The Impact of Educational Attainment on Observed Race/Ethnic Disparities in Inflammatory Risk in the 2001–2008 National Health and Nutrition Examination Survey
Abstract
:1. Introduction
2. Methods
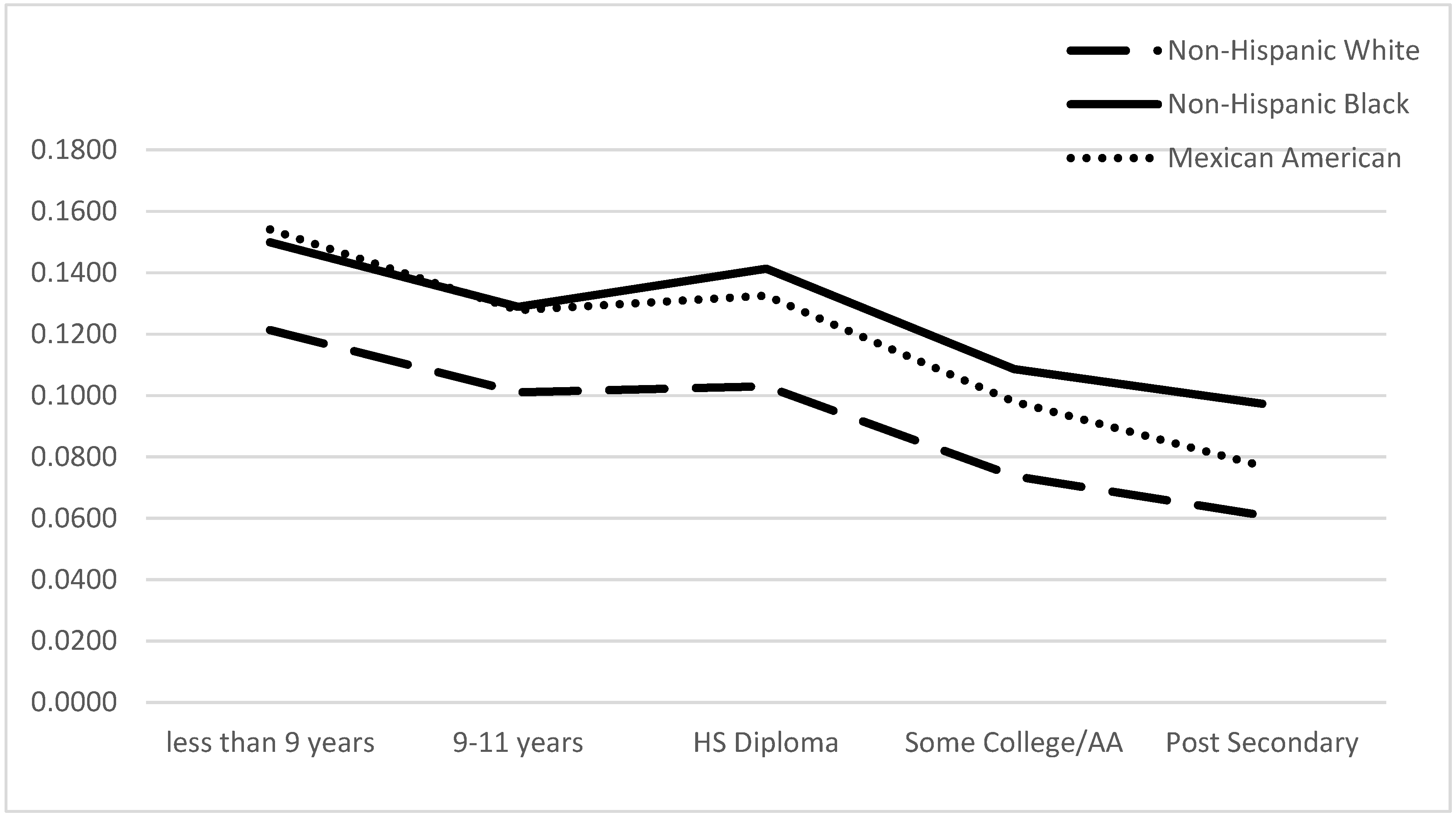
3. Results
| Variable | Non-Hispanic White n = 13,362 | Non-Hispanic Black n = 7696 | Mexican American n = 4545 | p-Value |
|---|---|---|---|---|
| Age | ||||
| 20–34 | 26.7% | 36.8% | 49.6% | p ≤ 0.001 |
| 35–44 | 19.2 | 20.3 | 17.5 | |
| 45–54 | 21.7 | 19.8 | 14.7 | |
| 55–64 | 13.6 | 11.7 | 9.3 | |
| 65+ | 18.8 | 11.3 | 8.9 | |
| Sex | ||||
| Female | 50.9% | 54.0% | 51.3% | p ≤ 0.001 |
| Male | 49.1 | 46.0 | 48.7 | |
| Income | ||||
| Less than 25,000 | 18.7% | 37.9% | 31.1% | p ≤ 0.001 |
| 25,000–44,999 | 21.3 | 26.0 | 28.1 | |
| 45,000–74,000 | 25.1 | 19.3 | 22.2 | |
| 75,000+ | 34.9 | 16.8 | 18.5 | |
| Education | ||||
| Less than 9 years | 3.6% | 5.3% | 8.5% | p ≤ 0.001 |
| 9–11 years | 9.4 | 22.7 | 19.5 | |
| High school diploma/GED | 26.8 | 24.2 | 26.1 | |
| Some college/AA degree | 31.6 | 32.3 | 33.5 | |
| Post Secondary or higher | 28.7 | 15.5 | 12.4 | |
| Health Behaviors | ||||
| Non Smoker | 59.4% | 45.9% | 63.9% | p ≤ 0.001 |
| Smoker | 40.6 | 54.1 | 36.1 | |
| Not Heavy Drinker | 83.9 | 83.7 | 85.2 | |
| Heavy drinker | 16.1 | 16.3 | 14.8 | |
| Health Status | ||||
| Normal Waist Circumference | 34.1% | 40.6% | 49.6% | p ≤ 0.001 |
| High Waist Circumference | 65.9 | 59.4 | 50.4 | |
| Normal Blood Pressure | 84.2 | 81.0 | 90.8 | |
| High Blood Pressure | 15.8 | 19.0 | 9.2 | |
| Diabetic | 6.8 | 9.6 | 5.7 | |
| Statin User | 11.2 | 6.1 | 3.5 | |
| C-Reactive Protein | ||||
| Low | 92.2% | 88.0% | 90.0% | p ≤ 0.001 |
| Intermediate | 6.7 | 10.6 | 7.9 | |
| High | 1.2 | 1.4 | 1.3 |
| Variable | Low CRP | Intermediate CRP | High CRP | p-Value |
|---|---|---|---|---|
| Sex | ||||
| Female | 88.8% | 9.8% | 1.4% | p ≤ 0.001 |
| Male | 94.4 | 4.6 | 1.0 | |
| RACE | ||||
| NHW | 92.2% | 6.7% | 1.2% | p ≤ 0.001 |
| NHB | 88.0 | 10.6 | 1.4 | |
| MA | 90.9 | 7.9 | 1.3 | |
| AGE | ||||
| 20–34 | 92.0% | 6.8% | 1.2% | p ≤ 0.001 |
| 35–44 | 91.6 | 7.3 | 1.1 | |
| 45–54 | 88.9 | 9.8 | 1.2 | |
| 55–64 | 88.4 | 10.3 | 1.4 | |
| 65+ | 88.8 | 9.1 | 2.2 | |
| Income | ||||
| less than 25,000 | 88.8% | 9.7% | 1.6% | p ≤ 0.001 |
| 25,000–44,999 | 90.9 | 7.6 | 1.4 | |
