The Association of Ideal Cardiovascular Health and Atherogenic Index of Plasma in Rural Population: A Cross-Sectional Study from Northeast China
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Ethical Statement
2.3. Data Collection
2.4. Smoking Status
2.5. Diet Score
2.6. Physical Activity
2.7. Category of Blood Pressure (BP)
2.8. Category of BMI
2.9. Serum Analysis
2.10. Definition of AIP and Ideal CVH
2.11. Statistical Analyses
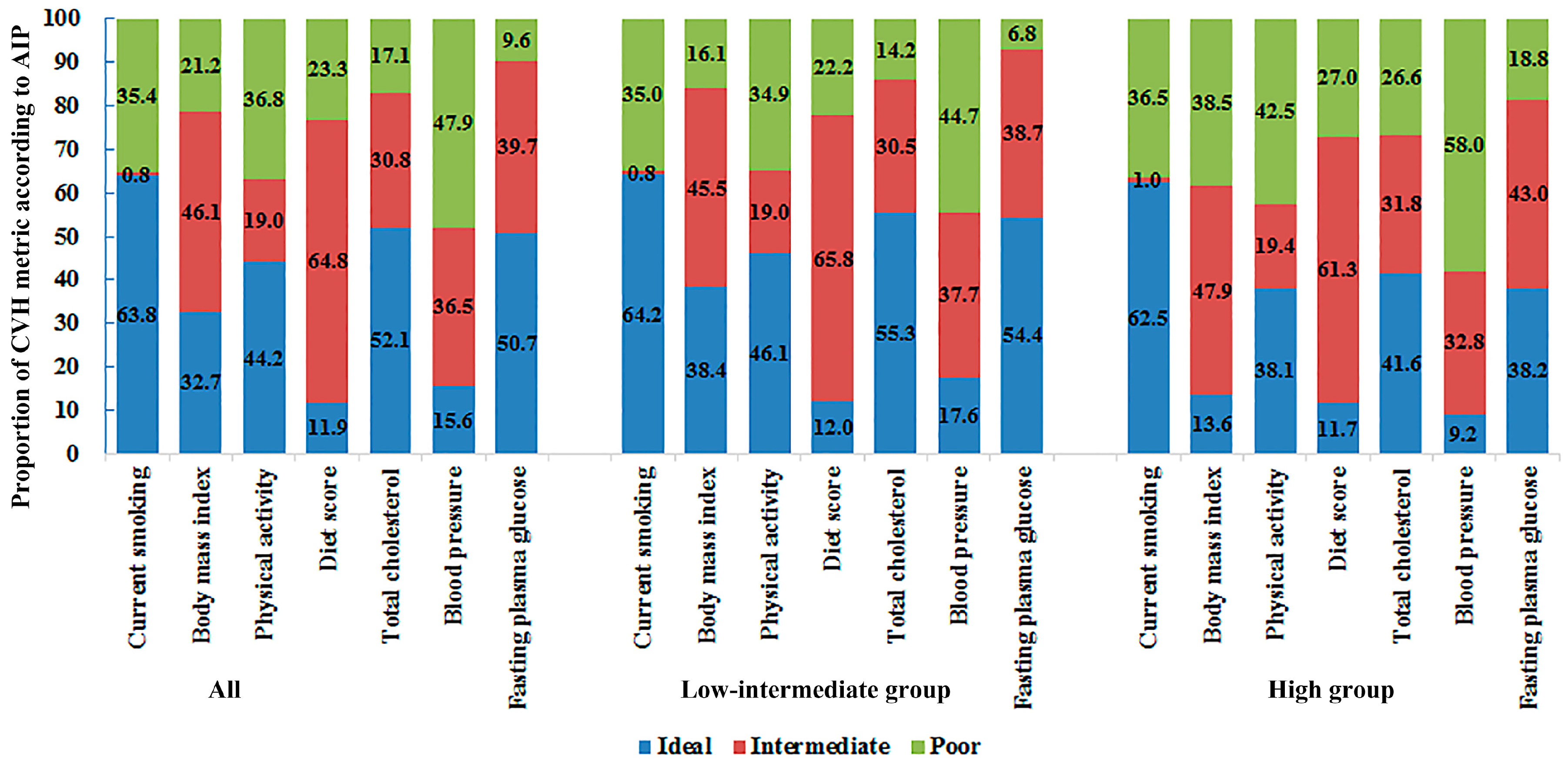
3. Results
4. Discussion
5. Limitations
6. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Lloyd-Jones, D.; Adams, R.J.; Brown, T.M.; Carnethon, M.; Dai, S.; De Simone, G.; Ferguson, T.B.; Ford, E.; Furie, K.; Gillespie, C.; et al. Heart disease and stroke statistics—2010 update: A report from the American Heart Association. Circulation 2010, 121, e46–e215. [Google Scholar] [PubMed]
- Capewell, S.; Ford, E.S.; Croft, J.B.; Critchley, J.A.; Greenlund, K.J.; Labarthe, D.R. Cardiovascular risk factor trends and potential for reducing coronary heart disease mortality in the United States of America. Bull. WHO 2010, 88, 120–130. [Google Scholar] [PubMed]
- Ford, E.S.; Capewell, S. Proportion of the decline in cardiovascular mortality disease due to prevention versus treatment: Public health versus clinical care. Annu. Rev. Public Health 2011, 32, 5–22. [Google Scholar] [CrossRef] [PubMed]
- Ford, E.S.; Ajani, U.A.; Croft, J.B.; Critchley, J.A.; Labarthe, D.R.; Kottke, T.E.; Giles, W.H.; Capewell, S. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N. Engl. J. Med. 2007, 356, 2388–2398. [Google Scholar] [CrossRef] [PubMed]
- IOM (Institute of Medicine). Promoting Cardiovascular Health in the Developing World: A Critical Challenge to Achieve Global Health; Fuster, V., Kelly, B.B., Eds.; National Academies Press: Washington, DC, USA, 2010. [Google Scholar]
- Jankovic, S.; Stojisavljevic, D.; Jankovic, J.; Eric, M.; Marinkovic, J. Status of cardiovascular health in a transition European country: Findings from a population-based cross-sectional study. Int. J. Public Health 2014, 59, 769–778. [Google Scholar] [CrossRef] [PubMed]
- Yang, G.; Kong, L.; Zhao, W.; Wan, X.; Zhai, Y.; Chen, L.C.; Koplan, J.P. Emergence of chronic non-communicable diseases in China. Lancet 2008, 372, 1697–1705. [Google Scholar] [CrossRef]
- National Center for Cardiovascular Diseases, China. Report on Cardiovascular Diseases in China (2016); Encyclopedia of China Publishing House: Beijing, China, 2015. [Google Scholar]
