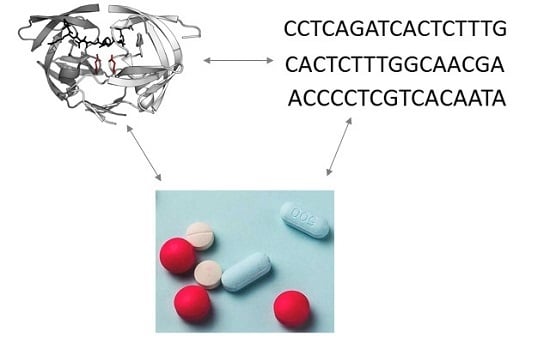
A Computational Approach for the Prediction of Treatment History and the Effectiveness or Failure of Antiretroviral Therapy
Abstract
:1. Introduction
2. Results
2.1. Results of PASS Based Prediction of the Associations between Viral Genotype and Drug Set to which the Virus Was Exposed
2.2. Results of Predicting Association between Nucleotide Sequence, Clinical Parameters, and Immunological Effectiveness/Failure
3. Discussion
3.1. Predicting Drug Exposure
3.2. Predicting Treatment Failure and Treatment Effectiveness
4. Materials and Methods
4.1. Training Sets
4.2. Algorithm
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| HIV-1 | Human Immunodeficiency Virus Type 1 |
| ART | Antiretroviral Therapy |
| RT | Reverse Transcriptase |
| PR | Protease |
| WHO | The World Health Organization |
| PASS | Prediction of Activity Spectra for Substances |
| RF | Random Forest |
| STDB | The Stanford HIV Resistance Database |
| ROC | Receiver Operating Characteristic |
| AUC/ROC | The Area under ROC Curve |
| ATV | Atazanavir |
| APV | Amprenavir |
| DRV | Darunavir |
| FPV | Fosamprenavir |
| DRV | Darunavir |
| IDV | Indinavir |
| LPV | Lopinavir |
| NFV | Nelfinavir |
| RTV | Ritonavir |
| SQV | Saquinavir |
| TPV | Tipranavir |
References
- Zhang, Z.; Li, S.; Gu, Y.; Xia, N. Antiviral Therapy by HIV-1 Broadly Neutralizing and Inhibitory Antibodies. Int. J. Mol. Sci. 2016, 17, 1901. [Google Scholar] [CrossRef]
- Trovato, M.; D’Apice, L.; Prisco, A.; De Berardinis, P. HIV Vaccination: A Roadmap among Advancements and Concerns. Int. J. Mol. Sci. 2018, 19, 1241. [Google Scholar] [CrossRef] [Green Version]
- Cuevas, J.M.; Geller, R.; Garijo, R.; López-Aldeguer, J.; Sanjuán, R. Extremely High Mutation Rate of HIV-1 In Vivo. PLoS Biol. 2015, 13, e1002251. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vansant, G.; Bruggemans, A.; Janssens, J.; Debyser, Z. Block-And-Lock Strategies to Cure HIV Infection. Viruses 2020, 12, 84. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ronsard, L.; Yousif, A.; Ramesh, J.; Sumi, N.; Gorman, M.; Ramachandran, V.; Banerjea, A. In-Vitro Subtype-Specific Modulation of HIV-1 Trans-Activator of Transcription (Tat) on RNAi Silencing Suppressor Activity and Cell Death. Viruses 2019, 11, 976. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- The World Health Organization. HIV/AIDS Treatment and Care. Available online: https://www.who.int/hiv/topics/treatment/en/ (accessed on 30 October 2019).
