Maternal Anxiety and Children’s Laboratory Pain: The Mediating Role of Solicitousness
Abstract
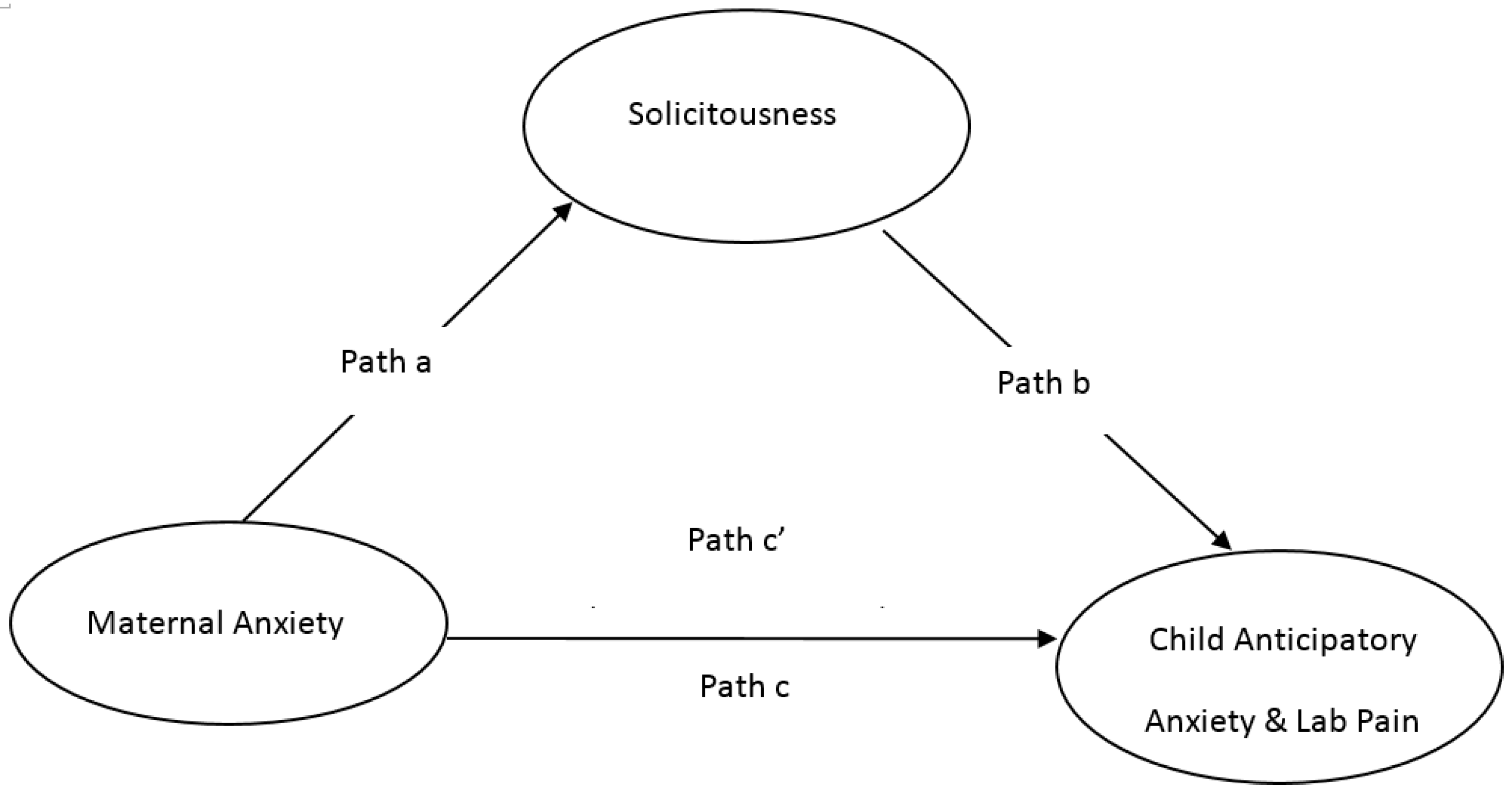
:1. Introduction
2. Methods
2.1. Participants
2.2. Procedures
2.2.1. Evoked Pressure (EP) Task
2.2.2. Cold Pressor Tolerance (CPT) Task
2.2.3. Tonic Pressure Tolerance (TPT) Task
2.2.4. Conditioned Pain Modulation (CPM) Task
2.3. Measures
2.3.1. Pain Task Measures
2.3.2. Self-Reporting Questionnaires
2.4. Data Analysis
3. Results
3.1. Descriptive Statistics
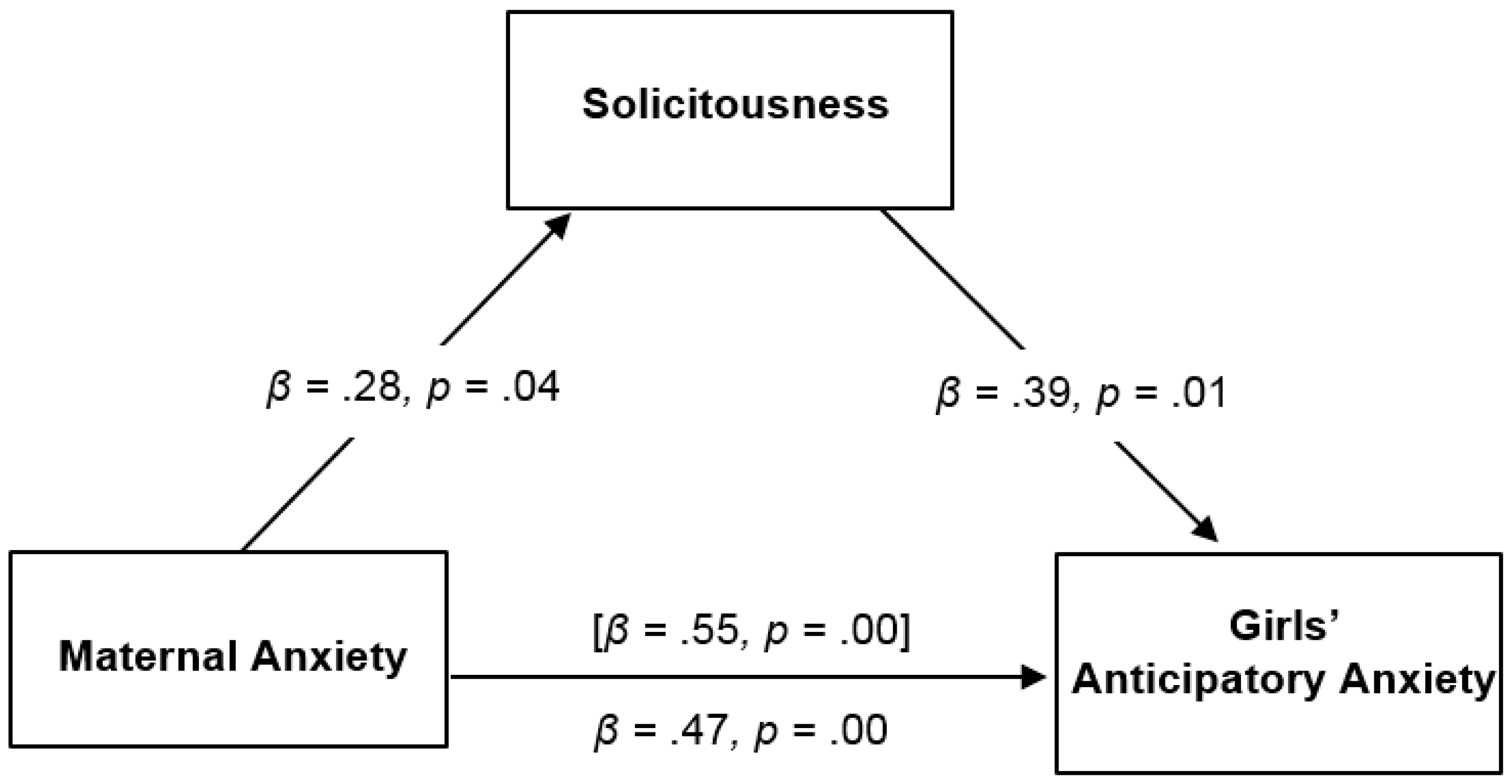
3.2. Hypothesis Testing
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Palermo, T.M.; Chambers, C.T. Parent and family factors in pediatric chronic pain and disability: An integrative approach. Pain 2005, 119, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Coric, A.; Banozic, A.; Klaric, M.; Vukojevic, K.; Puljak, L. Dental fear and anxiety in older children: An association with parental dental anxiety and effective pain coping strategies. J. Pain Res. 2014, 7, 515–521. [Google Scholar] [PubMed]
- Darlington, A.-S.E.; Verhulst, F.C.; De Winter, A.F.; Ormel, J.; Passchier, J.; Hunfeld, J.A.M. The influence of maternal vulnerability and parenting stress on chronic pain in adolescents in a general population sample: the TRAILS study. Eur. J. Pain 2012, 16, 150–159. [Google Scholar] [CrossRef] [PubMed]
- Levy, R.L.; Langer, S.L.; Romano, J.M.; Labus, J.; Walker, L.S.; Murphy, T.B.; Tilburg, M.A.; Feld, L.D.; Christie, D.L.; Whitehead, W.E. Cognitive mediators of treatment outcomes in pediatric functional abdominal pain. Clin. J. Pain 2014, 30, 1033–1043. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.L.; Gilleland, J.; Campbell, R.M.; Simpson, P.; Johnson, G.L.; Dooley, K.J.; Blount, R.L. Health care utilization and psychosocial factors in pediatric noncardiac chest pain. Health Psychol. 2013, 32, 320–327. [Google Scholar] [CrossRef] [PubMed]
- Martin, S.R.; Chorney, J.M.; Cohen, L.L.; Kain, Z.N. Sequential analysis of mothers' and fathers' reassurance and children's postoperative distress. J. Pediatr. Psychol. 2013, 38, 1121–1129. [Google Scholar] [CrossRef] [PubMed]
- Tourigny, J. Emotional states of mothers and behavior of the child during minor surgery. Can. J. Nurs. Res. 1992, 24, 65–80. [Google Scholar] [PubMed]
