Y.; Tang, Z.; Zhang, H.; et al. Passive smoking and preterm birth in urban China. Am. J. Epidemiol. 2014, 180, 94–102. [Google Scholar]
- Jaddoe, V.W.; Troe, E.J.; Hofman, A.; Mackenbach, J.P.; Moll, H.A.; Steegers, E.A.; Witteman, J.C. Active and passive maternal smoking during pregnancy and the risks of low birthweight and preterm birth: The Generation R Study. Paediatr. Perinat. Epidemiol. 2008, 22, 162–171. [Google Scholar] [PubMed]
- Fantuzzi, G.; Aggazzotti, G.; Righi, E.; Facchinetti, F.; Bertucci, E.; Kanitz, S.; Barbone, F.; Sansebastiano, G.; Battaglia, M.A.; Leoni, V.; et al. Preterm delivery and exposure to active and passive smoking during pregnancy: A case-control study from Italy. Paediatr. Perinat. Epidemiol. 2007, 21, 194–200. [Google Scholar] [PubMed]
- Anderson, H.R.; Cook, D.G. Passive smoking and sudden infant death syndrome: Review of the epidemiological evidence. Thorax 1997, 52, 1003–1009. [Google Scholar] [CrossRef] [PubMed]
- Strachan, D.P.; Cook, D.G. Health effects of passive smoking 1: Parental smoking and lower respiratory illness in infancy and early childhood. Thorax 1997, 52, 905–914. [Google Scholar] [CrossRef]
- Cook, D.G.; Strachan, D.P. Health effects of passive smoking. 3. Parental smoking and prevalence of respiratory symptoms and asthma in school age children. Thorax 1997, 52, 1081–1094. [Google Scholar] [PubMed]
- Yang, G.H.; Ma, J.M.; Liu, N.A.; Zhou, L.N. Smoking and passive smoking in Chinese, 2002. Chin. J. Epidemiol. 2005, 26, 77–83. [Google Scholar]
- Chen, M.H. Economic concerns hamper tobacco control in China. Lancet 2007, 370, 729–730. [Google Scholar] [CrossRef]
- Li, Q.; Hsia, J.; Yang, G. Prevalence of Smoking in China in 2010. New Engl. J. Med. 2011, 364, 2469–2470. [Google Scholar] [CrossRef] [PubMed]
- Gan, Q.; Smith, K.R.; Hammond, S.K.; Hu, T. Disease burden of adult lung cancer and ischaemic heart disease from passive tobacco smoking in China. Tob. Control 2007, 16, 417–422. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Xiao, L.; Zhao, L.; Morton, J.; Wang, C.; Feng, G.; Wu, Y.; Jiang, Y.; Yang, J.; Gan, Q.; et al. Global Adult Tobacco Survey (GATS) China 2010 Country Report. Available online: http://www.notc.org.cn/newjcpg/201304/W020121108628365808856.pdf (accessed on 6 August 2010).
