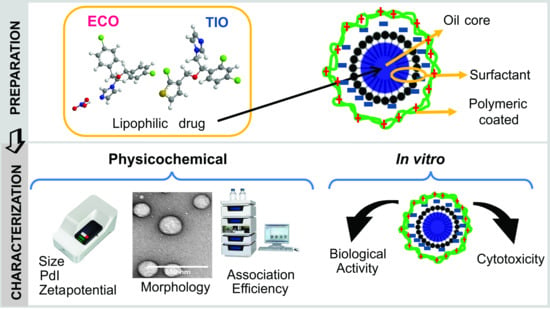
Design and Characterization of Chitosan Nanoformulations for the Delivery of Antifungal Agents
Abstract
1. Introduction
2. Results and Discussion
2.1. Physicochemical Properties of Tioconazol and Econazole Nanoformulations
2.2. Stability of NCs
2.3. Release Assays of TIO- and ECO-Loaded NCs
2.4. Storage Stability
2.5. In Vitro Cytotoxicity
2.6. Biological Activity against Candida Albicans
2.6.1. Antifungal Susceptibility Testing
2.6.2. Time-to-Kill
3. Materials and Methods
3.1. Chemicals
3.2. Nanoformulation Preparation
3.3. Reverse-Phase High-Performance Liquid Chromatography (RP-HPLC with UV Detection)
3.4. Association Efficiency
3.5. Physicochemical Characterization
3.6. Transmission Electron Microscopy
3.7. Colloidal Stability in Media
3.8. Storage Stability of NCs
3.9. In Vitro Release Assay
3.10. Cell Culture
3.11. Cell Viability
3.12. Biological Activity against Candida Albicans
3.12.1. Strains and Culture Conditions
3.12.2. Antifungal Susceptibility Testing
3.12.3. Time-to-Kill
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Rosenbach, A.; Dignard, D.; Pierce, J.V.; Whiteway, M.; Kumamoto, C.A. Adaptations of Candida albicans for Growth in the Mammalian Intestinal Tract. Eukaryot. Cell 2010, 9, 1075–1086. [Google Scholar] [CrossRef] [PubMed]
- Achkar, J.M.; Fries, B.C. Candida Infections of the Genitourinary Tract. Clin. Microbiol. Rev. 2010, 23, 253–273. [Google Scholar] [CrossRef] [PubMed]
- Heeres, J.; Van den Bossche, H. Antifungal Chemotherapy. In Annual Reports in Medicinal Chemistry; Academic Press: Cambridge, MA, USA, 1980; Volume 15, pp. 139–148. [Google Scholar]
- Spampinato, C.; Leonardi, D. Candida infections, causes, targets, and resistance mechanisms: traditional and alternative antifungal agents. Biomed Res. Int. 2013, 2013, 204237. [Google Scholar] [CrossRef] [PubMed]
- Zhang, A.Y.; Camp, W.L.; Elewski, B.E. Advances in Topical and Systemic Antifungals. Dermatol. Clin. 2007, 25, 165–183. [Google Scholar] [CrossRef] [PubMed]
- Firooz, A.; Nafisi, S.; Maibach, H.I. Novel drug delivery strategies for improving econazole antifungal action. Int. J. Pharm. 2015, 495, 599–607. [Google Scholar] [CrossRef] [PubMed]
- Passerini, N.; Gavini, E.; Albertini, B.; Rassu, G.; Di Sabatino, M.; Sanna, V.; Giunchedi, P.; Rodriguez, L. Evaluation of solid lipid microparticles produced by spray congealing for topical application of econazole nitrate. J. Pharm. Pharmacol. 2009, 61, 559–567. [Google Scholar] [CrossRef] [PubMed]
- Calvo, N.L.; Svetaz, L.A.; Alvarez, V.A.; Quiroga, A.D.; Lamas, M.C.; Leonardi, D. Chitosan-hydroxypropyl methylcellulose tioconazole films: A promising alternative dosage form for the treatment of vaginal candidiasis. Int. J. Pharm. 2019, 556, 181–191. [Google Scholar] [CrossRef]
- Dyas, A.; Delargy, H. Analytical Profiles of Drug Substances and Excipients; Elsevier Academic Press: New York, NY, USA, 1994; pp. 125–151. [Google Scholar]
- Cevher, E.; Açma, A.; Sinani, G.; Aksu, B.; Zloh, M.; Mülazımoğlu, L. Bioadhesive tablets containing cyclodextrin complex of itraconazole for the treatment of vaginal candidiasis. Int. J. Biol. Macromol. 2014, 69, 124–136. [Google Scholar] [CrossRef]