- Arai, Y.C.; Ueda, W.; Ito, H.; Wakao, Y.; Matsura, M.; Komatsu, T. Maternal heart rate variability just before surgery significantly correlated with emergence behavior of children undergoing general anesthesia. Paediatr. Anaesth. 2008, 18, 167–171. [Google Scholar] [CrossRef] [PubMed]
- Goodman, J.E.; McGrath, P.J. Mothers’ modeling influences children's pain during a cold pressor task. Pain 2003, 104, 559–565. [Google Scholar] [CrossRef]
- Noel, M.; Palermo, T.M.; Essner, B.; Zhou, C.; Levy, R.L.; Langer, S.L.; Sherman, A.L.; Walker, L.S. A developmental analysis of the factorial validity of the parent-report version of the Adult Responses to Children's Symptoms in children versus adolescents with chronic pain or pain-related chronic illness. J. Pain 2015, 16, 31–41. [Google Scholar] [CrossRef] [PubMed]
- Claar, R.L.; Simons, L.E.; Logan, D.E. Parental response to children's pain: the moderating impact of children's emotional distress on symptoms and disability. Pain 2008, 138, 172–179. [Google Scholar] [CrossRef] [PubMed]
- Penner, L.A.; Cline, R.J.; Albrecht, T.L.; Harper, F.W.; Peterson, A.M.; Taub, J.M.; Ruckdeschel, J.C. Parents’ Empathic Responses and Pain and Distress in Pediatric Patients. Basic Appl. Soc. Psych. 2008, 30, 102–113. [Google Scholar] [CrossRef] [PubMed]
- Walker, L.S.; Garber, J.; Greene, J.W. Psychosocial correlates of recurrent childhood pain: A comparison of pediatric patients with recurrent abdominal pain, organic illness, and psychiatric disorders. J. Abnorm. Psychol. 1993, 102, 248–258. [Google Scholar] [CrossRef] [PubMed]
- McMurtry, C.M.; McGrath, P.J.; Chambers, C.T. Reassurance can hurt: parental behavior and painful medical procedures. J. Pediatr. 2006, 148, 560–561. [Google Scholar] [CrossRef] [PubMed]
- Link, C.J.; Fortier, M.A. The Relationship Between Parent Trait Anxiety and Parent-reported Pain, Solicitous Behaviors, and Quality of Life Impairment in Children With Cancer. J. Pediatr. Hematol. Oncol. 2015, 1, 58–62. [Google Scholar] [CrossRef] [PubMed]
- Sieberg, C.B.; Williams, S.; Simons, L.E. Do parent protective responses mediate the relation between parent distress and child functional disability among children with chronic pain? J. Pediatr. Psychol. 2011, 36, 1043–1051. [Google Scholar] [CrossRef] [PubMed]