- Hertogs, K.; de Béthune, M.P.; Miller, V.; Ivens, T.; Schel, P.; Van Cauwenberge, A.; Van Den Eynde, C.; Van Gerwen, V.; Azijn, H.; Van Houtte, M.; et al. A rapid method for simultaneous detection of phenotypic resistance to inhibitors of protease and reverse transcriptase in recombinant human immunodeficiency virus type 1 isolates from patients treated with antiretroviral drugs. Antimicrob. Agents Chemother. 1998, 42, 269–276. [Google Scholar]
- Petropoulos, C.J.; Parkin, N.T.; Limoli, K.L.; Lie, Y.S.; Wrin, T.; Huang, W.; Tian, H.; Smith, D.; Winslow, G.A.; Capon, D.J.; et al. A Novel Phenotypic Drug Susceptibility Assay for Human Immunodeficiency Virus Type 1. Antimicrob. Agents Chemother. 2000, 44, 920–928. [Google Scholar] [CrossRef] [Green Version]
- Ramon, E.; Belanche-Muñoz, L.; Pérez-Enciso, M. HIV drug resistance prediction with weighted categorical kernel functions. BMC Bioinform. 2019, 20, 410. [Google Scholar] [CrossRef]
- Tarasova, O.; Biziukova, N.; Filimonov, D.; Poroikov, V. A Computational Approach for the Prediction of HIV Resistance Based on Amino Acid and Nucleotide Descriptors. Molecules 2018, 23, 2751. [Google Scholar] [CrossRef] [Green Version]
- Sheik Amamuddy, O.; Bishop, N.T.; Tastan Bishop, Ö. Improving fold resistance prediction of HIV-1 against protease and reverse transcriptase inhibitors using artificial neural networks. BMC Bioinform. 2017, 18, 369. [Google Scholar] [CrossRef] [Green Version]
- Singh, Y. Machine Learning to Improve the Effectiveness of ANRS in Predicting HIV Drug Resistance. Healthc. Inform. Res. 2017, 23, 271. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Riemenschneider, M.; Senge, R.; Neumann, U.; Hüllermeier, E.; Heider, D. Exploiting HIV-1 protease and reverse transcriptase cross-resistance information for improved drug resistance prediction by means of multi-label classification. BioData Min. 2016, 9, 10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heider, D.; Verheyen, J.; Hoffmann, D. Machine learning on normalized protein sequences. BMC Res. Notes 2011, 4, 94. [Google Scholar] [CrossRef] [Green Version]
- Van Westen, G.J.P.; Hendriks, A.; Wegner, J.K.; Ijzerman, A.P.; van Vlijmen, H.W.T.; Bender, A. Significantly Improved HIV Inhibitor Efficacy Prediction Employing Proteochemometric Models Generated from Antivirogram Data. PLoS Comput. Biol. 2013, 9, e1002899. [Google Scholar] [CrossRef] [PubMed]
- Revell, A.; Khabo, P.; Ledwaba, L.; Emery, S.; Wang, D.; Wood, R.; Morrow, C.; Tempelman, H.; Hamers, R.L.; Reiss, P.; et al. Computational models as predictors of HIV treatment outcomes for the Phidisa cohort in South Africa. South. Afr. J. HIV Med. 2016, 17. [Google Scholar] [CrossRef] [PubMed]
- Pironti, A.; Pfeifer, N.; Walter, H.; Jensen, B.-E.O.; Zazzi, M.; Gomes, P.; Kaiser, R.; Lengauer, T. Using drug exposure for predicting drug resistance—A data-driven genotypic interpretation tool. PLoS ONE 2017, 12, e0174992. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tarasova, O.A.; Filimonov, D.A.; Poroikov, V.V. Computational prediction of human immunodeficiency resistance to reverse transcriptase inhibitors. Biomed Khim 2017, 63, 457–460. [Google Scholar] [CrossRef] [Green Version]
- Tarasova, O.; Filimonov, D.; Poroikov, V. PASS based approach to predict HIV-1 reverse transcriptase resistance. J. Bioinform. Comput. Biol. 2017, 15, 1650040. [Google Scholar] [CrossRef]
- Rhee, S.-Y. Human immunodeficiency virus reverse transcriptase and protease sequence database. Nucleic Acids Res. 2003, 31, 298–303. [Google Scholar] [CrossRef] [Green Version]
- Filz, O.; Lagunin, A.; Filimonov, D.; Poroikov, V. Computer-aided prediction of QT-prolongation. SAR QSAR Environ. Res. 2008, 19, 81–90. [Google Scholar] [CrossRef]
- Filimonov, D.A.; Druzhilovskiy, D.S.; Lagunin, A.A.; Gloriozova, T.A.; Rudik, A.V.; Dmitriev, A.V.; Pogodin, P.V.; Poroikov, V.V. Computer-aided prediction of biological activity spectra for chemical compounds: opportunities and limitation. BMCRM 2018, 1, e00004. [Google Scholar] [CrossRef] [Green Version]
- Filz, O.A.; Lagunin, A.A.; Filimonov, D.A.; Poroikov, V.V. In silico fragment based drug design using a PASS approach. SAR QSAR Environ. Res. 2012, 23, 279–296. [Google Scholar] [CrossRef] [PubMed]
- Poroikov, V.; Filimonov, D.; Lagunin, A.; Gloriozova, T.; Zakharov, A. PASS: Identification of probable targets and mechanisms of toxicity. SAR QSAR Environ. Res. 2007, 18, 101–110. [Google Scholar] [CrossRef] [PubMed]
- Consolidated Guidelines on the Use of Antiretroviral Drugs for Treating and Preventing HIV Infection: Recommendations for a Public Health Approach; World Health Organization: Geneva, Switzerland, 2013; Available online: https://www.who.int/hiv/pub/arv/arv-2016/en/ (accessed on 30 October 2019).