- Lloyd-Jones, D.M.; Hong, Y.; Labarthe, D.; Mozaffarian, D.; Appel, L.J.; Van Horn, L.; Greenlund, K.; Daniels, S.; Nichol, G.; Tomaselli, G.F.; et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: The American Heart Association’s strategic impact goal through 2020 and beyond. Circulation 2010, 121, 586–613. [Google Scholar] [CrossRef] [PubMed]
- Dong, C.; Rundek, T.; Wright, C.B.; Anwar, Z.; Elkind, M.S.; Sacco, R.L. Ideal cardiovascular health predicts lower risks of myocardial infarction, stroke, and vascular death across whites, blacks, and hispanics: The Northern Manhattan Study. Circulation 2012, 125, 2975–2984. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Zhou, Y.; Gao, X.; Wang, C.; Zhang, S.; Wang, A.; Li, N.; Bian, L.; Wu, J.; Jia, Q.; et al. Ideal cardiovascular health metrics and the risks of ischemic and intracerebral hemorrhagic stroke. Stroke 2013, 44, 2451–2456. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.; Guo, X.; Chen, Y.; Guo, L.; Li, Z.; Yu, S.; Yang, H.; Sun, G.; Sun, Y. Prevalence and metrics distribution of ideal cardiovascular health: A population-based, cross-sectional study in rural China. Heart Lung Circ. 2016, 25, 982–992. [Google Scholar] [CrossRef] [PubMed]
- Kulshreshtha, A.; Goyal, A.; Veledar, E.; McClellan, W.; Judd, S.; Eufinger, S.C.; Bremner, J.D.; Goldberg, J.; Vaccarino, V. Association between ideal cardiovascular health and carotid intima-media thickness: A twin study. J. Am. Heart Assoc. 2014, 3, e000282. [Google Scholar] [CrossRef] [PubMed]
- Pahkala, K.; Hietalampi, H.; Laitinen, T.T.; Viikari, J.S.A.; Ronnemaa, T.; Niinikoski, H.; Lagstrom, H.; Talvia, S.; Jula, A.; Heinonen, O.J.; et al. Ideal cardiovascular health in adolescence: Effect of lifestyle intervention and association with vascular intima-media thickness and elasticity (the STRIP study). Circulation 2013, 127, 2088–2096. [Google Scholar] [CrossRef] [PubMed]
- Luo, T.Y.; Liu, X.H.; Dai, T.Y.; Liu, X.M.; Zhang, Q.; Dong, J.Z. Ideal cardiovascular health metrics and coronary artery calcification in northern Chinese population: A cross-sectional study. Biomed. Environ. Sci. 2016, 29, 475–483. [Google Scholar] [PubMed]
- Shen, S.W.; Lu, Y.; Li, F.; Shen, Z.H.; Xu, M.; Yao, W.F.; Feng, Y.B.; Yun, J.T.; Wang, Y.P.; Ling, W.; et al. Potential long-term effects of previous schistosome infection may reduce the atherogenic index of plasma in Chinese men. Int. J. Parasitol. 2015, 45, 289–294. [Google Scholar] [CrossRef] [PubMed]
- Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA 2001, 285, 2486–2497. [Google Scholar]