- Zhang, L.; Hsia, J.; Tu, X.; Xia, Y.; Zhang, L.; Bi, Z.; Liu, H.; Li, X.; Stanton, B. Exposure to secondhand tobacco smoke and interventions among pregnant women in China: A systematic review. Prev. Chronic Dis. 2015, 12, E35. [Google Scholar] [CrossRef] [PubMed]
- National Health and Family Planning Commission of China. Report on China’s Migrant Population Development (2015); China Population Publishing House: Beijing, China, 2015. [Google Scholar]
- Mou, J.; Fellmeth, G.; Griffiths, S.; Dawes, M.; Cheng, J. Tobacco smoking among migrant factory workers in Shenzhen, China. Nicotine Tob. Res. 2013, 15, 69–76. [Google Scholar] [CrossRef]
- Chen, X.; Li, X.; Stanton, B.; Fang, X.; Lin, D.; Cole, M.; Liu, H.; Yang, H. Cigarette smoking among rural-to-urban migrants in Beijing, China. Prev. Med. 2004, 39, 666–673. [Google Scholar] [PubMed]
- Yu, Z.; Qiao, L.; Wang, X.; Yang, X.; Zhang, L.; Hu, W.; Wu, Y.; Kong, L.; Du, S.; Ma, G. Investigation on health-threatening behaviors among the immigrants living in an urban district of Beijing. Chin. J. Prev. Control Chronic Non-Commun. Dis. 2010, 18, 448–451. [Google Scholar]
- Zhu, Z.; Zhang, M.; Zhong, S. Investigation of Health Related Factors of Migrant Workers Gathering Areas. Chin. Gen. Pract. 2013, 16, 2140–2142. [Google Scholar]
- Cui, X.; Rockett, I.R.; Yang, T.; Cao, R. Work stress, life stress, and smoking among rural–urban migrant workers in China. BMC Public Health 2012, 12, 979. [Google Scholar] [CrossRef] [PubMed]
- Gong, P.; Liang, S.; Carlton, E.J.; Jiang, Q.; Wu, J.; Wang, L.; Remais, J.V. Urbanisation and health in China. Lancet 2012, 379, 843–852. [Google Scholar] [CrossRef]
- Zhang, J.; Zhu, Y.; Fu, Y.; Ding, D.; Hou, Z.; Liu, J. Investigation on the current situation of passive smoking among the floating population in Jilin province. Chin. J. Public Health Eng. 2015, 160–161. [Google Scholar]
- Huang, Z.; Wang, L.; Zhang, M.; Deng, Q.; Wang, Z.; Zhao, Y.; Li, Y.; Zhao, Z. Smoking behavior among the Chinese employed floating population aged 18–59 in 2012. Chin. J. Epidemiol. 2014, 35, 1192–1197. [Google Scholar]
- Department of Sociology at Sun Yat-sen University China Labor Force Dynamics Survey. Available online: http://css.sysu.edu.cn/Data (accessed on 24 January 2016).
- World Health Organization (WHO). Trends in Maternal Mortality: 1990 to 2013: Estimates by WHO, UNICEF, UNFPA, the World Bank and the United Nations Population Division; WHO: Geneva, Switzerland, 2014. [Google Scholar]
- Ledwith, F. Guidelines for the Conduct of Tobacco Smoking Surveys of the General Population; WHO: Geneva, Switzerland, 1983. [Google Scholar]
- Fay, M.P.; Feuer, E.J. Confidence intervals for directly standardized rates: A method based on the gamma distribution. Stat. Med. 1997, 16, 791–801. [Google Scholar] [PubMed]
- Selvin, S. Statistical Analysis of Epidemiologic Data; Oxford University Press: Oxford, UK, 2004; pp. 382–383. [Google Scholar]
