Usefulness of Plasma YKL-40 in Management of Community-Acquired Pneumonia Severity in Patients
Abstract
:1. Introduction
2. Results and Discussion
3. Experimental Section
3.1. Subjects and Diagnosis
3.2. Subjects and Blood Specimen Collection
3.3. Sample Size and Statistical Power
3.4. Measurement of White Blood Cells (WBC), Neutrophil Cells, and C-Reactive Protein (CRP) Concentrations
3.5. Measurement of Plasma YKL-40 Level by Enzyme-Linked Immunosorbent Assay
3.6. Statistical Analysis
4. Conclusions
| Clinical Variables | Controls (n = 60) Median (Range) | Pretreated (n = 61) Median (Range) | Posttreated (n = 61) Median (Range) | p Value UT/C b | p Value UT/T c |
|---|---|---|---|---|---|
| Age | 59.4 ± 1.5 | 59.5 ± 2.6 | - | p = 0.963 | - |
| Gender | - | - | - | - | - |
| Male | 36 (60%) | 37 (60.7%) | - | p = 0.941 | - |
| Female | 24 (40%) | 24 (39.3%) | - | - | - |
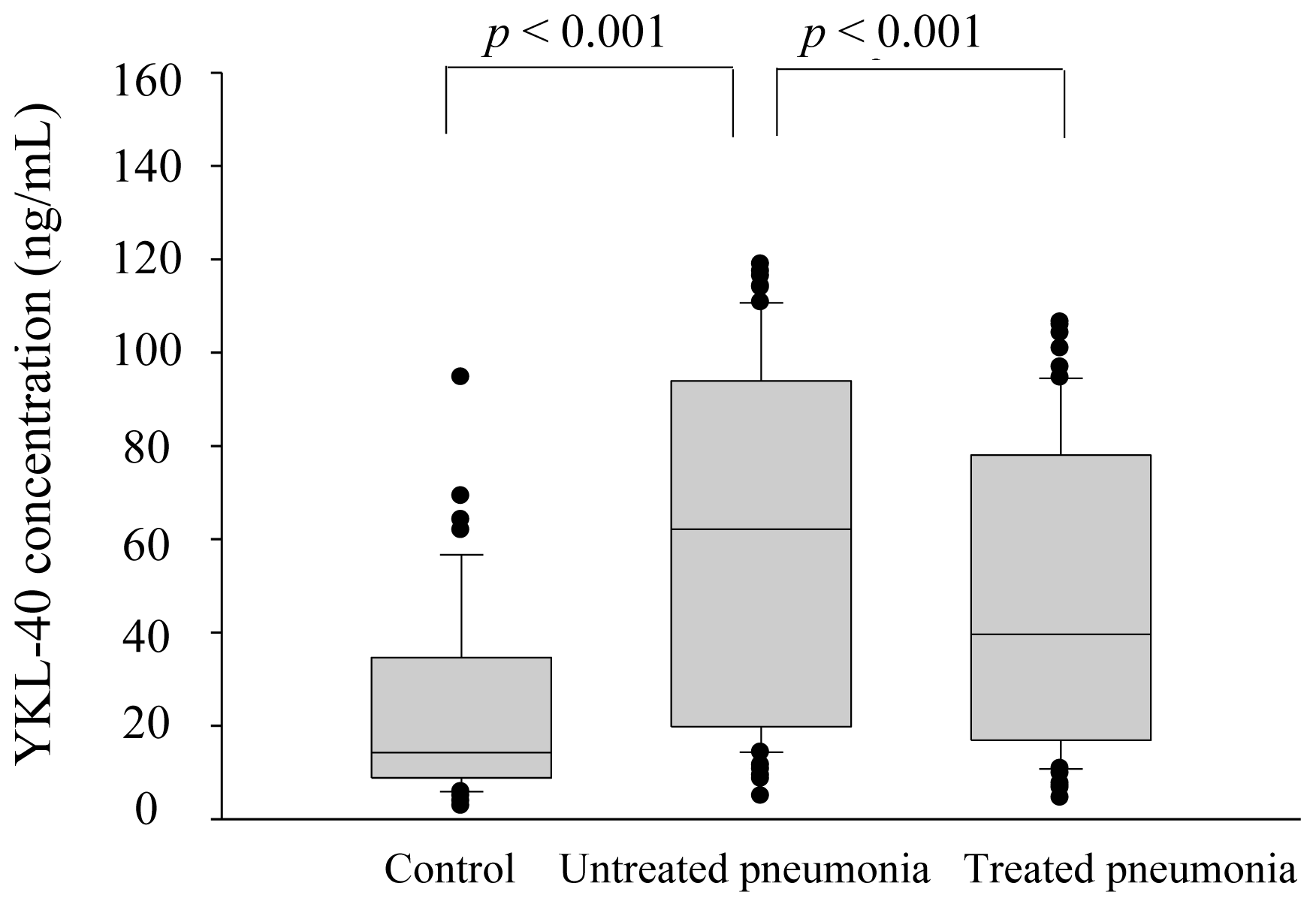
| YKL-40 (ng/mL) | 23.1 (2.7–94.6) | 62.1 (4.8–118.8) | 39.6 (4.5–106.4) | p < 0.001 | p < 0.001 |
| CRP (mg/dL) | 0.3 (0.1–1.7) | 8.6 (0.7–27.4) | 0.9 (0.3–11.3) | p < 0.001 | p < 0.001 |
| WBC (/mm3) | 5860 (3110–10190) | 10890 (3560–32480) | 8450 (3460–22340) | p < 0.001 | p < 0.001 |
| Neutrophils (/mm3) | 3530 (1738–6046) | 8673 (1032–29686) | 5484 (1518–21155) | p < 0.001 | p < 0.001 |
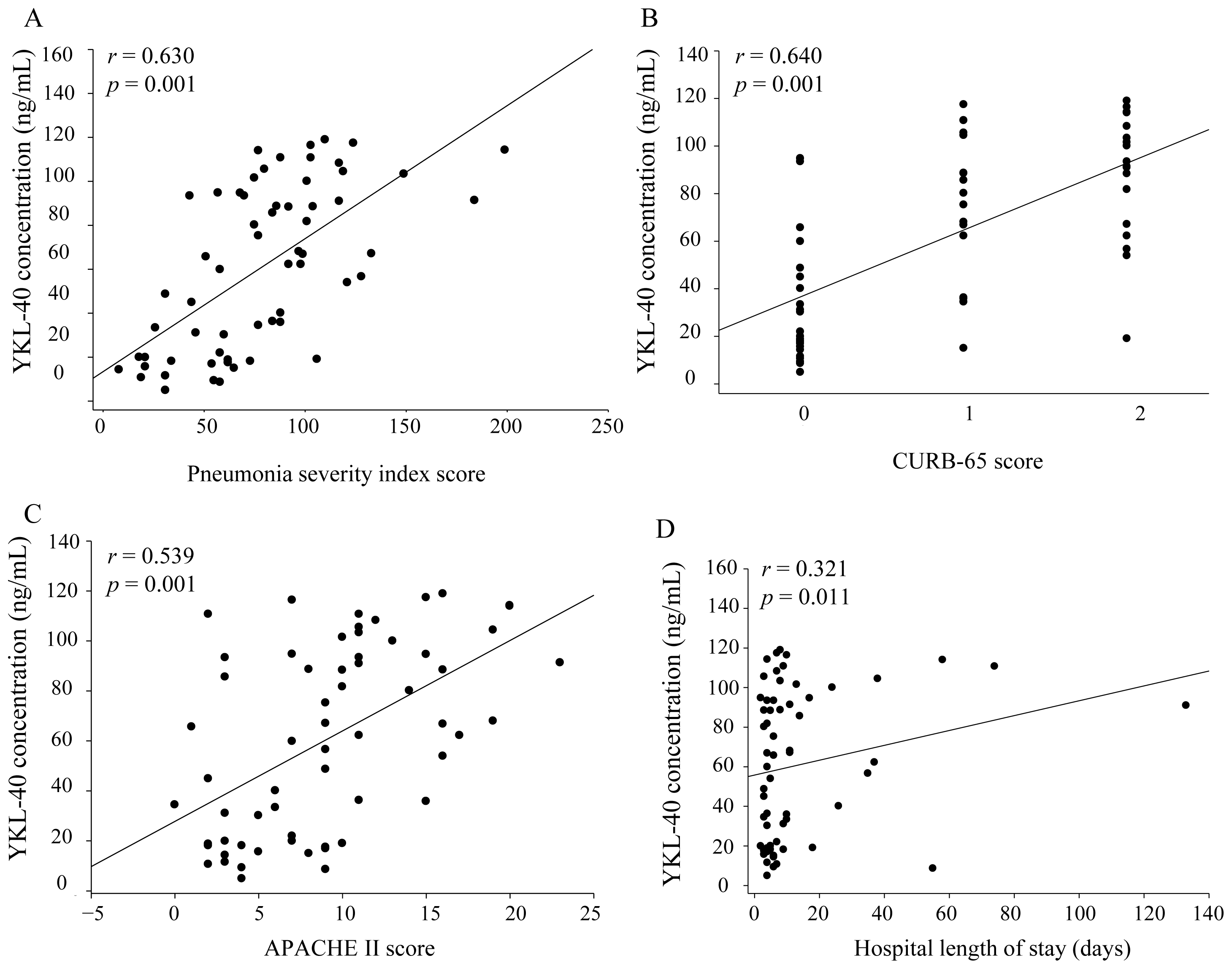
| PSI score | - | 79.0 ±5.9 e | - | - | - |
| CURB-65 score d | - | 0.9 ± 0.1 e | - | - | - |
| APACHE II score | - | 9.2 ± 0.7 e | - | - | - |
| Hospital length of stay (Days) | - | 13.9 ± 2.7 | - | - | - |
Conflicts of Interest
References
- Chiang, T.Y.; Shyu, L.Y.; Tsao, T.C.; Chien, M.H.; Tsao, S.M.; Lee, Y.T.; Yang, S.F. Elevated plasma matrix metalloproteinase-9 protein and its gene polymorphism in patients with community-acquired pneumonia. Clin. Chem. Lab. Med 2011, 50, 449–454. [Google Scholar]
- Lee, Y.T.; Chen, S.C.; Shyu, L.Y.; Lee, M.C.; Wu, T.C.; Tsao, S.M.; Yang, S.F. Significant elevation of plasma cathepsin B and cystatin C in patients with community-acquired pneumonia. Clin. Chim. Acta 2012, 413, 630–635. [Google Scholar]