- Real, D.A.; Martinez, M.V.; Frattini, A.; Soazo, M.; Luque, A.G.; Biasoli, M.S.; Salomon, C.J.; Olivieri, A.C.; Leonardi, D. Design, Characterization, and In Vitro Evaluation of Antifungal Polymeric Films. AAPS PharmSciTech 2013, 14, 64–73. [Google Scholar] [CrossRef]
- Deshkar, S.S.; Palve, V.K. Formulation and development of thermosensitive cyclodextrin-based in situ gel of voriconazole for vaginal delivery. J. Drug Deliv. Sci. Technol. 2019, 49, 277–285. [Google Scholar] [CrossRef]
- Vergara, D.; Bellomo, C.; Zhang, X.; Vergaro, V.; Tinelli, A.; Lorusso, V.; Rinaldi, R.; Lvov, Y.M.; Leporatti, S.; Maffia, M. Lapatinib/Paclitaxel polyelectrolyte nanocapsules for overcoming multidrug resistance in ovarian cancer. Nanomed. Nanotechnol. Biol. Med. 2012, 8, 891–899. [Google Scholar] [CrossRef] [PubMed]
- Danhier, F.; Messaoudi, K.; Lemaire, L.; Benoit, J.-P.; Lagarce, F. Combined anti-Galectin-1 and anti-EGFR siRNA-loaded chitosan-lipid nanocapsules decrease temozolomide resistance in glioblastoma: In vivo evaluation. Int. J. Pharm. 2015, 481, 154–161. [Google Scholar] [CrossRef] [PubMed]
- Schultze, E.; Ourique, A.; Yurgel, V.C.; Begnini, K.R.; Thurow, H.; de Leon, P.M.M.; Campos, V.F.; Dellagostin, O.A.; Guterres, S.R.; Pohlmann, A.R.; et al. Encapsulation in lipid-core nanocapsules overcomes lung cancer cell resistance to tretinoin. Eur. J. Pharm. Biopharm. 2014, 87, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Schultze, E.; Buss, J.; Coradini, K.; Begnini, K.R.; Guterres, S.S.; Collares, T.; Beck, R.C.R.; Pohlmann, A.R.; Seixas, F.K. Tretinoin-loaded lipid-core nanocapsules overcome the triple-negative breast cancer cell resistance to tretinoin and show synergistic effect on cytotoxicity induced by doxorubicin and 5-fluororacil. Biomed. Pharmacother. 2017, 96, 404–409. [Google Scholar] [CrossRef] [PubMed]
- Cé, R.; Marchi, J.G.; Bergamo, V.Z.; Fuentefria, A.M.; Lavayen, V.; Guterres, S.S.; Pohlmann, A.R. Chitosan-coated dapsone-loaded lipid-core nanocapsules: Growth inhibition of clinical isolates, multidrug-resistant Staphylococcus aureus and Aspergillus ssp. Colloids Surfaces A Physicochem. Eng. Asp. 2016, 511, 153–161. [Google Scholar] [CrossRef]
- Kothamasu, P.; Kanumur, H.; Ravur, N.; Maddu, C.; Parasuramrajam, R.; Thangavel, S. Nanocapsules: the weapons for novel drug delivery systems. Bioimpacts 2012, 2, 71–81. [Google Scholar] [PubMed]
- Barratt, G.M. Therapeutic applications of colloidal drug carriers. Pharm. Sci. Technolo. Today 2000, 3, 163–171. [Google Scholar] [CrossRef]
- Sánchez-Moreno, P.; Ortega-Vinuesa, J.L.; Martín-Rodríguez, A.; Boulaiz, H.; Marchal-Corrales, J.A.; Peula-García, J.M. Characterization of Different Functionalized Lipidic Nanocapsules as Potential Drug Carriers. Int. J. Mol. Sci. 2012, 13, 2405–2424. [Google Scholar] [CrossRef] [PubMed]
- Calvo, P.; Remuñán-López, C.; Vila-Jato, J.L.; Alonso, M.J. Development of positively charged colloidal drug carriers: Chitosan-coated polyester nanocapsules and submicron-emulsions. Colloid Polym. Sci. 1997, 275, 46–53. [Google Scholar] [CrossRef]