- Tsao, J.C.; Lu, Q.; Myers, C.D.; Kim, S.C.; Turk, N.; Zeltzer, L.K. Parent and child anxiety sensitivity: Relationship to children's experimental pain responsivity. J. Pain 2006, 7, 319–326. [Google Scholar] [CrossRef] [PubMed]
- Chambers, C.T.; Craig, K.D.; Bennett, S.M. The impact of maternal behavior on children's pain experiences: An experimental analysis. J. Pediatr. Psychol. 2002, 27, 293–301. [Google Scholar] [CrossRef] [PubMed]
- Walker, L.S.; Williams, S.E.; Smith, C.A.; Garber, J.; Van Slyke, D.A.; Lipani, T.A. Parent attention versus distraction: impact on symptom complaints by children with and without chronic functional abdominal pain. Pain 2006, 122, 43–52. [Google Scholar] [CrossRef] [PubMed]
- McGrath, P.J.; Walco, G.A.; Turk, D.C.; Dworkin, R.H.; Brown, M.T.; Davidson, K.; Eccleston, C.; Finley, G.A.; Goldschneider, K.; Haverkos, L.; et al. Core outcome domains and measures for pediatric acute and chronic/recurrent pain clinical trials: PedIMMPACT recommendations. J. Pain 2008, 9, 771–783. [Google Scholar] [CrossRef] [PubMed]
- Payne, L.A.; Seidman, L.C.; Lung, K.C.; Zeltzer, L.K.; Tsao, J.C. Relationship of neuroticism and laboratory pain in healthy children: Does anxiety sensitivity play a role? Pain 2013, 154, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Tsao, J.C.; Li, N.; Parker, D.; Seidman, L.C.; Zeltzer, L.K. Pubertal status moderates the association between mother and child laboratory pain tolerance. Pain Res. Manag. 2014, 19, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Tsao, J.C.; Seidman, L.C.; Evans, S.; Lung, K.C.; Zeltzer, L.K.; Naliboff, B.D. Conditioned pain modulation in children and adolescents: Effects of sex and age. J. Pain 2013, 14, 558–567. [Google Scholar] [CrossRef] [PubMed]
- Tsao, J.C.; Myers, C.D.; Craske, M.G.; Bursch, B.; Kim, S.C.; Zeltzer, L.K. Role of anticipatory anxiety and anxiety sensitivity in children's and adolescents' laboratory pain responses. J. Pediatr. Psychol. 2004, 29, 379–388. [Google Scholar] [CrossRef] [PubMed]
- Gracely, R.H.; Grant, M.A.; Giesecke, T. Evoked pain measures in fibromyalgia. Best. Pract. Res. Clin. Rheumatol. 2003, 17, 593–609. [Google Scholar] [CrossRef]
- Gracely, R.H.; Myers, C.D.; Craske, M.G.; Bursch, B.; Kim, S.C.; Zeltzer, L.K. A multiple random staircase method of psychophysical pain assessment. Pain 1988, 32, 55–63. [Google Scholar] [CrossRef]