- Li, Z.; Yao, Y.; Yu, Y.; Shi, J.; Liu, Y.; Tao, Y.; Kou, C.; Zhang, H.; Han, W.; Yin, Y.; et al. Prevalence and Associated Factors of Passive Smoking among Women in Jilin Province, China: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2015, 12, 13970–13980. [Google Scholar]
- Yang, T.; Wu, J.; Rockett, I.; Abdullah, A.S.; Beard, J.; Ye, J. Smoking patterns among Chinese rural–urban migrant workers. Public Health 2009, 123, 743–749. [Google Scholar] [CrossRef]
- Joseph, L. Epidemic Models of the Onset of Social Activities. In Handbook of Developmental Research Methods; Guilford Press: New York, NY, USA, 2012; pp. 706–724. [Google Scholar]
- Ennett, S.T.; Foshee, V.A.; Bauman, K.E.; Hussong, A.; Faris, R.; Hipp, J.R.; Cai, L. A social contextual analysis of youth cigarette smoking development. Nicotine Tob. Res. 2010, 12, 950–962. [Google Scholar]
- Glad, W.; Adesso, V.J. The relative importance of socially induced tension and behavioral contagion for smoking behavior. J. Abnorm. Psychol. 1976, 85, 119. [Google Scholar]
- Desalu, O.O.; Onyedum, C.C.; Adewole, O.O.; Fawibe, A.E.; Salami, A.K. Secondhand smoke exposure among nonsmoking adults in two Nigerian cities. Ann. Afr. Med. 2011, 10, 103–111. [Google Scholar]
- King, B.A.; Mirza, S.A.; Babb, S.D.; GATS Collaborating Group. A cross-country comparison of secondhand smoke exposure among adults: Findings from the Global Adult Tobacco Survey (GATS). Tob. Control 2013, 22, e5. [Google Scholar]
- Protano, C.; Andreoli, R.; Manini, P.; Vitali, M. How home-smoking habits affect children: A cross-sectional study using urinary cotinine measurement in Italy. Int. J. Public Health 2012, 57, 885–892. [Google Scholar]
- Matt, G.E.; Quintana, P.J.; Destaillats, H.; Gundel, L.A.; Sleiman, M.; Singer, B.C.; Jacob, P.; Benowitz, N.; Winickoff, J.P.; Rehan, V.; et al. Thirdhand tobacco smoke: Emerging evidence and arguments for a multidisciplinary research agenda. Environ. Health Perspect. 2011, 119, 1218–1226. [Google Scholar] [PubMed]
- Protano, C.; Vitali, M. The new danger of thirdhand smoke: Why passive smoking does not stop at secondhand smoke. Environ. Health Perspect. 2011, 119, A422. [Google Scholar] [PubMed]
| Variables | Number | Participants With Migration Experience | Participants Without Migration Experience | ||
|---|---|---|---|---|---|
| SHS (N, %) | Non-SHS (N, %) | SHS (N, %) | Non-SHS (N, %) | ||
| Sample Size | 7617 | 1094 | 1398 | 1806 | 3319 |
| Age Group | |||||
| 15–19 | 732 (9.6) | 29 (2.7) | 48 (3.4) | 214 (11.8) | 441 (13.3) |
| 20–29 | 1754 (23.0) | 308 (28.2) | 438 (31.3) | 340 (18.8) | 668 (20.1) |
| 30–39 | 1998 (26.2) | 355 (32.4) | 418 (29.9) | 437 (24.2) | 788 (23.7) |
| 40–49 | 3133 (41.1) | 402 (36.7) | 494 (35.3) | 815 (45.1) | 1422 (42.8) |
| Marital Status | |||||
| Single | 1425 (18.7) | 99 (9.0) | 185 (13.2) | 362 (20.1) | 779 (23.5) |
| Married: First Marriage | 5833 (76.6) | 944 (86.3) | 1146 (82) | 1380 (76.5) | 2363 (71.2) |