- Dobiasova, M.; Frohlich, J. The plasma parameter log (TG/HDL-C) as an atherogenic index: Correlation with lipoprotein particle size and esterification rate in apob-lipoprotein-depleted plasma (FERHDL). Clin. Biochem. 2001, 34, 583–588. [Google Scholar] [CrossRef]
- Dobiasova, M.; Frohlich, J. The new atherogenic plasma index reflects the triglyceride and HDL-cholesterol ratio, the lipoprotein particle size and the cholesterol esterification rate: Changes during lipanor therapy. Vnitrni Lekarstvi 2000, 46, 152–156. [Google Scholar] [PubMed]
- Dobiasova, M.; Urbanova, Z.; Samanek, M. Relations between particle size of HDL and LDL lipoproteins and cholesterol esterification rate. Physiol. Res. 2005, 54, 159–165. [Google Scholar] [PubMed]
- Onat, A.; Can, G.; Kaya, H.; Hergenc, G. “Atherogenic index of plasma” (log10 triglyceride/high-density lipoprotein-cholesterol) predicts high blood pressure, diabetes, and vascular events. J. Clin. Lipidol. 2010, 4, 89–98. [Google Scholar] [CrossRef] [PubMed]
- Niroumand, S.; Khajedaluee, M.; Khadem-Rezaiyan, M.; Abrishami, M.; Juya, M.; Khodaee, G.; Dadgarmoghaddam, M. Atherogenic index of plasma (AIP): A marker of cardiovascular disease. Med. J. Islam. Repub. Iran 2015, 29, 240. [Google Scholar] [PubMed]
- Shen, S.; Lu, Y.; Qi, H.; Li, F.; Shen, Z.; Wu, L.; Yang, C.; Wang, L.; Shui, K.; Wang, Y.; et al. Association between ideal cardiovascular health and the atherogenic index of plasma. Medicine 2016, 95, e3866. [Google Scholar] [CrossRef] [PubMed]
- Ge, K. The transition of Chinese dietary guidelines and food guide pagoda. Asia Pac. J. Clin. Nutr. 2011, 20, 439–446. [Google Scholar] [PubMed]
- Hu, G.; Tuomilehto, J.; Silventoinen, K.; Barengo, N.; Jousilahti, P. Joint effects of physical activity, body mass index, waist circumference and waist-to-hip ratio with the risk of cardiovascular disease among middle-aged Finnish men and women. Eur. Heart J. 2004, 25, 2212–2219. [Google Scholar] [CrossRef] [PubMed]
- Pickering, T.G.; Hall, J.E.; Appel, L.J.; Falkner, B.E.; Graves, J.; Hill, M.N.; Jones, D.W.; Kurtz, T.; Sheps, S.G.; Roccella, E.J. Recommendations for blood pressure measurement in humans and experimental animals part 1: Blood pressure measurement in humans: A statement for professionals from the subcommittee of professional and public education of the American Heart Association Council on high blood pressure research. Circulation 2005, 111, 697–716. [Google Scholar] [PubMed]
- Appropriate Body-Mass Index for Asian Populations and Its Implications for Policy and Intervention Strategies. Avaliable online: http://www.who.int/nutrition/publications/bmi_asia_strategies.pdf (accessed on 10 January 2004).
