IMM-H004 Protects against Cerebral Ischemia Injury and Cardiopulmonary Complications via CKLF1 Mediated Inflammation Pathway in Adult and Aged Rats
Abstract
:1. Introduction
2. Results
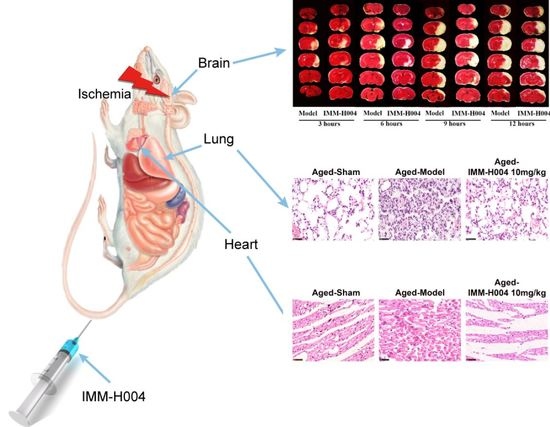
2.1. Effects of IMM-H004 on Permanent Focal Cerebral Ischemia-Induced Brain Injury in Adult Rats
2.2. Effects of IMM-H004 on Permanent Focal Cerebral Ischemia Induced Brain Injury in Aged Rats
2.3. IMM-H004 Inhibits Brain Inflammation after Permanent Focal Cerebral Ischemia in Aged Rats
2.4. Effects of IMM-H004 on Cardiopulmonary Complications in Aged Rats
2.5. IMM-H004 Suppresses Inflammation in Heart and Lung Post-Stroke of Aged Rats
2.6. IMM-H004 Exerts Protective Effects in Ischemic Brain through CKLF1 Mediated Inflammatory Pathway
2.7. IMM-H004 Protects against Ischemic Stroke Induced Cardiopulmonary Complications via CKLF1
3. Discussion
4. Materials and Methods
4.1. Experimental Animals
4.2. Materials
4.3. Rat pMCAO Model and Drug Administration
4.4. TTC Staining and Behavior Assessment
4.5. Magnetic Resonance Imaging (MRI)
4.6. ELISA Analysis
4.7. Nissl Staining
4.8. Histo-Pathological Examination
4.9. Cardiac Function Detection
4.10. Pulmonary Function Detection
4.11. Immunohistological Staining
4.12. Immunofluorescence Staining
4.13. qPCR
4.14. Western Blotting
4.15. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| CKLF1 | Chemokine-like factor 1 |
| CCR4 | C-C chemokine receptor type 4 |
| TTC | 2,3,5-triphenyltetrazolium-chloride |
| MRI | Magnetic resonance imaging |
| ELISA | Enzyme-linked immunosorbent assay |
| qPCR | Quantitative real-time PCR |
| tPA | Tissue plasminogen activator |
| FDA | Food and Drug Administration |
| MI | Myocardial infarction |
| PE | Pulmonary embolism |
| tMCAO | Transient middle cerebral artery occlusion |
| pMCAO | Permanent middle cerebral artery occlusion |
| ICA | Internal carotid artery |
| ECA | External carotid artery |
| CCA | Common carotid artery |
| PBS | Phosphate-buffered saline |
| DWI | Diffusion weighted imaging |
| IL-1β | Interleukin 1β |
| TNF-α | Tumor necrosis factor α |
| LDH | Lactate dehydrogenase |
| BCA | Bicinchoninic acid |
| HE | Hematoxylin-eosin |
| LVSP | Left ventricular systolic pressure |
| LVDP | Left ventricular developed pressure |
| +dp/dtmax | The maximal ventricular pressure rise ratio during systolic period |
| −dp/dtmax | The maximal ventricular pressure decrease ratio during diastolic period |
| VE | Minute ventilation |
| FEV1 | Forced expiratory volume in the first second |
| BSA | Bovine serum albumin |
| DBA | 3,3-diaminobenzidin |
| PVDF | Polyvinylidene difluoride |
| ECL | Enhanced chemiluminescence |
| SD | Standard deviation. |
References
- Feigin, V.L.; Forouzanfar, M.H.; Krishnamurthi, R.; Mensah, G.A.; Connor, M.; Bennett, D.A.; Moran, A.E.; Sacco, R.L.; Anderson, L.; Truelsen, T.; et al. Global and regional burden of stroke during 1990-2010: Findings from the Global Burden of Disease Study 2010. Lancet 2014, 383, 245–254. [Google Scholar] [CrossRef]