- Prego, C.; Fabre, M.; Torres, D.; Alonso, M.J. Efficacy and Mechanism of Action of Chitosan Nanocapsules for Oral Peptide Delivery. Pharm. Res. 2006, 23, 549–556. [Google Scholar] [CrossRef]
- Prego, C.; Torres, D.; Alonso, M.J. Chitosan nanocapsules: a new carrier for nasal peptide delivery. J. Drug Deliv. Sci. Technol. 2006, 16, 331–337. [Google Scholar] [CrossRef]
- Prego, C.; Torres, D.; Alonso, M.J. Chitosan nanocapsules as carriers for oral peptide delivery: effect of chitosan molecular weight and type of salt on the in vitro behaviour and in vivo effectiveness. J. Nanosci. Nanotechnol. 2006, 6, 2921–2928. [Google Scholar] [CrossRef] [PubMed]
- Lozano, M.V.; Torrecilla, D.; Torres, D.; Vidal, A.; Domínguez, F.; Alonso, M.J. Highly Efficient System To Deliver Taxanes into Tumor Cells: Docetaxel-Loaded Chitosan Oligomer Colloidal Carriers. Biomacromolecules 2008, 9, 2186–2193. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, C.P.; Venturini, C.G.; Donida, B.; Poletto, F.S.; Guterres, S.S.; Pohlmann, A.R. An algorithm to determine the mechanism of drug distribution in lipid-core nanocapsule formulations. Soft Matter 2013, 9, 1141–1150. [Google Scholar] [CrossRef]
- Pavinatto, F.J.; Caseli, L.; Oliveira, O.N. Chitosan in Nanostructured Thin Films. Biomacromolecules 2010, 11, 1897–1908. [Google Scholar] [CrossRef] [PubMed]
- Bernkop-Schnürch, A.; Dünnhaupt, S. Chitosan-based drug delivery systems. Eur. J. Pharm. Biopharm. 2012, 81, 463–469. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Vimal, A.; Kumar, A. Why Chitosan? From properties to perspective of mucosal drug delivery. Int. J. Biol. Macromol. 2016, 91, 615–622. [Google Scholar] [CrossRef] [PubMed]
- Vicente, S.; Diaz-Freitas, B.; Peleteiro, M.; Sanchez, A.; Pascual, D.W.; Gonzalez-Fernandez, A.; Alonso, M.J. A Polymer/Oil Based Nanovaccine as a Single-Dose Immunization Approach. PLoS ONE 2013, 8, e62500. [Google Scholar] [CrossRef] [PubMed]
- Iglesias, N.; Galbis, E.; Díaz-Blanco, M.; Lucas, R.; Benito, E.; de-Paz, M.-V.; Iglesias, N.; Galbis, E.; Díaz-Blanco, M.J.; Lucas, R.; et al. Nanostructured Chitosan-Based Biomaterials for Sustained and Colon-Specific Resveratrol Release. Int. J. Mol. Sci. 2019, 20, 398. [Google Scholar] [CrossRef]
- Ali, A.; Ahmed, S. A review on chitosan and its nanocomposites in drug delivery. Int. J. Biol. Macromol. 2018, 109, 273–286. [Google Scholar] [CrossRef]
- Alonso-Sande, M.; Cuña, M.; Remuñán-López, C.; Teijeiro-Osorio, D.; Alonso-Lebrero, J.L.; Alonso, M.J. Formation of New Glucomannan−Chitosan Nanoparticles and Study of Their Ability To Associate and Deliver Proteins. Macromolecules 2006, 39, 4152–4158. [Google Scholar] [CrossRef]
- Langenbucher, F. Linearization of dissolution rate curves by the Weibull distribution. J. Pharm. Pharmacol. 1972, 24, 979–981. [Google Scholar] [CrossRef] [PubMed]
- Goldsmith, J.A.; Randall, N.; Ross, S.D. On methods of expressing dissolution rate data. J. Pharm. Pharmacol. 1978, 30, 347–349. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulou, V.; Kosmidis, K.; Vlachou, M.; Macheras, P. On the use of the Weibull function for the discernment of drug release mechanisms. Int. J. Pharm. 2006, 309, 44–50. [Google Scholar] [CrossRef] [PubMed]