| Married: Non-first Marriage | 141 (1.9) | 23 (2.1) | 21 (1.5) | 25 (1.4) | 72 (2.2) |
| Divorced | 82 (1.1) | 9 (0.8) | 17 (1.2) | 14 (0.8) | 42 (1.3) |
| Widowed | 62 (0.8) | 4 (0.4) | 21 (1.5) | 10 (0.6) | 27 (0.8) |
| Cohabitation | 72 (0.9) | 15 (1.4) | 8 (0.6) | 14 (0.8) | 35 (1.1) |
| Education Level | |||||
| Primary School or Below | 2263 (29.7) | 325 (29.7) | 366 (26.2) | 568 (31.5) | 1004 (30.3) |
| Secondary School | 2618 (34.4) | 429 (39.2) | 493 (35.3) | 611 (33.8) | 1085 (32.7) |
| High School or Equivalent | 1355 (17.8) | 177 (16.2) | 229 (16.4) | 331 (18.3) | 618 (18.6) |
| Undergraduate or Above | 1381 (18.1) | 163 (14.9) | 310 (22.2) | 296 (16.4) | 612 (18.4) |
| Social Support | |||||
| No Support | 1022 (13.4) | 144 (13.2) | 242 (17.3) | 208 (11.5) | 428 (12.9) |
| Low Support | 1508 (19.8) | 256 (23.4) | 330 (23.6) | 346 (19.2) | 576 (17.4) |
| Moderate Support | 2789 (36.6) | 403 (36.8) | 479 (34.3) | 694 (38.4) | 1213 (36.5) |
| High Support | 2298 (30.2) | 291 (26.6) | 347 (24.8) | 558 (30.9) | 1102 (33.2) |
| Self-reported Health Status | |||||
| Excellent | 1925 (25.3) | 231 (21.1) | 322 (23) | 429 (23.8) | 943 (28.4) |
| Good | 3328 (43.7) | 462 (42.2) | 600 (42.9) | 792 (43.9) | 1474 (44.4) |
| Fair | 1750 (23) | 303 (27.7) | 379 (27.1) | 397 (22) | 671 (20.2) |
| Poor | 540 (7.1) | 87 (8.0) | 88 (6.3) | 169 (9.4) | 196 (5.9) |
| Very Poor | 74 (1.0) | 11 (1.0) | 9 (0.6) | 19 (1.1) | 35 (1.1) |
| Tobacco Use | |||||
| Non-smokers | 7524 (98.8) | 1072 (98.0) | 1390 (99.4) | 1767 (97.8) | 3295 (99.3) |
| Smokers | 93 (1.2) | 22 (2.0) | 8 (0.6) | 39 (2.2) | 24 (0.7) |
| Alcohol Use | |||||
| Less than once a week | 7437 (97.6) | 1052 (96.2) | 1373 (98.2) | 1747 (96.7) | 3265 (98.4) |
| Once a week or more | 180 (2.4) | 42 (3.8) | 25 (1.8) | 59 (3.3) | 54 (1.6) |
| Work Place | |||||
| Outdoors | 1723 (22.6) | 236 (21.6) | 213 (15.2) | 473 (26.2) | 801 (24.1) |
| Factory Workshop | 690 (9.1) | 156 (14.3) | 186 (13.3) | 138 (7.6) | 210 (6.3) |
| Indoor Business Places | 1020 (13.4) | 194 (17.7) | 272 (19.5) | 206 (11.4) | 348 (10.5) |
| Office | 1190 (15.6) | 188 (17.2) | 271 (19.4) | 293 (16.2) | 438 (13.2) |
| Home | 294 (3.9) | 42 (3.8) | 71 (5.1) | 71 (3.9) | 110 (3.3) |
| Unfixed or Other | 2700 (35.4) | 278 (25.4) | 385 (27.5) | 625 (34.6) | 1412 (42.5) |
| Variables | Univariate Logistic Regression | Multivariate Logistic Regression | ||
|---|---|---|---|---|
| OR (95% CI) | p–Value | OR (95% CI) | p–Value | |
| Age Group | ||||
| 15–19 | Reference | Reference | ||
| 20–29 | 1.16 (0.72–1.91) | 0.538 | 1.18 (0.69–2.04) | 0.554 |
| 30–39 | 1.41 (0.87–2.30) | 0.166 | 1.21 (0.68–2.18) | 0.512 |
| 40–49 | 1.35 (0.84–2.20) | 0.223 | 1.07 (0.60–1.93) | 0.827 |
| Marital Status | ||||
| Single | Reference | Reference | ||
| Married: First Marriage | 1.54 (1.19–2.00) | 0.001 | 1.24 (0.89–1.73) | 0.207 |