- Benjamin, E.J.; Virani, S.S.; Callaway, C.W.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Chiuve, S.E.; Cushman, M.; Delling, F.N.; Deo, R.; et al. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation 2018, 137, e67–e492. [Google Scholar] [CrossRef] [PubMed]
- Rojas, J.I.; Zurru, M.C.; Romano, M.; Patrucco, L.; Cristiano, E. Acute ischemic stroke and transient ischemic attack in the very old—Risk factor profile and stroke subtype between patients older than 80 years and patients aged less than 80 years. Eur. J. Neurol. 2007, 14, 895–899. [Google Scholar] [CrossRef] [PubMed]
- Leonardi-Bee, J.; Bath, P.M.; Phillips, S.J.; Sandercock, P.A. Blood pressure and clinical outcomes in the International Stroke Trial. Stroke 2002, 33, 1315–1320. [Google Scholar] [CrossRef] [PubMed]
- Williams, G.R.; Jiang, J.G.; Matchar, D.B.; Samsa, G.P. Incidence and occurrence of total (first-ever and recurrent) stroke. Stroke 1999, 30, 2523–2528. [Google Scholar] [CrossRef]
- Appelros, P.; Stegmayr, B.; Terent, A. Sex differences in stroke epidemiology: A systematic review. Stroke 2009, 40, 1082–1090. [Google Scholar] [CrossRef] [PubMed]
- Morris, D.C. Thrombolysis 3 to 4.5 Hours after Acute Ischemic Stroke. N. Engl. J. Med. 2008, 359, 2839–2841. [Google Scholar]
- Sun, Y.Y.; Morozov, Y.M.; Yang, D.; Li, Y.; Dunn, R.S.; Rakic, P.; Chan, P.H.; Abe, K.; Lindquist, D.M.; Kuan, C.Y. Synergy of combined tPA-edaravone therapy in experimental thrombotic stroke. PLoS ONE 2014, 9, e98807. [Google Scholar] [CrossRef]
- Won, S.; Lee, J.K.; Stein, D.G. Recombinant tissue plasminogen activator promotes, and progesterone attenuates, microglia/macrophage M1 polarization and recruitment of microglia after MCAO stroke in rats. Brain Behav. Immun. 2015, 49, 267–279. [Google Scholar] [CrossRef] [PubMed]
- Johnston, K.C.; Li, J.Y.; Lyden, P.D.; Hanson, S.K.; Feasby, T.E.; Adams, R.J.; Faught, R.E., Jr.; Haley, E.C., Jr. Medical and neurological complications of ischemic stroke: Experience from the RANTTAS trial. RANTTAS Investigators. Stroke 1998, 29, 447–453. [Google Scholar] [CrossRef]
- Hong, K.S.; Kang, D.W.; Koo, J.S.; Yu, K.H.; Han, M.K.; Cho, Y.J.; Park, J.M.; Bae, H.J.; Lee, B.C. Impact of neurological and medical complications on 3-month outcomes in acute ischaemic stroke. Eur. J. Neurol. 2008, 15, 1324–1331. [Google Scholar] [CrossRef] [PubMed]
- Viitanen, M.; Winblad, B.; Asplund, K. Autopsy-verified causes of death after stroke. Acta Med. Scand. 1987, 222, 401–408. [Google Scholar] [CrossRef] [PubMed]
- Balami, J.S.; Chen, R.L.; Grunwald, I.Q.; Buchan, A.M. Neurological complications of acute ischaemic stroke. Lancet Neurol. 2011, 10, 357–371. [Google Scholar] [CrossRef]
- Kumar, S.; Selim, M.H.; Caplan, L.R. Medical complications after stroke. Lancet Neurol. 2010, 9, 105–118. [Google Scholar] [CrossRef]