| 45,000–74,000 | 91.4 | 7.4 | 1.2 | |
| 75,000+ | 93.8 | 5.4 | 0.8 | |
| Education | ||||
| less than 9 years | 86.8% | 10.8% | 2.4% | p ≤ 0.001 |
| 9–11 years | 84.6 | 13.2 | 2.2 | |
| HS | 88.8 | 10.0 | 1.2 | |
| Some College | 90.5 | 8.1 | 1.4 | |
| Post-Secondary | 90.1 | 8.5 | 1.4 | |
| Health Behaviors | ||||
| Non smokers | 89.7% | 8.9% | 1.4% | p ≤ 0.001 |
| Smokers | 88.6 | 9.7 | 1.7 | |
| Not Heavy Drinkers | 89.9 | 8.8 | 1.3 | |
| Heavy Drinkers | 91.3 | 7.3 | 1.4 | |
| Health Condition | ||||
| Normal waist | 97.0% | 2.2% | 0.7% | p ≤ 0.001 |
| HWC | 88.9 | 9.7 | 1.4 | |
| Normal Bldpres | 92.0 | 6.8 | 1.1 | |
| High Bldpres | 88.3 | 10.4 | 1.3 | |
| Non Diabetic | 92.2 | 6.7 | 1.1 | |
| Diabetic | 82.4 | 15.2 | 2.4 |
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
|---|---|---|---|---|---|---|---|---|
| CRP Level | ||||||||
| 1–3 mg/dL (95% CI) | >3 mg/dL (95% CI) | 1–3 mg/dL (95% CI) | >3 mg/dL (95% CI) | 1–3 mg/dL (95% CI) | >3 mg/dL (95%CI) | 1–3 mg/dL (95% CI) | >3 mg/dL (95% CI) | |
| Race/ethnicity | ||||||||
| NHW(ref.) | ||||||||
| NHB | 1.66 (1.65–1.66) | 1.31 (1.30–1.31) | 1.52 (1.52–1.52) | 1.20 (1.19–1.21) | 1.69 (1.69–1.70) | 1.36 (1.35–1.36) | 1.31 (1.30–1.32) | 1.14 (1.13–1.15) |
| MA | 1.20 (1.19–1.20) | 1.10 (1.09–1.11) | 1.12 (1.11–1.12) | 1.05 (1.05–1.06) | 1.47 (1.46–1.47) | 1.51 (1.50–1.52) | 0.74 (0.73–0.75) | 0.38 (0.37–0.39) |
| Income | ||||||||
| Less than 25,000 | 1.76 (1.76–1.77) | 1.99 (1.98–2.00) | 1.49 (1.48–1.49) | 2.06 (2.05–2.07) | 1.24 (1.23–1.24) | 3.51 (3.47–3.54) | ||
| 25,000–44,999 | 1.41 (1.40–1.41) | 1.80 (1.78–1.80) | 1.16 (1.15–1.16) | 1.91 (1.90–1.92) | 1.06 (1.05–1.06) | 3.54 (3.51–3.57) | ||
| 45,000–74,000 | 1.39 (1.39–1.39) | 1.48 (1.47–1.49) | 1.22 (1.22–1.22) | 1.58 (1.57–1.58) | 1.11 (1.11–1.12) | 1.75 (1.73–1.76) | ||
| 75,000+ (ref.) | ||||||||
| Education | ||||||||
| Less than 9 years | 1.32 (1.36–1.37) | 1.48 (1.47–1.49) | 1.91 (1.90–1.92) | 1.13 (1.12–1.15) | ||||
| 9–11 years | 1.58 (1.57–1.59) | 1.30 (1.29–1.30) | 1.49 (1.49–1.50) | 0.70 (0.69–0.71) | ||||
| HS/GED | 1.54 (1.53–1.54) | 0.84 (0.83–0.84) | 1.55 (1.54–1.55) | 0.77 (0.77–0.78) | ||||
| SC/AA degree | 1.25 (1.25–1.26) | 0.99 (0.98–0.99) | 1.06 (1.05–1.06) | 1.05 (1.03–1.05) | ||||
| Post-Secondary or Higher (ref.) | ||||||||
| Controls | ||||||||