- Raslova, K.; Dobiasova, M.; Hubacek, J.A.; Bencova, D.; Sivakova, D.; Dankova, Z.; Franekova, J.; Jabor, A.; Gasparovic, J.; Vohnout, B. Association of metabolic and genetic factors with cholesterol esterification rate in HDL plasma and atherogenic index of plasma in a 40 years old Slovak population. Physiol. Res. 2011, 60, 785–795. [Google Scholar] [PubMed]
- Akbas, E.M.; Timuroglu, A.; Ozcicek, A.; Ozcicek, F.; Demirtas, L.; Gungor, A.; Akbas, N. Association of uric acid, atherogenic index of plasma and albuminuria in diabetes mellitus. Int. J. Clin. Exp. Med. 2014, 7, 5737–5743. [Google Scholar] [PubMed]
- Folsom, A.R.; Yatsuya, H.; Nettleton, J.A.; Lutsey, P.L.; Cushman, M.; Rosamond, W.D.; Investigators, A.S. Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J. Am. Coll. Cardiol. 2011, 57, 1690–1696. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Zhang, S.; Wang, C.; Gao, X.; Zhou, Y.; Zhou, H.; Wang, A.; Wu, J.; Bian, L.; Wu, S.; et al. Ideal cardiovascular health metrics on the prevalence of asymptomatic intracranial artery stenosis: A cross-sectional study. PLoS ONE 2013, 8, e58923. [Google Scholar] [CrossRef] [PubMed]
- Saleem, Y.; DeFina, L.F.; Radford, N.B.; Willis, B.L.; Barlow, C.E.; Gibbons, L.W.; Khera, A. Association of a favorable cardiovascular health profile with the presence of coronary artery calcification. Circ. Cardiovasc. Imaging 2015, 8, e001851. [Google Scholar] [CrossRef] [PubMed]
- Nansseu, J.R.; Moor, V.J.; Nouaga, M.E.; Zing-Awona, B.; Tchanana, G.; Ketcha, A. Atherogenic index of plasma and risk of cardiovascular disease among Cameroonian postmenopausal women. Lipids Health Dis. 2016, 15, 49. [Google Scholar] [CrossRef] [PubMed]
- Nunes, S.O.; Piccoli de Melo, L.G.; Pizzo de Castro, M.R.; Barbosa, D.S.; Vargas, H.O.; Berk, M.; Maes, M. Atherogenic index of plasma and atherogenic coefficient are increased in major depression and bipolar disorder, especially when comorbid with tobacco use disorder. J. Affect. Disord. 2015, 172, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Sturlaugsdottir, R.; Aspelund, T.; Bjornsdottir, G.; Sigurdsson, S.; Eiriksdottir, G.; Imai, C.M.; Garcia, M.; Launer, L.J.; Harris, T.B.; Gudnason, V. Carotid atherosclerosis and cardiovascular health metrics in old subjects from the AGES-Reykjavik study. Atherosclerosis 2015, 242, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Bambs, C.; Kip, K.E.; Dinga, A.; Mulukutla, S.R.; Aiyer, A.N.; Reis, S.E. Low prevalence of “ideal cardiovascular health” in a community-based population: The heart strategies concentrating on risk evaluation (heart score) study. Circulation 2011, 123, 850–857. [Google Scholar] [CrossRef] [PubMed]