- Vernino, S.; Brown, R.D., Jr.; Sejvar, J.J.; Sicks, J.D.; Petty, G.W.; O’Fallon, W.M. Cause-specific mortality after first cerebral infarction: A population-based study. Stroke 2003, 34, 1828–1832. [Google Scholar] [CrossRef] [PubMed]
- Bronnum-Hansen, H.; Davidsen, M.; Thorvaldsen, P. Long-term survival and causes of death after stroke. Stroke 2001, 32, 2131–2136. [Google Scholar] [CrossRef] [PubMed]
- Hardie, K.; Hankey, G.J.; Jamrozik, K.; Broadhurst, R.J.; Anderson, C. Ten-year survival after first-ever stroke in the perth community stroke study. Stroke 2003, 34, 1842–1846. [Google Scholar] [CrossRef] [PubMed]
- Koennecke, H.C.; Belz, W.; Berfelde, D.; Endres, M.; Fitzek, S.; Hamilton, F.; Kreitsch, P.; Mackert, B.M.; Nabavi, D.G.; Nolte, C.H.; et al. Factors influencing in-hospital mortality and morbidity in patients treated on a stroke unit. Neurology 2011, 77, 965–972. [Google Scholar] [CrossRef] [PubMed]
- Iadecola, C.; Anrather, J. The immunology of stroke: From mechanisms to translation. Nat. Med. 2011, 17, 796–808. [Google Scholar] [CrossRef]
- Chamorro, A.; Hallenbeck, J. The harms and benefits of inflammatory and immune responses in vascular disease. Stroke 2006, 37, 291–293. [Google Scholar] [CrossRef]
- Offner, H.; Vandenbark, A.A.; Hurn, P.D. Effect of experimental stroke on peripheral immunity: CNS ischemia induces profound immunosuppression. Neuroscience 2009, 158, 1098–1111. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Jin, W.N.; Liu, Y.; Shi, K.; Sun, H.; Zhang, F.; Zhang, C.; Gonzales, R.J.; Sheth, K.N.; La Cava, A.; et al. Brain Ischemia Suppresses Immunity in the Periphery and Brain via Different Neurogenic Innervations. Immunity 2017, 46, 474–487. [Google Scholar] [CrossRef] [PubMed]
- Katzan, I.L.; Cebul, R.D.; Husak, S.H.; Dawson, N.V.; Baker, D.W. The effect of pneumonia on mortality among patients hospitalized for acute stroke. Neurology 2003, 60, 620–625. [Google Scholar] [CrossRef] [PubMed]
- Yang, G.Y.; Chen, X.; Sun, Y.C.; Ma, C.L.; Qian, G. Chemokine-like factor 1 (CLFK1) is over-expressed in patients with atopic dermatitis. Int. J. Biol. Sci. 2013, 9, 759–765. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Guo, C.; Zhang, Y.; Qi, H.; Sun, Q.; Xu, E.; Zhang, Y.; Ma, D.; Wang, Y. Alleviation of murine allergic rhinitis by C19, a C-terminal peptide of chemokine-like factor 1 (CKLF1). Int. Immunopharmacol. 2011, 11, 2188–2193. [Google Scholar] [CrossRef] [PubMed]
- Tan, Y.X.; Yang, T.; Chen, Q.L.; Ye, F.; Jiang, M.; Li, S.Y.; Ding, J.; Song, Q.S.; Li, X.T.; Tang, Y.; et al. Outcome and significance of pulmonary pathological changes induced by a single intramuscular injection of chemokine-like factor 1 in mice. Zhonghua Yi Xue Za Zhi. 2009, 89, 2408–2411. [Google Scholar]