- Kosmidis, K.; Argyrakis, P.; Macheras, P. Fractal kinetics in drug release from finite fractal matrices. J. Chem. Phys. 2003, 119, 6373–6377. [Google Scholar] [CrossRef]
- Burnham, K.P.; Anderson, D.R. Model Selection and Multimodel Inference; Springer New York: New York, NY, USA, 2002. [Google Scholar]
- Brum, A.A.S.; dos Santos, P.P.; da Silva, M.M.; Paese, K.; Guterres, S.S.; Costa, T.M.H.; Pohlmann, A.R.; Jablonski, A.; Flôres, S.H.; de Rios, A.O. Lutein-loaded lipid-core nanocapsules: Physicochemical characterization and stability evaluation. Colloids Surfaces A Physicochem. Eng. Asp. 2017, 522, 477–484. [Google Scholar] [CrossRef]
- Real, D.; Hoffmann, S.; Leonardi, D.; Salomon, C.; Goycoolea, F.M. Chitosan-based nanodelivery systems applied to the development of novel triclabendazole formulations. PLoS ONE 2018, 13, e0207625. [Google Scholar] [CrossRef] [PubMed]
- Pardeike, J.; Müller, R.H. Nanosuspensions: A promising formulation for the new phospholipase A2 inhibitor PX-18. Int. J. Pharm. 2010, 391, 322–329. [Google Scholar] [CrossRef] [PubMed]
- Emulsion Stability and Testing. Available online: https://www.particlesciences.com/news/technical-briefs/2011/emulsion-stability-and-testing.html (accessed on 18 July 2019).
- Hu, X.; Zhang, Y.; Zhao, X.; Hwang, H.-M. Biodegradation of benzo[a]pyrene with immobilized laccase: Genotoxicity of the products in HaCat and A3 cells. Environ. Mol. Mutagen. 2007, 48, 106–113. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, R.F.; Motta, M.H.; Härter, A.P.G.; Flores, F.C.; Beck, R.C.R.; Schaffazick, S.R.; de Bona da Silva, C. Spray-dried powders improve the controlled release of antifungal tioconazole-loaded polymeric nanocapsules compared to with lyophilized products. Mater. Sci. Eng. C 2016, 59, 875–884. [Google Scholar] [CrossRef]
- Alam, M.A.; Ahmad, F.J.; Khan, Z.I.; Khar, R.K.; Ali, M. Development and evaluation of acid-buffering bioadhesive vaginal tablet for mixed vaginal infections. AAPS PharmSciTech 2007, 8, 229. [Google Scholar] [CrossRef] [PubMed]
- Owen, D.H.; Katz, D.F. A vaginal fluid simulant. Contraception 1999, 59, 91–95. [Google Scholar] [CrossRef]
- Zhang, Y.; Huo, M.; Zhou, J.; Zou, A.; Li, W.; Yao, C.; Xie, S. DDSolver: An Add-In Program for Modeling and Comparison of Drug Dissolution Profiles. AAPS J. 2010, 12, 263–271. [Google Scholar] [CrossRef] [PubMed]
- CLSI. Reference Method for Broth Dilution Antifungal Susceptibility Testing of Yeasts; Approved Standard-Third Edition; CLSI: Wayne, PA, USA, 2008. [Google Scholar]
- Rodero, L.; Córdoba, S. Método de dilución en medio líquido. In Manual de Técnicas in vitro para la detección de compuestos antifúngicos; Zacchino, S., Gupta, M., Eds.; Corpus: Rosario, Argentina, 2007; pp. 85–97. [Google Scholar]
- Machado, A.; Cunha-Reis, C.; Araújo, F.; Nunes, R.; Seabra, V.; Ferreira, D.; das Neves, J.; Sarmento, B. Development and in vivo safety assessment of tenofovir-loaded nanoparticles-in-film as a novel vaginal microbicide delivery system. Acta Biomater. 2016, 44, 332–340. [Google Scholar] [CrossRef] [PubMed]