- Houck, P.M.; Bratzler, D.W.; Nsa, W.; Ma, A.; Bartlett, J.G. Timing of antibiotic administration and outcomes for Medicare patients hospitalized with community-acquired pneumonia. Arch. Intern. Med 2004, 164, 637–644. [Google Scholar]
- Lee, S.H.; Lin, C.Y.; Wang, P.H.; Han, C.P.; Yang, S.F.; Chang, J.T.; Lee, M.C.; Lin, L.Y.; Lee, M.S. Significant association of elevated concentration of plasma YKL-40 with disease severity in patients with pelvic inflammatory disease. J. Clin. Lab. Anal 2012, 26, 136–142. [Google Scholar]
- Zheng, J.L.; Lu, L.; Hu, J.; Zhang, R.Y.; Zhang, Q.; Chen, Q.J.; Shen, W.F. Genetic polymorphisms in chitinase 3-like 1 (CHI3L1) are associated with circulating YKL-40 levels, but not with angiographic coronary artery disease in a Chinese population. Cytokine 2011, 54, 51–55. [Google Scholar]
- Nordenbaek, C.; Johansen, J.S.; Junker, P.; Borregaard, N.; Sørensen, O.; Price, P.A. YKL-40, a matrix protein of specific granules in neutrophils, is elevated in serum of patients with community-acquired pneumonia requiring hospitalization. J. Infect. Dis 1999, 180, 1722–1726. [Google Scholar]
- Badariotti, F.; Kypriotou, M.; Lelong, C.; Dubos, M.P.; Renard, E.; Galera, P.; Favrel, P. The phylogenetically conserved molluscan chitinase-like protein 1 (Cg-Clp1), homologue of human HC-gp39, stimulates proliferation and regulates synthesis of extracellular matrix components of mammalian chondrocytes. J. Biol. Chem 2006, 281, 29583–29596. [Google Scholar]
- Volck, B.; Price, P.A.; Johansen, J.S.; Sørensen, O.; Benfield, T.L.; Nielsen, H.J.; Calafat, J.; Borregaard, N. YKL-40, a mammalian member of the chitinase family, is a matrix protein of specific granules in human neutrophils. Proc. Assoc. Am. Physicians 1998, 110, 351–360. [Google Scholar]
- Malinda, K.M.; Ponce, L.; Kleinman, H.K.; Shackelton, L.M.; Millis, A.J. Gp38k, a protein synthesized by vascular smooth muscle cells, stimulates directional migration of human umbilical vein endothelial cells. Exp. Cell. Res 1999, 250, 168–173. [Google Scholar]