- Li, G.; Wang, D.; Sun, M.; Li, G.; Hu, J.; Zhang, Y.; Yuan, Y.; Ji, H.; Chen, N.; Liu, G. Discovery and optimization of novel 3-piperazinylcoumarin antagonist of chemokine-like factor 1 with oral antiasthma activity in mice. J. Med. Chem. 2010, 53, 1741–1754. [Google Scholar] [CrossRef] [PubMed]
- Kong, L.L.; Hu, J.F.; Zhang, W.; Yuan, Y.H.; Ma, K.L.; Han, N.; Chen, N.H. Expression of chemokine-like factor 1 after focal cerebral ischemia in the rat. Neurosci. Lett. 2011, 505, 14–18. [Google Scholar] [CrossRef] [PubMed]
- Kong, L.L.; Hu, J.F.; Zhang, W.; Yuan, Y.H.; Han, N.; Chen, N.H. C19, a C-terminal peptide of chemokine-like factor 1, protects the brain against focal brain ischemia in rats. Neurosci. Lett. 2012, 508, 13–16. [Google Scholar] [CrossRef] [PubMed]
- Kong, L.L.; Wang, Z.Y.; Hu, J.F.; Yuan, Y.H.; Han, N.; Li, H.; Chen, N.H. Inhibition of chemokine-like factor 1 protects against focal cerebral ischemia through the promotion of energy metabolism and anti-apoptotic effect. Neurochem. Int. 2014, 76, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Santos Samary, C.; Pelosi, P.; Leme Silva, P.; Rieken Macedo Rocco, P. Immunomodulation after ischemic stroke: Potential mechanisms and implications for therapy. Crit. Care 2016, 20, 391. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, H.; Tajiri, N.; Vasconcellos, J.; Kaneko, Y.; Mimura, O.; Dezawa, M.; Borlongan, C.V. Ischemic stroke brain sends indirect cell death signals to the heart. Stroke 2013, 44, 3175–3182. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Y.; Zhang, Y.; Han, W.; Li, D.; Tian, L.; Yin, C.; Ma, D. Two C-terminal peptides of human CKLF1 interact with the chemokine receptor CCR4. Int. J. Biochem. Cell Biol. 2008, 40, 909–919. [Google Scholar] [CrossRef] [PubMed]
- Sun, M.; Hu, J.; Song, X.; Wu, D.; Kong, L.; Sun, Y.; Wang, D.; Wang, Y.; Chen, N.; Liu, G. Coumarin derivatives protect against ischemic brain injury in rats. Eur. J. Med. Chem. 2013, 67, 39–53. [Google Scholar] [CrossRef] [PubMed]
- Zuo, W.; Zhang, W.; Han, N.; Chen, N.H. Compound IMM-H004, a novel coumarin derivative, protects against CA1 cell loss and spatial learning impairments resulting from transient global ischemia. CNS Neurosci. Ther. 2015, 21, 280–288. [Google Scholar] [CrossRef] [PubMed]
- Niu, F.; Song, X.Y.; Hu, J.F.; Zuo, W.; Kong, L.L.; Wang, X.F.; Han, N.; Chen, N.H. IMM-H004, A New Coumarin Derivative, Improved Focal Cerebral Ischemia via Blood-Brain Barrier Protection in Rats. J. Stroke Cerebrovasc. Dis. 2017, 26, 2065–2073. [Google Scholar] [CrossRef] [PubMed]
- Yang, P.-F.; Song, X.-Y.; Zeng, T.; Ai, Q.-D.; Liu, D.-D.; Zuo, W.; Zhang, S.; Xia, C.-Y.; He, X.; Chen, N.-H. IMM-H004, a coumarin derivative, attenuated brain ischemia/reperfusion injuries and subsequent inflammation in spontaneously hypertensive rats through inhibition of VCAM-1. RSC Adv. 2017, 7, 27480–27495. [Google Scholar] [CrossRef] [Green Version]