| Sex (1 = male) | 0.45 (0.45–0.46) | 0.58 (0.57–0.58) | ||||||
| Age | ||||||||
| 20–34 | 0.91 (0.91–0.92) | 0.39 (0.39–0.40) | ||||||
| 35–44 | 0.94 (0.97–0.98) | 0.33 (0.32–0.33) | ||||||
| 45–54 | 1.52 (1.52–1.53) | 0.54 (0.53–0.55) | ||||||
| 55–64 | 1.04 (1.03–1.04) | 0.61 (0.60–0.61) | ||||||
| 65+ (ref.) | ||||||||
| Health behaviors | ||||||||
| Smokers (Yes) | 1.20 (1.19–1.20) | 1.66 (1.65–1.67) | ||||||
| Heavy drinkers (Yes) | 0.89 (0.88–0.89) | 1.08 (1.07–1.09) | ||||||
| Health Status | ||||||||
| HWC | 3.22 (3.20–3.22) | 1.31 (1.30–1.32) | ||||||
| HBP | 1.04 (1.03–1.04) | 0.72 (0.72–0.74) | ||||||
| Diabetes | 1.78 (1.77–1.79) | 0.82 (0.81–0.82) | ||||||
| Statin (Yes) | 1.01 (1.00–1.01) | 1.01 (0.99–1.01) | ||||||
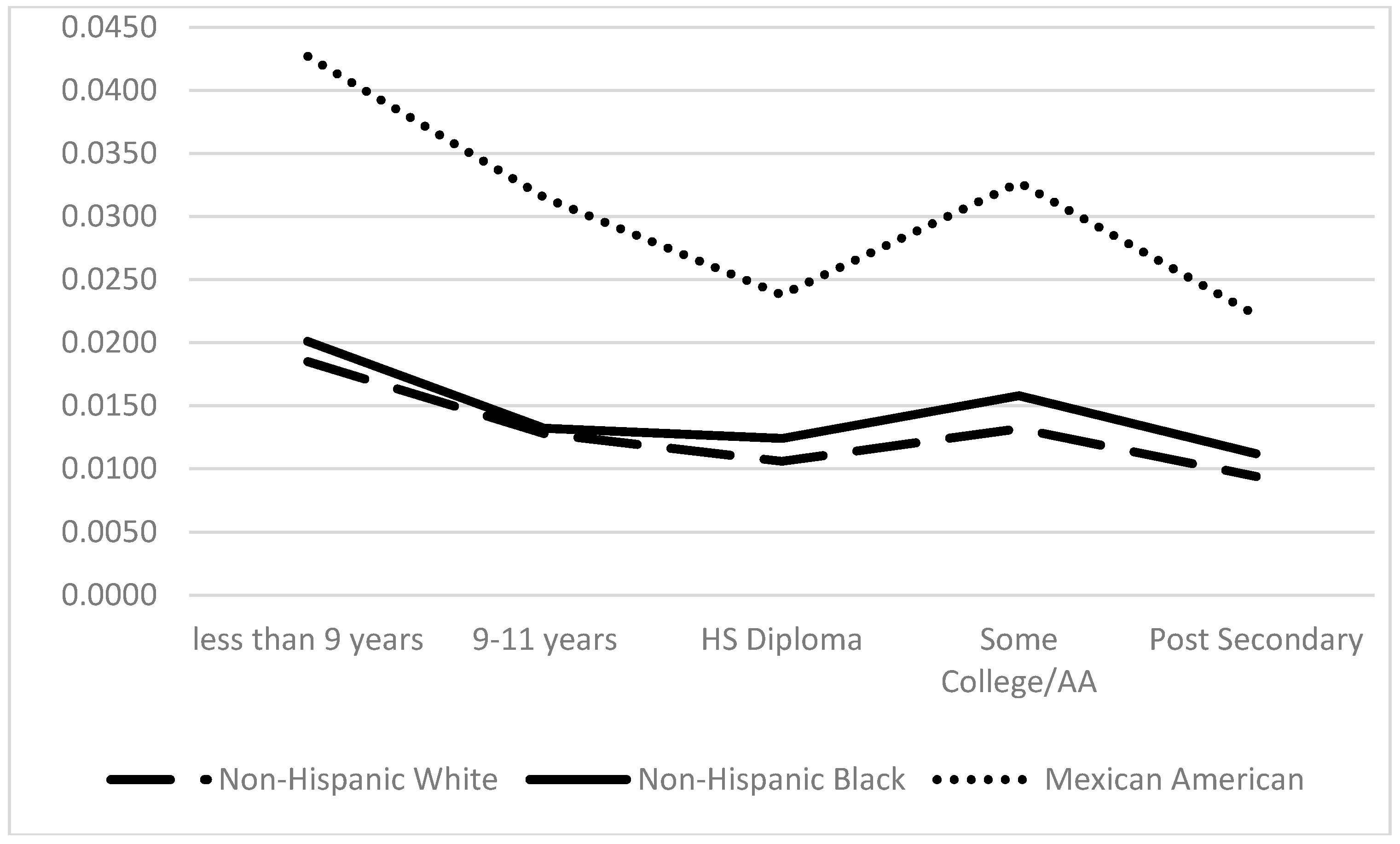
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Lloyd-Jones, D.M.; Hong, Y.; Labarthe, D.; Mozaffarian, D.; Appel, L.J.; van Horn, L.; Greenlund, K.; Daniels, S.; Nichol, G.; Tomaselli, G.F.; et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: The American Heart Association’s strategic impact goal through 2030 and beyond. Circulation 2010, 121, 586–613. [Google Scholar] [CrossRef] [PubMed]
- Lowe, L.P.; Greenland, P.; Ruth, K.J.; Dyer, A.R.; Stamler, R.; Stamler, J. Impact of major cardiovascular disease risk factors, particularly in combination, on 22-year mortality in women and men. Arch. Intern. Med. 1988, 158, 2007–2014. [Google Scholar] [CrossRef]
- Stamler, J.; Dyer, A.R.; Shekelle, R.B.; Neaton, J.; Stamler, R. Relationship of baseline major risk factors to coronary and all-cause mortality, and to longevity: Findings from long-term follow-up of Chicago cohorts. Cardiology 1993, 82, 191–222. [Google Scholar] [CrossRef] [PubMed]
- Heron, M. Deaths: Leading causes for 2008. In National Vital Statistics Reports; National Center for Health Statistics: Hyattsville, MD, USA, 2012; Volume 61. [Google Scholar]
- Dinwiddie, G.Y.; Zambrana, R.E.; Garza, M.E. Exploring risk factors in Latino cardiovascular disease: The role of education, nativity and gender. Am. J. Public Health 2014, 104, 1742–1750. [Google Scholar] [CrossRef] [PubMed]