- Hakala, B.E.; White, C.; Recklies, A.D. Human cartilage gp-39, a major secretory product of articular chondrocytes and synovial cells, is a mammalian member of a chitinase protein family. J. Biol. Chem 1993, 268, 25803–25810. [Google Scholar]
- Lee, J.H.; Kim, S.S.; Kim, I.J.; Song, S.H.; Kim, Y.K.; In Kim, J.; Jeon, Y.K.; Kim, B.H.; Kwak, I.S. Clinical implication of plasma and urine YKL-40, as a proinflammatory biomarker, on early stage of nephropathy in type 2 diabetic patients. J. Diabetes Complicat 2012, 26, 308–312. [Google Scholar]
- Bojesen, S.E.; Johansen, J.S.; Nordestgaard, B.G. Plasma YKL-40 levels in healthy subjects from the general population. Clin. Chim. Acta 2011, 412, 709–712. [Google Scholar]
- Kim, H.R.; Jun, C.D.; Lee, K.S.; Cho, J.H.; Jeong, E.T.; Yang, S.H.; Lee, Y.J.; Park, D.S. Levels of YKL-40 in pleural effusions and blood from patients with pulmonary or pleural disease. Cytokine 2012, 58, 336–343. [Google Scholar]
- Létuvé, S.; Kozhich, A.; Arouche, N.; Grandsaigne, M.; Reed, J.; Dombret, M.C.; Kiener, P.A.; Aubier, M.; Coyle, A.J.; Pretolani, M. YKL-40 is elevated in patients with chronic obstructive pulmonary disease and activates alveolar macrophages. J. Immunol 2008, 181, 5167–5173. [Google Scholar]
- Østergaard, C.; Johansen, J.S.; Benfield, T.; Price, P.A.; Lundgren, J.D. YKL-40 is elevated in cerebrospinal fluid from patients with purulent meningitis. Clin. Diagn. Lab. Immunol 2002, 9, 598–604. [Google Scholar]
- Kronborg, G.; Ostergaard, C.; Weis, N.; Nielsen, H.; Obel, N.; Pedersen, S.S.; Price, P.A.; Johansen, J.S. Serum level of YKL-40 is elevated in patients with Streptococcus pneumoniae bacteremia and is associated with the outcome of the disease. Scand. J. Infect. Dis 2002, 34, 323–326. [Google Scholar]
- Rathcke, C.N.; Persson, F.; Tarnow, L.; Rossing, P.; Vestergaard, H. YKL-40, a marker of inflammation and endothelial dysfunction, is elevated in patients with type 1 diabetes and increases with levels of albuminuria. Diabetes Care 2009, 32, 323–328. [Google Scholar]