- Zuo, W.; Chen, J.; Zhang, S.; Tang, J.; Liu, H.; Zhang, D.; Chen, N. IMM-H004 prevents toxicity induced by delayed treatment of tPA in a rat model of focal cerebral ischemia involving PKA-and PI3K-dependent Akt activation. Eur. J. Neurosci. 2014, 39, 2107–2118. [Google Scholar] [CrossRef] [PubMed]
- Zhang, G.; Zhang, R.; Wu, H.; Wang, H.; Zhang, W.; Zhang, L.; Sun, H.; Li, Y.; Bu, N.; Du, Y.; et al. Recanalization of occluded large arteries with broadened therapeutic window for acute cerebral infarction. Clin. Neurol. Neurosurg. 2013, 115, 1009–1015. [Google Scholar] [CrossRef] [PubMed]
- Jung, S.; Gralla, J.; Fischer, U.; Mono, M.L.; Weck, A.; Ludi, R.; Heldner, M.R.; Findling, O.; El-Koussy, M.; Brekenfeld, C.; et al. Safety of endovascular treatment beyond the 6-h time window in 205 patients. Eur. J. Neurol. 2013, 20, 865–871. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Cui, X.; Li, J.; Zhang, C.; Zhang, J.; Liu, M. Edaravone for acute stroke: Meta-analyses of data from randomized controlled trials. Dev. Neurorehabil. 2015, 18, 330–335. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.Y.; Tang, Y.; Gao, L.Y.; Sun, W.X.; Hua, Y.; Yang, S.B.; Zhang, Z.P.; Liao, G.Y.; Zhou, Q.G.; Luo, C.X.; et al. The synergetic effect of edaravone and borneol in the rat model of ischemic stroke. Eur. J. Pharmacol. 2014, 740, 522–531. [Google Scholar] [CrossRef] [PubMed]
- Oguro, H.; Mitaki, S.; Takayoshi, H.; Abe, S.; Onoda, K.; Yamaguchi, S. Retrospective Analysis of Argatroban in 353 Patients with Acute Noncardioembolic Stroke. J. Stroke Cerebrovasc. Dis. 2018, 27, 2175–2181. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, K.; Tanaka, M.; Yuki, S.; Hirai, M.; Yamamoto, Y. How is edaravone effective against acute ischemic stroke and amyotrophic lateral sclerosis? J. Clin. Biochem. Nutr. 2018, 62, 20–38. [Google Scholar] [CrossRef]
- Jin, R.; Liu, L.; Zhang, S.; Nanda, A.; Li, G. Role of inflammation and its mediators in acute ischemic stroke. J. Cardiovasc. Transl. Res. 2013, 6, 834–851. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kong, L.L.; Wang, Z.Y.; Han, N.; Zhuang, X.M.; Wang, Z.Z.; Li, H.; Chen, N.H. Neutralization of chemokine-like factor 1, a novel C-C chemokine, protects against focal cerebral ischemia by inhibiting neutrophil infiltration via MAPK pathways in rats. J. Neuroinflamm. 2014, 11, 112. [Google Scholar] [CrossRef] [PubMed]
- Kong, L.L.; Wang, Z.Y.; Hu, J.F.; Yuan, Y.H.; Li, H.; Chen, N.H. Inhibition of chemokine-like factor 1 improves blood-brain barrier dysfunction in rats following focal cerebral ischemia. Neurosci. Lett. 2016, 627, 192–198. [Google Scholar] [CrossRef]
- Shim, R.; Wong, C.H. Ischemia, Immunosuppression and Infection—Tackling the Predicaments of Post-Stroke Complications. Int. J. Mol. Sci. 2016, 17, 64. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.D.; Chu, S.F.; Chen, C.; Yang, P.F.; Chen, N.H.; He, X. Research progress in stroke-induced immunodepression syndrome (SIDS) and stroke-associated pneumonia (SAP). Neurochem. Int. 2018, 114, 42–54. [Google Scholar] [CrossRef] [PubMed]