- Daviglus, M.L.; Talavera, G.A.; Aviles-Santa, L.; Allison, M.; Cai, J.; Criqui, M.H.; Gellman, M.; Giachello, A.L.; Gouskova, N.; Kaplan, R.C.; et al. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. J. Am. Med. Assoc. 2012, 308, 1775–1784. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Kronmal, R.A.; Newman, A.B.; Bild, D.E.; Mittlemark, M.B.; Polak, J.F.; Robbins, J.A.; Gardin, J.M. Risk factors for 5-year mortality in older adults. J. Am. Med. Assoc. 1998, 279, 585–592. [Google Scholar] [CrossRef]
- Geronimus, A.T.; Hicken, M.; Keene, D.; Bound, J. Weathering and age patterns of allostatic load scores among blacks and whites in the United States. Am. J. Public Health 2006, 96, 826–833. [Google Scholar] [CrossRef] [PubMed]
- Seeman, T.E.; McEwen, B.S.; Rowe, J.W.; Singer, B. Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proc. Natl. Acad. Sci. USA 2001, 98, 4770–4775. [Google Scholar] [CrossRef] [PubMed]
- Ridker, P.M.; Cushman, M.; Stampler, M.J.; Tracy, R.P.; Hennekens, C.H. Inflammation, aspirin and the risk of cardiovascular disease in apparently healthy men. N. Engl. J. Med. 1997, 336, 973–979. [Google Scholar] [CrossRef] [PubMed]
- Ridker, P.M.; Cushman, M.; Stampfer, M.J.; Tracy, R.P.; Hennekens, C.H. Plasma concentration of C-reactive protein and risk of developing peripheral vascular disease. Circulation 1998, 97, 425–428. [Google Scholar] [CrossRef] [PubMed]
- Pradhan, A.D.; Manson, J.E.; Rifai, N.; Buring, J.E.; Ridker, P.M. C- reactive protein, interleukin 6, and risk of developing type 2 diabetes mellitus. J. Am. Med. Assoc. 2001, 286, 327–334. [Google Scholar] [CrossRef]
- Harris, T.B.; Ferrucci, L.; Tracy, R.P.; Corti, M.C.; Wacholder, S.; Ettinger, W.H., Jr.; Heimovitz, H.; Cohen, H.J.; Wallace, R. Associations of elevated interleukin-6 and C-reactive protein levels with mortality in the elderly. Am. J. Med. 1999, 106, 506–512. [Google Scholar] [CrossRef]
- Reuben, D.B.; Cheh, A.I.; Harris, T.; Ferrucci, L.; Rowe, J.W.; Tracy, R.P.; Seeman, T.E. Peripheral blood markers of inflammation predict mortality and functional decline in high-functioning community-dwelling older persons. J. Am. Geriatr. Soc. 2002, 50, 638–644. [Google Scholar] [CrossRef]
- Gruenewald, T.L.; Cohen, S.; Matthews, K.A.; Tracy, R.; Seeman, T.E. Association of socioeconomic status with inflammation markers in black and white men and women in the coronary artery risk development in young adults (CARDIA) study. Soc. Sci. Med. 2009, 69, 451–459. [Google Scholar] [CrossRef] [PubMed]