- Dufton, L.M.; Konik, B.; Colletti, R.; Stanger, C.; Boyer, M.; Morrow, S.; Compas, B.E. Effects of stress on pain threshold and tolerance in children with recurrent abdominal pain. Pain 2008, 136, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Birnie, K.A.; Petter, M.; Boerner, K.E.; Noel, M.; Chambers, C.T. Contemporary use of the cold pressor task in pediatric pain research: A systematic review of methods. J. Pain 2012, 13, 817–826. [Google Scholar] [CrossRef] [PubMed]
- Von Baeyer, C.L.; Spagrud, L.J.; McCormick, J.C.; Choo, E.; Neville, K.; Connelly, M.A. Three new datasets supporting use of the Numerical Rating Scale (NRS-11) for children's self-reports of pain intensity. Pain 2009, 143, 223–227. [Google Scholar] [CrossRef] [PubMed]
- Derogatis, L.R. Brief Symptom Inventory (BSI) 18. In Administration, Scoring, and Procedures Manual; NCS Pearson, Inc.: Minneapolis, MN, USA, 2001. [Google Scholar]
- Van Slyke, D.A.; Walker, L.S. Mothers’ responses to children's pain. Clin. J. Pain. 2006, 22, 387–391. [Google Scholar] [CrossRef] [PubMed]
- Walker, L.S.; Levy, R.L.; Whitehead, W.E. Validation of a measure of protective parent responses to children's pain. Clin. J. Pain 2006, 22, 712–716. [Google Scholar] [CrossRef] [PubMed]
- Preacher, K.J.; Hayes, A.F. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav. Res. Methods 2008, 40, 879–891. [Google Scholar] [CrossRef] [PubMed]
- Rucker, D.D.; Preacher, K.J.; Tormala, Z.L.; Petty, R.E. Mediation analysis in social psychology: Current practices and new recommendations. Soc. Personal. Psychol. Compass 2011, 5, 359–371. [Google Scholar] [CrossRef]
- MacKinnon, D.P.; Krull, J.L.; Lockwood, C.M. Equivalence of the mediation, confounding and suppression effect. Prev. Sci. 2000, 1, 173–181. [Google Scholar] [CrossRef] [PubMed]
- Shrout, P.E.; Bolger, N. Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychol. Methods. 2002, 7, 422–445. [Google Scholar] [CrossRef] [PubMed]
- Logan, D.E.; Scharff, L. Relationships between family and parent characteristics and functional abilities in children with recurrent pain syndromes: An investigation of moderating effects on the pathway from pain to disability. J. Pediatr. Psychol. 2005, 30, 698–707. [Google Scholar] [CrossRef] [PubMed]