- Aslanyan, S.; Weir, C.J.; Diener, H.C.; Kaste, M.; Lees, K.R. Pneumonia and urinary tract infection after acute ischaemic stroke: A tertiary analysis of the GAIN International trial. Eur. J. Neurol. 2004, 11, 49–53. [Google Scholar] [CrossRef] [PubMed]
- Hilker, R.; Poetter, C.; Findeisen, N.; Sobesky, J.; Jacobs, A.; Neveling, M.; Heiss, W.D. Nosocomial pneumonia after acute stroke: Implications for neurological intensive care medicine. Stroke 2003, 34, 975–981. [Google Scholar] [CrossRef] [PubMed]
- Liesz, A.; Hagmann, S.; Zschoche, C.; Adamek, J.; Zhou, W.; Sun, L.; Hug, A.; Zorn, M.; Dalpke, A.; Nawroth, P.; et al. The spectrum of systemic immune alterations after murine focal ischemia: Immunodepression versus immunomodulation. Stroke 2009, 40, 2849–2858. [Google Scholar] [CrossRef]
- Prass, K.; Meisel, C.; Hoflich, C.; Braun, J.; Halle, E.; Wolf, T.; Ruscher, K.; Victorov, I.V.; Priller, J.; Dirnagl, U.; et al. Stroke-induced immunodeficiency promotes spontaneous bacterial infections and is mediated by sympathetic activation reversal by post-stroke T helper cell type 1-like immunostimulation. J. Exp. Med. 2003, 198, 725–736. [Google Scholar] [CrossRef]
- Williams, J.L.; Holman, D.W.; Klein, R.S. Chemokines in the balance: Maintenance of homeostasis and protection at CNS barriers. Front. Cell. Neurosci. 2014, 8, 154. [Google Scholar] [CrossRef] [PubMed]
- Mukaida, N.; Matsumoto, T.; Yokoi, K.; Harada, A.; Matsushima, K. Inhibition of neutrophil-mediated acute inflammation injury by an antibody against interleukin-8 (IL-8). Inflamm. Res. 1998, 47 (Suppl. 3), S151–S157. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, T. The nuclear factor NF-kappaB pathway in inflammation. Cold Spring Harb. Perspect. Biol. 2009, 1, a001651. [Google Scholar] [CrossRef] [PubMed]
- Shih, R.H.; Wang, C.Y.; Yang, C.M. NF-kappaB Signaling Pathways in Neurological Inflammation: A Mini Review. Front. Mol. Neurosci. 2015, 8, 77. [Google Scholar] [CrossRef]
- Clemens, J.A.; Stephenson, D.T.; Dixon, E.P.; Smalstig, E.B.; Mincy, R.E.; Rash, K.S.; Little, S.P. Global cerebral ischemia activates nuclear factor-kappa B prior to evidence of DNA fragmentation. Brain Res. Mol. Brain Res. 1997, 48, 187–196. [Google Scholar] [CrossRef]
- Venna, V.R.; Weston, G.; Benashski, S.E.; Tarabishy, S.; Liu, F.; Li, J.; Conti, L.H.; McCullough, L.D. NF-kappaB contributes to the detrimental effects of social isolation after experimental stroke. Acta Neuropathol. 2012, 124, 425–438. [Google Scholar] [CrossRef]
- Chauhan, A.; Moser, H.; McCullough, L.D. Sex differences in ischaemic stroke: Potential cellular mechanisms. Clin. Sci. (Lond.) 2017, 131, 533–552. [Google Scholar] [CrossRef]