| Married: Non–first Marriage | 2.05 (1.08–3.91) | 0.028 | 1.46 (0.72–2.95) | 0.291 |
| Divorced | 0.99 (0.41–2.25) | 0.98 | 0.94 (0.37–2.25) | 0.896 |
| Widowed | 0.36 (0.10–0.97) | 0.065 | 0.21 (0.06–0.62) | 0.009 |
| Cohabitation | 3.50 (1.47–8.97) | 0.006 | 3.01 (1.24–7.86) | 0.018 |
| Education Level | ||||
| Primary School or Below | Reference | Reference | ||
| Secondary School | 0.98 (0.80–1.19) | 0.841 | 1.02 (0.82–1.27) | 0.853 |
| High School or Equivalent | 0.87 (0.68–1.11) | 0.27 | 0.94 (0.71–1.24) | 0.653 |
| Undergraduate or Above | 0.59 (0.46–0.75) | <0.001 | 0.58 (0.42–0.79) | 0.001 |
| Social Support | ||||
| None Support | Reference | Reference | ||
| Low Support | 1.30 (1.00–1.70) | 0.048 | 1.34 (1.03–1.76) | 0.032 |
| Moderate Support | 1.41 (1.11–1.81) | 0.006 | 1.51 (1.18–1.95) | 0.001 |
| High Support | 1.41 (1.09–1.83) | 0.009 | 1.59 (1.22–2.08) | 0.001 |
| Self–reported Health Status | ||||
| Excellent | Reference | Reference | ||
| Good | 1.07 (0.87–1.32) | 0.505 | 1.06 (0.85–1.31) | 0.607 |
| Fair | 1.11 (0.89–1.40) | 0.349 | 1.00 (0.79–1.27) | 0.987 |
| Poor | 1.38 (0.98–1.94) | 0.065 | 1.28 (0.89–1.84) | 0.188 |
| Very Poor | 1.70 (0.69–4.29) | 0.244 | 1.73 (0.67–4.59) | 0.255 |
| Tobacco Use | ||||
| Non–smokers | Reference | Reference | ||
| Smokers | 3.57 (1.65–8.56) | 0.002 | 3.50 (1.55–8.78) | 0.004 |
| Alcohol Use | ||||
| Less than once a week | Reference | Reference | ||
| Once a week or more | 2.19 (1.34–3.67) | 0.002 | 2.24 (1.34–3.81) | 0.002 |
| Work Place | ||||
| Outdoors | Reference | Reference | ||
| Factory Workshop | 0.76 (0.57–1.00) | 0.053 | 0.77 (0.57–1.03) | 0.074 |
| Indoor Business Places | 0.64 (0.50–0.84) | 0.001 | 0.68 (0.51–0.90) | 0.008 |
| Office | 0.63 (0.48–0.81) | <0.001 | 0.86 (0.62–1.18) | 0.343 |
| Home | 0.53 (0.35–0.81) | 0.004 | 0.55 (0.35–0.85) | 0.007 |
| Unfixed or Other | 0.65 (0.51–0.83) | <0.001 | 0.69 (0.53–0.89) | 0.004 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gong, X.; Luo, X.; Ling, L. Prevalence and Associated Factors of Secondhand Smoke Exposure among Internal Chinese Migrant Women of Reproductive Age: Evidence from China’s Labor-Force Dynamic Survey. Int. J. Environ. Res. Public Health 2016, 13, 371. https://doi.org/10.3390/ijerph13040371
Gong X, Luo X, Ling L. Prevalence and Associated Factors of Secondhand Smoke Exposure among Internal Chinese Migrant Women of Reproductive Age: Evidence from China’s Labor-Force Dynamic Survey. International Journal of Environmental Research and Public Health. 2016; 13(4):371. https://doi.org/10.3390/ijerph13040371
Chicago/Turabian StyleGong, Xiao, Xiaofeng Luo, and Li Ling. 2016. "Prevalence and Associated Factors of Secondhand Smoke Exposure among Internal Chinese Migrant Women of Reproductive Age: Evidence from China’s Labor-Force Dynamic Survey" International Journal of Environmental Research and Public Health 13, no. 4: 371. https://doi.org/10.3390/ijerph13040371