- Beasley, L.E.; Koster, A.; Newman, A.B.; Javaid, M.K.; Ferrucci, L.; Kritchevsky, S.B.; Kuller, L.H.; Pahor, M.; Schaap, L.A.; Visser, M.; et al. Inflammation and race and gender differences in computerized tomography-measured adipose depots. Obesity 2009, 17, 1062–1069. [Google Scholar] [CrossRef] [PubMed]
- Nazmi, A.; Victora, C.G. Socioeconomic and racial/ethnic differentials of C-reactive protein levels: A systematic review of population-based studies. BMC Public Health 2007, 7. [Google Scholar] [CrossRef] [PubMed]
- Khera, A.; McGuire, D.K.; Murphy, S.A.; Stanek, H.G.; Das, S.R.; Vongpatanasin, W.; Wians, F.H., Jr.; Grundy, S.M.; de Lemos, J.A. Race and gender differences in C-reactive protein levels. J. Am. Coll. Cardiol. 2005, 46, 464–469. [Google Scholar] [CrossRef] [PubMed]
- Lynch, J.; Davey Smith, G.; Harper, S.; Hillemeier, M.; Ross, N.; Kaplan, G.A.; Wolfson, M. Is income inequality a determinant of population health? Part I. A systematic review. Millbank Q. 2004, 82, 5–99. [Google Scholar] [CrossRef]
- Koster, A.; Bosma, H.; Penninx, B.W.J.H.; Newman, A.B.; Harris, T.B.; van Eijk, J.T.M.; Kempen, G.I.; Simonsick, E.M.; Johnson, K.C.; Rooks, R.N.; et al. Association of inflammatory markers with socioeconomic status. J. Gerontol. A Biol. Sci. Med. Sci. 2006, 1, 284–290. [Google Scholar] [CrossRef]
- Pollitt, R.; Kaufman, J.; Rose, K.; Diez-Roux, A.V.; Zeng, D.; Heiss, G. Early-life and adult socioeconomic status and inflammatory risk markers in adulthood. Eur. J. Epidemiol. 2007, 22, 55–66. [Google Scholar] [CrossRef] [PubMed]
- Deverts, D.J.; Cohen, S.; Kalra, P.; Matthews, K.A. The prospective association of socioeconomic status with C-reactive protein levels in the CARDIA study. Brain Behav. Immun. 2012, 26, 1128–1135. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, F.; Peralta, C.A.; Green, A.R.; Lopez, L. Comparison of C-reactive protein levels in less versus more acculturated Hispanic adults in the United States (from the National Health and Nutrition Examination Survey 1999–2008). Am. J. Cardiol. 2012, 109, 665–669. [Google Scholar] [CrossRef] [PubMed]
- Ranjit, N.; Diez-Roux, A.V.; Shea, S.; Cushman, M.; Hanyu, N.; Seeman, T. Socioeconomic position, race/ethnicity and inflammation in the Multi-Ethnic Study of Atherosclerosis. Circulation 2007, 116, 2383–2390. [Google Scholar] [CrossRef] [PubMed]