- Halverstadt, A.; Phares, D.A.; Wilund, K.R.; Goldberg, A.P.; Hagberg, J.M. Endurance exercise training raises high-density lipoprotein cholesterol and lowers small low-density lipoprotein and very low-density lipoprotein independent of body fat phenotypes in older men and women. Metabolism 2007, 56, 444–450. [Google Scholar] [CrossRef] [PubMed]
- Kraus, W.E.; Houmard, J.A.; Duscha, B.D.; Knetzger, K.J.; Wharton, M.B.; McCartney, J.S.; Bales, C.W.; Henes, S.; Samsa, G.P.; Otvos, J.D.; et al. Effects of the amount and intensity of exercise on plasma lipoproteins. N. Engl. J. Med. 2002, 347, 1483–1492. [Google Scholar] [CrossRef] [PubMed]
- Silva, R.C.; Diniz Mde, F.; Alvim, S.; Vidigal, P.G.; Fedeli, L.M.; Barreto, S.M. Physical activity and lipid profile in the ELSA-Brasil study. Arq. Bras. Cardiol. 2016, 107, 10–19. [Google Scholar] [CrossRef] [PubMed]
| Variables | Total (n = 11,113) | Low-Intermediate AIP (n = 8541) | High AIP (n = 2572) | p-Value |
|---|---|---|---|---|
| Age (year) | 53.8 ± 10.6 | 53.8 ± 10.7 | 54.4 ± 10.2 | <0.01 |
| Male (%) | 5129 (46.2) | 3909 (45.8) | 1220 (47.4) | 0.137 |
| Spouse (live, %) | 10,261 (91.6) | 7814 (91.5) | 2369 (92.1) | 0.320 |
| Education (%) | 0.325 | |||
| Primary school or below | 5528 (49.7) | 4192 (49.1) | 1336 (51.9) | |
| Middle school | 4539 (40.8) | 3573 (41.8) | 996 (37.6) | |
| High school or above | 1046 (9.4) | 776 (9.1) | 270 (10.5) | |
| Family income (CNY/year, %) | 0.248 | |||
| ≤5000 | 1375 (12.4) | 1047 (12.3) | 328 (12.8) | |
| 5000–20,000 | 6060 (54.5) | 4710 (55.1) | 1350 (52.5) | |
| >20,000 | 3678 (33.1) | 2784 (32.6) | 894 (34.7) | |
| Race | 0.20 | |||
| Han | 10,540 (94.8) | 8088 (94.7) | 2452 (95.3) | |
| Others a | 573 (5.2) | 453 (5.3) | 120 (4.7) | |
| Current smoking status (%) | 3932 (35.4) | 2994 (35.1) | 938 (36.5) | 0.190 |
| Current drinking status (%) | 2502 (22.5) | 1969 (23.1) | 533 (20.7) | <0.05 |
| Diet score | 2.33 ± 1.13 | 2.35 ± 1.11 | 2.26 ± 1.17 | <0.001 |
| SBP (mmHg) | 141.6 ± 23.4 | 140.2 ± 23.3 | 146.3 ± 23.3 | <0.001 |
| DBP (mmHg) | 82.0 ± 11.8 | 81.1 ± 11.6 | 85.1 ± 11.9 | <0.001 |
| BMI (kg/m2) | 24.8 ± 3.7 | 24.2 ± 3.5 | 26.6 ± 3.5 | <0.001 |
| WC (cm) | 82.4 ± 9.8 | 81.8 ± 9.5 | 87.9 ± 8.9 | <0.001 |
| FPG (mmol/L) | 5.90 ± 1.64 | 5.75 ± 1.38 | 6.42 ± 2.22 | <0.001 |
| TC (mmol/L) | 5.24 ± 1.09 | 5.13 ± 1.01 | 5.57 ± 1.26 | <0.001 |
| TG (mmol/L) | 1.64 ± 1.51 | 1.13 ± 0.44 | 3.32 ± 2.34 | <0.001 |
| LDL-C (mmol/L) | 2.93 ± 0.82 | 2.87 ± 0.79 | 3.10 ± 0.91 | <0.001 |
| HDL-C (mmol/L) | 1.41 ± 0.38 | 1.49 ± 0.38 | 1.12 ± 0.22 | <0.001 |
| AIP | −0.089 ± 0.315 | −0.140 ± 0.210 | 0.425 ± 0.194 | <0.001 |
| Metrics | β | p |
|---|---|---|
| Current smoking | 0.083 | <0.001 |
| Body mass index | 0.305 | <0.001 |
| Physical activity | 0.067 | <0.001 |
| Diet score | −0.045 | <0.001 |
| Total cholesterol | 0.148 | <0.001 |
| Systolic blood pressure | −0.108 | <0.001 |
| Diastolic blood pressure | 0.140 | <0.001 |
| Fasting plasma glucose | 0.134 | <0.001 |