- Ober, C.; Tan, Z.; Sun, Y.; Possick, J.D.; Pan, L.; Nicolae, R.; Radford, S.; Parry, R.R.; Heinzmann, A.; Klaus, A. Effect of variation in CHI3L1 on serum YKL-40 level, risk of asthma, and lung function. N. Engl. J. Med 2008, 358, 1682–1691. [Google Scholar]
- Xie, F.; Qian, Q.; Chen, Z.; Ma, G.; Feng, Y. Chitinase 3-like 1 gene-329G/A polymorphism, plasma concentration and risk of coronary heart disease in a Chinese population. Gene 2012, 499, 135–138. [Google Scholar]
- Park, H.Y.; Jun, C.D.; Jeon, S.J.; Choi, S.S.; Kim, H.R.; Choi, D.B.; Kwak, S.; Lee, H.S.; Cheong, J.S.; So, H.S.; et al. Serum YKL-40 levels correlate with infarct volume, stroke severity, and functional outcome in acute ischemic stroke patients. PLoS One 2012, 7, e51722. [Google Scholar]
- Johansen, J.S.; Schultz, N.A.; Jensen, B.V. Plasma YKL-40: A potential new cancer biomarker? Future Oncol 2009, 5, 1065–1082. [Google Scholar]
- Rathcke, C.N.; Vestergaard, H. YKL-40—An emerging biomarker in cardiovascular disease and diabetes. Cardiovasc. Diabetol 2009. [Google Scholar] [CrossRef]
© 2013 by the authors; licensee MDPI, Basel, Switzerland This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Wang, H.-L.; Hsiao, P.-C.; Tsai, H.-T.; Yeh, C.-B.; Yang, S.-F. Usefulness of Plasma YKL-40 in Management of Community-Acquired Pneumonia Severity in Patients. Int. J. Mol. Sci. 2013, 14, 22817-22825. https://doi.org/10.3390/ijms141122817
Wang H-L, Hsiao P-C, Tsai H-T, Yeh C-B, Yang S-F. Usefulness of Plasma YKL-40 in Management of Community-Acquired Pneumonia Severity in Patients. International Journal of Molecular Sciences. 2013; 14(11):22817-22825. https://doi.org/10.3390/ijms141122817
Chicago/Turabian StyleWang, Hsiang-Ling, Pei-Ching Hsiao, Hsiu-Ting Tsai, Chao-Bin Yeh, and Shun-Fa Yang. 2013. "Usefulness of Plasma YKL-40 in Management of Community-Acquired Pneumonia Severity in Patients" International Journal of Molecular Sciences 14, no. 11: 22817-22825. https://doi.org/10.3390/ijms141122817