- Herd, P.; Karraker, A.; Friedman, E. The social patterns of a biological risk factor for disease: Race, gender, socioeconomic position and C-reactive protein. J. Gerontol. B Psychol. Sci. Soc. Sci. 2012, 67, 503–513. [Google Scholar] [CrossRef] [PubMed]
- Francus, T.; Romano, P.M.; Manzano, G.; Fonacier, L.; Arango, N.; Szabo, P. IL-1, IL-6, and PDGF mRNA expression in alveolar cells following stimulation with a tobacco-derived antigen. Cell. Immunol. 1992, 145, 156–174. [Google Scholar] [CrossRef]
- Imhof, A.; Froehlich, M.; Brenner, H.; Boeing, H.; Pepys, M.B.; Koenig, W. Effect of alcohol consumption on systemic markers of inflammation. Lancet 2001, 357, 763–767. [Google Scholar] [CrossRef]
- Szeto, Y.; Kwok, T.C.Y.; Benzie, I.F.F. Effects of a long-term vegetarian diet on biomarkers of antioxidant status and cardiovascular disease risk. Nutrition 2004, 20, 863–866. [Google Scholar] [CrossRef] [PubMed]
- Albert, M.A.; Glynn, R.J.; Ridker, P.M. Alcohol consumption and plasma concentration of C-reactive protein. Circulation 2003, 107, 443–447. [Google Scholar] [CrossRef] [PubMed]
- Braveman, P.A.; Cubbin, C.; Egerter, S.; Chideya, S.; Marchi, K.S.; Metzler, M.; Posner, S. Socioeconomic status in health research: On size does not fit all. J. Am. Med. Assoc. 2005, 294, 2879–2888. [Google Scholar] [CrossRef] [PubMed]
- Herd, P.; Goesling, B.; House, J.S. Socioeconomic position and health: The differential effects of education verses income on the onset verses progression of health problems. J. Health Soc. Behav. 2007, 48, 223–238. [Google Scholar] [CrossRef] [PubMed]
- Friedman, E.M.; Herd, P. Income, education and inflammation: Differential associations in a national probability sample (The MIDUS Study). Psychosom. Med. 2010, 72, 290–300. [Google Scholar] [CrossRef] [PubMed]
- National Center for Health Statistics. National Health and Nutrition Examination Survey 2001–2008 Questionnaires, Datasets, and Related Documentation; Centers for disease Control and Prevention: Hyattsville, MD, USA, 2012. Available online: http://www.cdc.gov/nchs/nhanes.htm (accessed on 16 September 2014).