- Eholié, S.P.; Badje, A.; Kouame, G.M.; N’takpe, J.-B.; Moh, R.; Danel, C.; Anglaret, X. Antiretroviral treatment regardless of CD4 count: the universal answer to a contextual question. AIDS Res. Ther. 2016, 13, 27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tran, M.; Wood, E.; Kerr, T.; Patterson, S.; Bangsberg, D.; Dong, H.; Guillemi, S.; Montaner, J.S.; Milloy, M.-J. Increases in CD4+ T-cell count at antiretroviral therapy initiation among HIV-positive illicit drug users during a treatment-as-prevention initiative in Canada. Antivir Ther. 2017, 22, 403–411. [Google Scholar] [CrossRef] [Green Version]
- Tarasova, O.A.; Urusova, A.F.; Filimonov, D.A.; Nicklaus, M.C.; Zakharov, A.V.; Poroikov, V.V. QSAR Modeling Using Large-Scale Databases: Case Study for HIV-1 Reverse Transcriptase Inhibitors. J. Chem. Inf. Model. 2015, 55, 1388–1399. [Google Scholar] [CrossRef]
- Tarasova, O.; Poroikov, V. HIV Resistance Prediction to Reverse Transcriptase Inhibitors: Focus on Open Data. Molecules 2018, 23, 956. [Google Scholar] [CrossRef] [Green Version]
- Torti, C.; Quiros-Roldan, E.; Keulen, W.; Scudeller, L.; Lo Caputo, S.; Boucher, C.; Castelli, F.; Mazzotta, F.; Pierotti, P.; Been-Tiktak, A.M.; et al. Comparison between Rules-Based Human Immunodeficiency Virus Type 1 Genotype Interpretations and Real or Virtual Phenotype: Concordance Analysis and Correlation with Clinical Outcome in Heavily Treated Patients. J. Infect. Dis. 2003, 188, 194–201. [Google Scholar] [CrossRef] [Green Version]
- Qari, S.H.; Respess, R.; Weinstock, H.; Beltrami, E.M.; Hertogs, K.; Larder, B.A.; Petropoulos, C.J.; Hellmann, N.; Heneine, W. Comparative Analysis of Two Commercial Phenotypic Assays for Drug Susceptibility Testing of Human Immunodeficiency Virus Type 1. J. Clin. Microbiol. 2002, 40, 31–35. [Google Scholar] [CrossRef] [Green Version]
- Chernoff, D.N. The significance of HIV viral load assay precision: a review of the package insert specifications of two commercial kits. J. Int. Assoc. Physicians AIDS Care (Chic) 2002, 1, 134–140. [Google Scholar] [CrossRef]
- Ronsard, L.; Sood, V.; Yousif, A.S.; Ramesh, J.; Shankar, V.; Das, J.; Sumi, N.; Rai, T.; Mohankumar, K.; Sridharan, S.; et al. Genetic Polymorphisms in the Open Reading Frame of the CCR5 gene From HIV-1 Seronegative and Seropositive Individuals From National Capital Regions of India. Sci. Rep. 2019, 9, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Gaff, J.; Octaviana, F.; Pillay, P.; Mbenda, H.G.N.; Ariyanto, I.A.; Gan, J.A.; Cherry, C.L.; Kamerman, P.; Laws, S.M.; Price, P. TNF-Block Genotypes Influence Susceptibility to HIV-Associated Sensory Neuropathy in Indonesians and South Africans. Int. J. Mol. Sci. 2020, 21, 380. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chawla, A.; Wang, C.; Patton, C.; Murray, M.; Punekar, Y.; de Ruiter, A.; Steinhart, C. A Review of Long-Term Toxicity of Antiretroviral Treatment Regimens and Implications for an Aging Population. Infect Dis. Ther. 2018, 7, 183–195. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cao, W.; Hsieh, E.; Li, T. Optimizing Treatment for Adults with HIV/AIDS in China: Successes over Two Decades and Remaining Challenges. Curr. HIV/AIDS Rep. 2020, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]




| Drug Set 1 | Sample Number | Period of Exposure 2 | AUC/ROC 3 | AUC/ROC20 3 | |
|---|---|---|---|---|---|
| LPV 4 | 2896 | 63 (57) | 0.94 | 0.91 | |
| NFV | 1334 | 68 (62) | 0.81 | 0.80 | |
| IDV | 984 | 74 (72) | 0.77 | 0.79 | |
| IDV, NFV, RTV, SQV | 425 | 160 (77) | 0.83 | 0.82 | |
| IDV, NFV | 396 | 160 (81) | 0.81 | 0.78 | |
| IDV, NFV, SQV | 238 | 127 (71) | 0.80 | 0.79 | |
| RTV, TPV | 132 | N/A 5 | 0.91 | 0.90 | |
| APV, IDV, NFV, RTV, SQV | 121 | 218 (74) | 0.86 | 0.84 | |
| ATV | 106 | 39 (22) | 0.81 | 0.80 | |
| IDV, LPV | 91 | 129 (101) | 0.81 | 0.80 | |
| APV | 66 | 41 (29) | 0.82 | 0.80 | |
| IDV, LPV, NFV, RTV, SQV | 70 | 272 (107) | 0.77 | 0.76 | |
| LPV, RTV | 35 | 182 (104) | 0.81 | 0.80 | |
| RTV, SQV | 35 | 91 (60) | 0.81 | 0.79 | |
| Other (average) | 3314 | N/A 5 | 0.79 | 0.76 | |
| Total | 10,243 | 0.81 | 0.80 | ||
| Drug Combinations | Sequence Number | AUC/ROC | AUC/ROC20 |
|---|---|---|---|
| No PR inhibitor, effective | 234 | 0.94 | 0.91 |
| NFV 1, effective | 147 | 0.90 | 0.86 |
| LPV 1, effective | 58 | 0.77 | 0.79 |
| RTV 1, APV 1, effective | 26 | 0.82 | 0.80 |
| IDV 1, effective | 28 | 0.91 | 0.90 |
| No PR inhibitor, failed | 42 | 0.94 | 0.92 |
| SQV 1, RTV 1, failed | 26 | 0.94 | 0.92 |
| NFV 1, failed | 23 | 0.90 | 0.89 |
| Other (rare combinations) | 268 | 0.79 | 0.76 |
| Average | 852 | 0.84 | 0.82 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tarasova, O.; Biziukova, N.; Kireev, D.; Lagunin, A.; Ivanov, S.; Filimonov, D.; Poroikov, V. A Computational Approach for the Prediction of Treatment History and the Effectiveness or Failure of Antiretroviral Therapy. Int. J. Mol. Sci. 2020, 21, 748. https://doi.org/10.3390/ijms21030748
Tarasova O, Biziukova N, Kireev D, Lagunin A, Ivanov S, Filimonov D, Poroikov V. A Computational Approach for the Prediction of Treatment History and the Effectiveness or Failure of Antiretroviral Therapy. International Journal of Molecular Sciences. 2020; 21(3):748. https://doi.org/10.3390/ijms21030748
Chicago/Turabian StyleTarasova, Olga, Nadezhda Biziukova, Dmitry Kireev, Alexey Lagunin, Sergey Ivanov, Dmitry Filimonov, and Vladimir Poroikov. 2020. "A Computational Approach for the Prediction of Treatment History and the Effectiveness or Failure of Antiretroviral Therapy" International Journal of Molecular Sciences 21, no. 3: 748. https://doi.org/10.3390/ijms21030748