- Zuo, W.; Zhang, W.; Chen, N.H. Sexual dimorphism in cerebral ischemia injury. Eur. J. Pharmacol. 2013, 711, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Gibson, C.L. Cerebral ischemic stroke: Is gender important? J. Cereb. Blood Flow Metab. 2013, 33, 1355–1361. [Google Scholar] [CrossRef] [PubMed]
- Bekhbat, M.; Neigh, G.N. Sex differences in the neuro-immune consequences of stress: Focus on depression and anxiety. Brain Behav. Immun. 2018, 67, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Klein, S.L.; Flanagan, K.L. Sex differences in immune responses. Nat. Rev. Immunol. 2016, 16, 626–638. [Google Scholar] [CrossRef] [PubMed]
- Longa, E.Z.; Weinstein, P.R.; Carlson, S.; Cummins, R. Reversible middle cerebral artery occlusion without craniectomy in rats. Stroke 1989, 20, 84–91. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Song, X.-Y.; Xia, C.-Y.; Ai, Q.-D.; Chen, J.; Chu, S.-F.; He, W.-B.; Chen, N.-H. Effects of cerebral glucose levels in infarct areas on stroke injury mediated by blood glucose changes. RSC Adv. 2016, 6, 93815–93825. [Google Scholar] [CrossRef]
- Zhang, S.; Qi, Y.; Xu, Y.; Han, X.; Peng, J.; Liu, K.; Sun, C.K. Protective effect of flavonoid-rich extract from Rosa laevigata Michx on cerebral ischemia-reperfusion injury through suppression of apoptosis and inflammation. Neurochem. Int. 2013, 63, 522–532. [Google Scholar] [CrossRef] [PubMed]
- Zuo, W.; Yang, P.F.; Chen, J.; Zhang, Z.; Chen, N.H. Drp-1, a potential therapeutic target for brain ischaemic stroke. Br. J. Pharmacol. 2016, 173, 1665–1677. [Google Scholar] [CrossRef]
- Liu, S.; Ai, Q.; Feng, K.; Li, Y.; Liu, X. The cardioprotective effect of dihydromyricetin prevents ischemia-reperfusion-induced apoptosis in vivo and in vitro via the PI3K/Akt and HIF-1alpha signaling pathways. Apoptosis 2016, 21, 1366–1385. [Google Scholar] [CrossRef] [PubMed]















© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ai, Q.; Chen, C.; Chu, S.; Luo, Y.; Zhang, Z.; Zhang, S.; Yang, P.; Gao, Y.; Zhang, X.; Chen, N. IMM-H004 Protects against Cerebral Ischemia Injury and Cardiopulmonary Complications via CKLF1 Mediated Inflammation Pathway in Adult and Aged Rats. Int. J. Mol. Sci. 2019, 20, 1661. https://doi.org/10.3390/ijms20071661
Ai Q, Chen C, Chu S, Luo Y, Zhang Z, Zhang S, Yang P, Gao Y, Zhang X, Chen N. IMM-H004 Protects against Cerebral Ischemia Injury and Cardiopulmonary Complications via CKLF1 Mediated Inflammation Pathway in Adult and Aged Rats. International Journal of Molecular Sciences. 2019; 20(7):1661. https://doi.org/10.3390/ijms20071661
Chicago/Turabian StyleAi, Qidi, Chen Chen, Shifeng Chu, Yun Luo, Zhao Zhang, Shuai Zhang, Pengfei Yang, Yan Gao, Xiaoling Zhang, and Naihong Chen. 2019. "IMM-H004 Protects against Cerebral Ischemia Injury and Cardiopulmonary Complications via CKLF1 Mediated Inflammation Pathway in Adult and Aged Rats" International Journal of Molecular Sciences 20, no. 7: 1661. https://doi.org/10.3390/ijms20071661