| Metrics | Prevalence Ratio | 95% CI | p-Value |
|---|---|---|---|
| Current smoking | |||
| Ideal | 1.00 | ||
| Intermediate | 1.24 | 0.79–2.00 | 0.346 |
| Poor | 1.26 | 1.13–1.40 | <0.001 |
| Body mass index | |||
| Ideal | 1.00 | ||
| Intermediate | 2.33 | 2.05–2.65 | <0.001 |
| Poor | 3.76 | 3.27–4.32 | <0.001 |
| Physical activity | |||
| Ideal | 1.00 | ||
| Intermediate | 1.14 | 1.01–1.29 | <0.05 |
| Poor | 1.21 | 1.09–1.35 | <0.001 |
| Diet score | |||
| Ideal | 1.00 | ||
| Intermediate | 1.00 | 0.87–1.15 | 0.999 |
| Poor | 1.30 | 1.11–1.53 | <0.001 |
| Total cholesterol | |||
| Ideal | 1.00 | ||
| Intermediate | 1.15 | 1.03–1.27 | <0.05 |
| Poor | 1.56 | 1.39–1.75 | <0.001 |
| Blood pressure | |||
| Ideal | 1.00 | ||
| Intermediate | 1.22 | 1.04–1.43 | <0.05 |
| Poor | 1.31 | 1.12–1.54 | <0.001 |
| Fasting plasma glucose | |||
| Ideal | 1.00 | ||
| Intermediate | 1.25 | 1.13–1.38 | <0.001 |
| Poor | 1.90 | 1.66–2.18 | <0.001 |
| Number of Ideal CVH Metrics | Total Number (%) in Category | Number at High AIP Group (% Having a High AIP in Category) | Prevalence Ratio (95% CI) |
|---|---|---|---|
| 7 | 14 (0.1) | 0 (0) | (5–7 ideal CVH metrics) |
| 6 | 208 (1.9) | 18 (8.7) | |
| 5 | 816 (7.3) | 63 (7.7) | |
| 4 | 1996 (18.0) | 250 (12.5) | 1.67 (1.28, 2.17) |
| 3 | 2982 (26.8) | 578 (19.4) | 2.66 (2.08, 3.40) |
| 2 | 2989 (26.9) | 853 (28.5) | 4.00 (3.14, 5.09) |
| 1 | 1785 (16.1) | 666 (37.3) | 5.30 (4.13, 6.79) |
| 0 | 323 (2.9) | 144 (44.6) | 6.50 (4.79, 8.83) |
| Categories of CVH Metrics | Total Number (%) in Category | Number at High AIP Group (% Having a High AIP in Category) | Prevalence Ratio (95% CI) |
|---|---|---|---|
| Ideal | 14 (0.1) | 0 (0) | (ideal + intermediate) |
| Intermediate | 1300 (11.7) | 122 (9.4) | |
| Poor | 9799 (88.2) | 2450 (25.0) | 2.73 (2.25, 3.31) |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, Y.; Li, Y.; Guo, X.; Dai, D.; Sun, Y. The Association of Ideal Cardiovascular Health and Atherogenic Index of Plasma in Rural Population: A Cross-Sectional Study from Northeast China. Int. J. Environ. Res. Public Health 2016, 13, 1027. https://doi.org/10.3390/ijerph13101027
Chang Y, Li Y, Guo X, Dai D, Sun Y. The Association of Ideal Cardiovascular Health and Atherogenic Index of Plasma in Rural Population: A Cross-Sectional Study from Northeast China. International Journal of Environmental Research and Public Health. 2016; 13(10):1027. https://doi.org/10.3390/ijerph13101027
Chicago/Turabian StyleChang, Ye, Yuan Li, Xiaofan Guo, Dongxue Dai, and Yingxian Sun. 2016. "The Association of Ideal Cardiovascular Health and Atherogenic Index of Plasma in Rural Population: A Cross-Sectional Study from Northeast China" International Journal of Environmental Research and Public Health 13, no. 10: 1027. https://doi.org/10.3390/ijerph13101027