- Pearson, T.A.; Mensah, G.A.; Alexander, R.W.; Anderson, J.L.; Cannon, R.O., 3rd; Criqui, M.; Fadl, Y.Y.; Fortmann, S.P.; Hong, Y.; Myers, G.L.; et al. Markers of inflammation and cardiovascular disease: Application to clinical and public health practice. A statement for healthcare professionals from the centers for disease control and prevention and the American Heart Association. Circulation 2003, 107, 499–511. [Google Scholar] [CrossRef] [PubMed]
- Ridker, P.M. Clinical application of C-reactive protein for cardiovascular disease detection and prevention. Circulation 2003, 107, 363–369. [Google Scholar] [CrossRef] [PubMed]
- Ridker, P.M. C-reactive protein and the prediction of cardiovascular events among those at intermediate risk. J. Am. Coll. Cardiol. 2007, 49, 2129–2138. [Google Scholar] [CrossRef] [PubMed]
- Dinwiddie, G.Y.; Gaskin, D.J.; Chan, K.S.; Norrington, J.; McCleary, R. Residential segregation, geographic proximity and type of services used: Evidence for racial/ethnic disparities in mental health. Soc. Sci. Med. 2013, 80, 67–75. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.; Berenson, A.B. Accuracy of current body mass index obesity classification for white, black and Hispanic reproductive-age women. Obstet. Gynecol. 2010, 115, 982–988. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, J.R.; Heo, M.; Heymsfield, S.V.; Pierson, R.N.; Pi-Sunyer, F.X.; Wang, Z.M.; Wang, J.; Hayes, M.; Allison, D.B.; Gallagher, D. Is percentage body fat differentially related to body mass index in Hispanic Americans, African Americans, and European Americans? Am. J. Clin. Nutr. 2003, 77, 71–75. [Google Scholar] [PubMed]
- Golden, S.H.; Brown, A.; Cauley, J.A.; Chin, M.H.; Gary-Webb, T.L.; Kim, C. Health disparities in endocrine disorders: Biological, clinical, and nonclinical factors—An Endocrine Society scientific statement. J. Clin. Endocrinol. Metab. 2012, 97, E1579–E1639. [Google Scholar] [CrossRef] [PubMed]
- Elo, I.T.; Preston, S.H. Educational differentials in mortality: United States, 1979–1985. Soc. Sci. Med. 1996, 42, 47–57. [Google Scholar] [CrossRef]
- Dinwiddie, G.Y. The health advantages of educational attainment. In International Encyclopedia of Education; Peterson, P., Baker, E., McGaw, B., Eds.; Elsevier: Oxford, UK, 2010; pp. 667–672. [Google Scholar]
- Patel, C.J.; Ioannidis, J.P.; Cullen, M.R.; Rehkoph, D.H. Systematic assessment of the correlations of household income with infectious, biochemical, physiological and environmental factors in the United States, 1999–2006. Am. J. Epidemiol. 2015, 181, 171–179. [Google Scholar] [CrossRef] [PubMed]