- Contri, R.V.; Soares, R.M.D.; Pohlmann, A.R.; Guterres, S.S. Structural analysis of chitosan hydrogels containing polymeric nanocapsules. Mater. Sci. Eng. C 2014. [Google Scholar] [CrossRef] [PubMed]








| Sample | Nanoemulsions | Nanocapsules | ||||||
|---|---|---|---|---|---|---|---|---|
| Size (nm) | PdI a | ζ (mV) b | Size (nm) | PdI a | ζ (mV) | Drug AE (%) c | ||
| Unloaded | 139.0 ± 3.8 | 0.170 ± 0.028 | −42.0 ± 4.5 | 131.7 ± 0.5 | 0.103 ± 0.004 | +46.0 ± 0.7 | - | |
| ECO 2 mM | 1312 ± 131 | 0.763 ± 0.06 | +1.48 ± 1.6 | 127.1 ± 1.5 | 0.107 ± 0.017 | +33.0 ± 1.0 | 87.2 ± 6.1 | |
| TIO 5 mM | 2215 ± 1348 | 0.9 ± 0.173 | −5.19 ± 1.3 | 146.8 ± 0.8 | 0.079 ± 0.019 | +24.7 ± 1.1 | 99.0 ± 0.8 | |
| Formulation | Model | Parameters a | R2adj | AIC | MSC | |
|---|---|---|---|---|---|---|
| NC_TIO | Zero-order | K0 | 0.511 | 0.6047 | 54.7691 | 0.6292 |
| Higuchi | KH | 3.282 | 0.9247 | 38.1915 | 2.2870 | |
| First-order | K1 | 0.006 | 0.6418 | 53.7831 | 0.7278 | |
| Korsmeyer-Peppas | KKP | 4.230 | 0.9334 | 37.7848 | 2.3276 | |
| n | 0.421 | |||||
| Hixson-Crowell | KHC | 0.002 | 0.6295 | 54.1226 | 0.6939 | |
| Weibull | α | 17.652 | 0.9639 | 32.3242 | 2.8737 | |
| β | 0.368 | |||||
| T1 | 0.487 | |||||
| Formulation | Model | Parameters a | R2adj | AIC | MSC | |
|---|---|---|---|---|---|---|
| NC_ECO | Zero-order | K0 | 0.277 | 0.7961 | 35.7050 | 1.3082 |
| Higuchi | KH | 1.717 | 0.9853 | 9.3942 | 3.9393 | |
| First-order | K1 | 0.003 | 0.8126 | 34.8618 | 1.3925 | |
| Korsmeyer-Peppas | KKP | 1.681 | 0.9836 | 11.3412 | 3.7446 | |
| n | 0.506 | |||||
| Hixson-Crowell | KHC | 0.001 | 0.8072 | 35.1482 | 1.3639 | |
| Weibull | α | 53.377 | 0.9879 | 8.9542 | 3.9833 | |
| β | 0.493 | |||||
| T1 | 0.222 | |||||
| Sample | MIC (24 h) | MFC (24 h) | MFC (48 h) |
|---|---|---|---|
| TIO | 1.52 | 24.25 | 6.06 |
| NC_TIO | 1.52 | 48.50 | 3.03 |
| ECO | 3.03 | 24.25 | 3.03 |
| NC_ECO | 3.03 | 48.50 | 3.03 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Calvo, N.L.; Sreekumar, S.; Svetaz, L.A.; Lamas, M.C.; Moerschbacher, B.M.; Leonardi, D. Design and Characterization of Chitosan Nanoformulations for the Delivery of Antifungal Agents. Int. J. Mol. Sci. 2019, 20, 3686. https://doi.org/10.3390/ijms20153686
Calvo NL, Sreekumar S, Svetaz LA, Lamas MC, Moerschbacher BM, Leonardi D. Design and Characterization of Chitosan Nanoformulations for the Delivery of Antifungal Agents. International Journal of Molecular Sciences. 2019; 20(15):3686. https://doi.org/10.3390/ijms20153686
Chicago/Turabian StyleCalvo, Natalia L., Sruthi Sreekumar, Laura A. Svetaz, María C. Lamas, Bruno M. Moerschbacher, and Darío Leonardi. 2019. "Design and Characterization of Chitosan Nanoformulations for the Delivery of Antifungal Agents" International Journal of Molecular Sciences 20, no. 15: 3686. https://doi.org/10.3390/ijms20153686
APA StyleCalvo, N. L., Sreekumar, S., Svetaz, L. A., Lamas, M. C., Moerschbacher, B. M., & Leonardi, D. (2019). Design and Characterization of Chitosan Nanoformulations for the Delivery of Antifungal Agents. International Journal of Molecular Sciences, 20(15), 3686. https://doi.org/10.3390/ijms20153686