- Langer, S.L.; Romano, J.M.; Mancl, L.; Levy, R.L. Parental Catastrophizing Partially Mediates the Association between Parent-Reported Child Pain Behavior and Parental Protective Responses. Pain Res. Treat. 2014, 2014, 751097-05. [Google Scholar] [CrossRef] [PubMed]
- Evans, S.; Taub, R.; Tsao, J.C.; Meldrum, M.; Zeltzer, L.K. Sociodemographic factors in a pediatric chronic pain clinic: The roles of age, sex and minority status in pain and health characteristics. J. Pain Manag. 2010, 3, 273–281. [Google Scholar] [PubMed]

| Pain Boys (n = 28) | Pain Girls (n = 52) | |
|---|---|---|
| Child Age (mean (SD)) | 12.72 (2.35) | 14.92 * (2.45) |
| Pain Group Diagnoses (n (%)) | ||
| Headaches | 16 (57.1) | 33 (63.5) |
| Neurovisceral | 12 (42.9) | 25 (48.1) |
| Myofascial (non headache) | 10 (35.7) | 17 (32.7) |
| Fibromyalgia | 4 (14.3) | 17 (32.7) |
| CRPS | 3 (10.7) | 5 (9.6) |
| Joint pain | 3 (10.7) | 5 (9.6) |
| Child Ethnicity (n (% of subgroup)) | ||
| Non-Hispanic/Latino | 21 (75.0) | 36 (69.2) |
| Hispanic/Latino | 7 (25.0) | 16 (30.8) |
| Child Race (n (% of subgroup)) | ||
| White | 17 (60.7) | 37 (71.2) |
| African-American | 6 (21.4) | 5 (9.6) |
| Asian | 1 (3.6) | 1 (1.9) |
| American Indian/Alaska Native | 0 (0.0) | 0 (0.0) |
| Multi-Racial | 4 (14.3) | 9 (17.3) |
| Mother age [mean (SD)] | 44.70 (5.29) | 45.62 (6.63) |
| Mother Education Level (n (% of subgroup)) | ||
| High school graduate or below | 4 (14.3) | 8 (15.4) |
| Some college/AA degree | 8 (28.6) | 12 (23.1) |
| College graduate (BA/BS) | 8 (28.6) | 15 (28.8) |
| Post-graduate degree | 8 (28.6) | 17 (32.7) |
| Pain Boys | Pain Girls | |
|---|---|---|
| Mother BSI Anxiety Subscale | 2.68 (3.14) | 3.04 (3.11) |
| Child ARCS Protect Subscale | 2.02 (0.71) | 1.63 (0.58) |
| EP Ant Anx | 3.07 (2.36) | 2.92 (2.65) |
| EP Pain | 6.04 (2.52) | 6.51 (1.38) |
| CPT Ant Anx | 1.61 (1.57) | 1.98 (2.29) |
| CPT Pain | 5.89 (2.56) | 5.75 (2.90) |
| Pressure Ant Anx | 4.07 (2.73) | 3.18 (2.46) |
| Pressure Pain | 5.78 (2.78) | 6.02 (2.42) |
| CPM Ant Anx | 3.68 (2.77) | 3.21 (2.64) |
| CPM Pain | 6.13 (2.85) | 6.09 (2.90) |
| Maternal Anxiety | Solicitousness | |
|---|---|---|
| Girls with Pain | ||
| Maternal Solicitousness | 0.28 * | |
| Child Lab Pain | ||