- Paalani, M. Determinants of inflammatory markers in a bi-ethnic population. Ethn. Disease 2011, 21, 142–149. [Google Scholar]
- Gallo, L.C.; Fortmann, A.L.; Espinosa De Los Monteros, K.; Mills, P.J.; Barrett-Connor, E.; Roesch, S.C.; Matthews, K.A. Individual and neighborhood socioeconomic status and inflammation in Mexican American women: What is the role of obesity? Psychosom. Med. 2012, 74, 535–542. [Google Scholar] [CrossRef] [PubMed]
- Mirosky, J.; Ross, C. Education, Social Status and Health; Gruyter: New York, NY, USA, 2003. [Google Scholar]
- Kimbro, R.T.; Bzostek, S.; Goldman, N.; Rodriguez, G. Race, ethnicity, and the education gradient in health. Health Aff. 2008, 27, 361–372. [Google Scholar] [CrossRef] [PubMed]
- Karlamangla, A.S.; Merkin, S.S.; Crimmins, E.M.; Seeman, T.E. Socioeconomic and ethnic disparities in cardiovascular risk in the United States, 2001–2006. Ann. Epidemiol. 2010, 20, 617–628. [Google Scholar] [CrossRef] [PubMed]
- Johnson, T.V.; Abbasi, A.; Master, V.A. Systematic review of the evidence of a relationship between chronic psychosocial stress and C-reactive protein. Mol. Diagn. Ther. 2013, 17, 147–164. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dinwiddie, G.Y.; Zambrana, R.E.; Doamekpor, L.A.; Lopez, L. The Impact of Educational Attainment on Observed Race/Ethnic Disparities in Inflammatory Risk in the 2001–2008 National Health and Nutrition Examination Survey. Int. J. Environ. Res. Public Health 2016, 13, 42. https://doi.org/10.3390/ijerph13010042
Dinwiddie GY, Zambrana RE, Doamekpor LA, Lopez L. The Impact of Educational Attainment on Observed Race/Ethnic Disparities in Inflammatory Risk in the 2001–2008 National Health and Nutrition Examination Survey. International Journal of Environmental Research and Public Health. 2016; 13(1):42. https://doi.org/10.3390/ijerph13010042
Chicago/Turabian StyleDinwiddie, Gniesha Y., Ruth E. Zambrana, Lauren A. Doamekpor, and Lenny Lopez. 2016. "The Impact of Educational Attainment on Observed Race/Ethnic Disparities in Inflammatory Risk in the 2001–2008 National Health and Nutrition Examination Survey" International Journal of Environmental Research and Public Health 13, no. 1: 42. https://doi.org/10.3390/ijerph13010042