| EP- Anticipatory Anxiety | 0.45 ** | 0.31 * |
| EP- Pain Intensity | 0.02 | 0.20 |
| CP- Anticipatory Anxiety | 0.45 ** | 0.34 * |
| CP- Pain Intensity | 0.12 | 0.35 * |
| TPT- Anticipatory Anxiety | 0.35 * | 0.30 * |
| TPT- Pain Intensity | 0.01 | 0.27 * |
| CPM- Anticipatory Anxiety | 0.45 ** | 0.40 * |
| CPM- Pain Intensity | 0.20 | 0.33 * |
| Boys with Pain | ||
| Maternal Solicitousness | −0.03 | |
| Child Lab Pain | ||
| EP- Anticipatory Anxiety | 0.38 * | 0.09 |
| EP- Pain Intensity | 0.41 * | −0.30 |
| CP- Anticipatory Anxiety | 0.17 | 0.03 |
| CP- Pain Intensity | 0.57 ** | −0.12 |
| TPT- Anticipatory Anxiety | 0.27 | 0.29 |
| TPT- Pain Intensity | 0.53 ** | 0.23 |
| CPM- Anticipatory Anxiety | 0.61 ** | −0.15 |
| CPM- Pain Intensity | 0.44 * | −0.11 |
| Maternal Predictors & Child Pain | Child Anticipatory Anxiety | Child Pain Intensity | Solicitousness | ||||||
|---|---|---|---|---|---|---|---|---|---|
| β | t | R² Δ | β | t | R² Δ | β | t | R² Δ | |
| Girls with Chronic Pain | |||||||||
| Child Age | −0.26 | −10.79 | 0.07 | 0.02 | 0.14 | 0.00 | 0.04 | 0.301 | 0.001 |
| Maternal Anxiety | 0.55 | 4.60 ** | 0.30 | 0.15 | 10.0 | 0.02 | 0.28 | 2.03* | 0.08 |
| Solicitousness | 0.39 | 2.95 ** | 0.15 | 0.36 | 2.6 * | 0.13 | |||
| Boys with Chronic Pain | |||||||||
| Child Age | −0.27 | −1.4 | 0.08 | −0.17 | −0.81 | 0.03 | −0.43 | −2.41 ** | 0.18 |
| Maternal Anxiety | 0.60 | 3.68 ** | 0.36 | 0.44 | 2.21 * | 0.19 | −0.23 | −1.21 | 0.05 |
| Solicitousness | 0.03 | 0.12 | 0.01 | −0.19 | −0.73 | 0.03 | |||
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Evans, S.; Payne, L.A.; Seidman, L.; Lung, K.; Zeltzer, L.; Tsao, J.C.I. Maternal Anxiety and Children’s Laboratory Pain: The Mediating Role of Solicitousness. Children 2016, 3, 10. https://doi.org/10.3390/children3020010
Evans S, Payne LA, Seidman L, Lung K, Zeltzer L, Tsao JCI. Maternal Anxiety and Children’s Laboratory Pain: The Mediating Role of Solicitousness. Children. 2016; 3(2):10. https://doi.org/10.3390/children3020010
Chicago/Turabian StyleEvans, Subhadra, Laura A. Payne, Laura Seidman, Kirsten Lung, Lonnie Zeltzer, and Jennie C. I. Tsao. 2016. "Maternal Anxiety and Children’s Laboratory Pain: The Mediating Role of Solicitousness" Children 3, no. 2: 10. https://doi.org/10.3390/children3020010





