Associations between Parents’ Health Literacy and Sleeping Hours in Children: A Cross-Sectional Study
Abstract
:1. Introduction
2. Methods
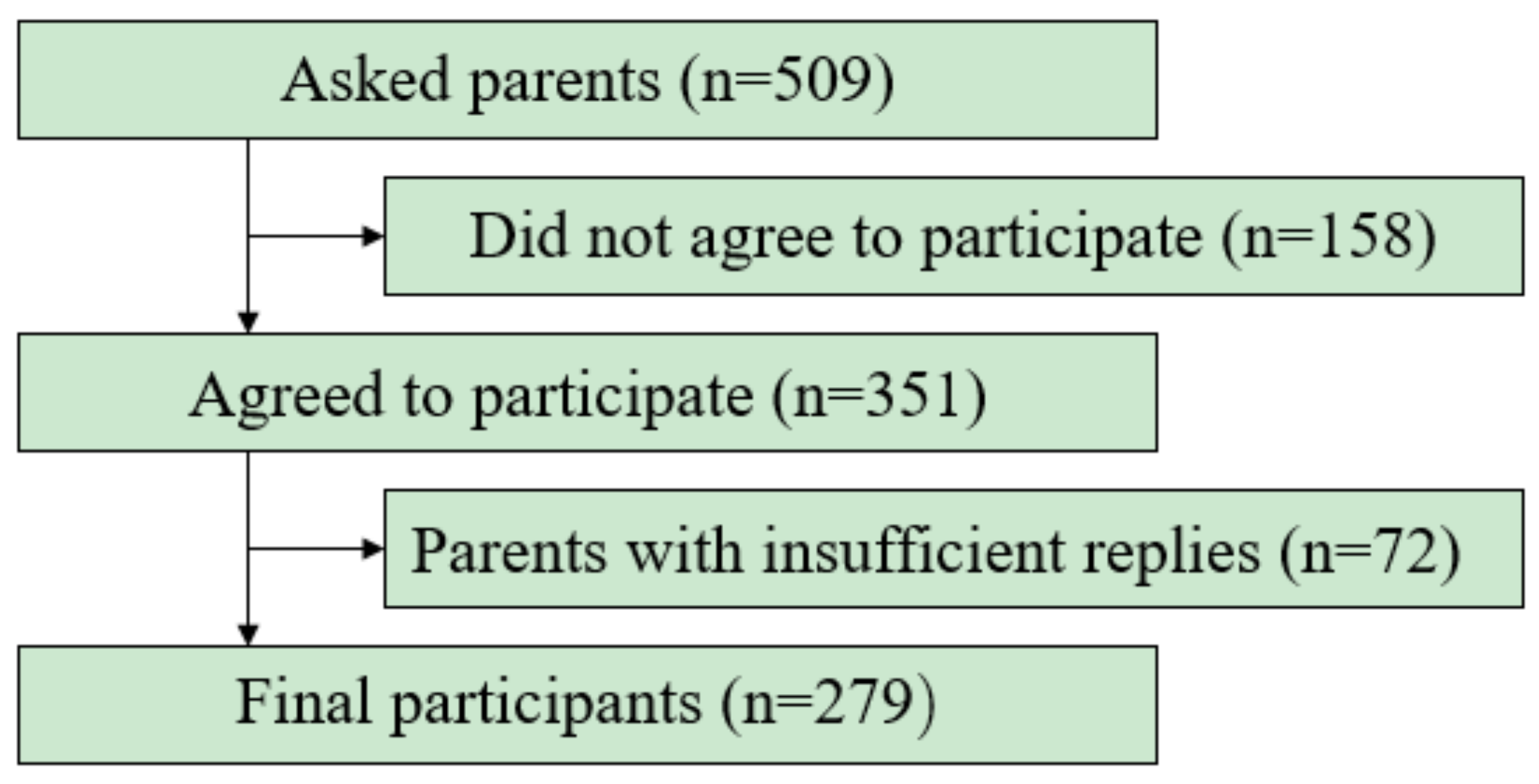
2.1. Participants
2.2. Demographic and Socioeconomic Characteristics
2.3. Health Literacy of Parents
2.4. Children’s Sleeping Duration
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| CI | confidence interval |
| HL | health literacy |
| HLS-14 | 14-item Health Literacy Scale |
| NSF | National Sleep Foundation |
References
- Dietch, J.R.; Taylor, D.J.; Smyth, J.M.; Ahn, C.; Smith, T.W.; Uchino, B.N.; Allison, M.; Ruiz, J.M. Gender and racial/ethnic differences in sleep duration in the North Texas heart study. Sleep Health 2017, 3, 324–327. [Google Scholar] [CrossRef] [PubMed]
- Schlieber, M.; Han, J. The sleeping patterns of Head Start children and the influence on developmental outcomes. Child Care Health Dev. 2017. [Google Scholar] [CrossRef] [PubMed]
- Sampei, M.; Dakeishi, M.; Wood, D.C.; Murata, K. Impact of total sleep duration on blood pressure in preschool children. Biomed. Res. 2006, 27, 111–115. [Google Scholar] [CrossRef] [PubMed]
- Sampei, M.; Murata, K.; Dakeishi, M.; Wood, D.C. Cardiac autonomic hypofunction in preschool children with short nocturnal sleep. Tohoku J. Exp. Med. 2006, 208, 235–242. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, K.; Yorifuji, T.; Yamakawa, M.; Oka, M.; Inoue, S.; Yoshinaga, H.; Doi, H. Poor toddler-age sleep schedules predict school-age behavioral disorders in a longitudinal survey. Brain Dev. 2015, 37, 572–578. [Google Scholar] [CrossRef] [PubMed]
- Bathory, E.; Tomopoulos, S. Sleep Regulation, Physiology and Development, Sleep Duration and Patterns, and Sleep Hygiene in Infants, Toddlers, and Preschool-Age Children. Curr. Probl. Pediatr. Adolesc. Health Care 2017, 47, 29–42. [Google Scholar] [CrossRef] [PubMed]
- Hirshkowitz, M.; Whiton, K.; Albert, S.M.; Alessi, C.; Bruni, O.; DonCarlos, L.; Hazen, N.; Herman, J.; Katz, E.S.; Kheirandish-Gozal, L.; et al. National Sleep Foundation’s sleep time duration recommendations: Methodology and results summary. Sleep Health 2015, 1, 40–43. [Google Scholar] [CrossRef] [PubMed]
- The 4th The General Condition Which Is Birth Child Running through Survey Result in the 21st Century. Available online: www.wam.go.jp/wamappl/bb16GS70.nsf/0/3baf55ad7af95af5492570cf001e6a58/$FILE/siryou_all.pdf (accessed on 10 March 2018).
- A Continual Comparative Study about the Degree of Infant Health. Available online: http://jschild.or.jp/book/pdf/2010_kenkochousa.pdf (accessed on 10 March 2018).
- Shinkoda, H.; Suetsugu, Y.; Asami, E.; Kato, N.; Kohyama, J.; Uchimura, N.; Chishaki, A.; Nishioka, K.; Okubo, I.; Matsumoto, K.; et al. Analysis of parent-child sleeping and living habits related to later bedtimes in children. Fukuoka Igaku Zasshi 2012, 103, 12–23. [Google Scholar] [PubMed]
- Nutbeam, D. The evolving concept of health literacy. Soc. Sci. Med. 2008, 67, 2072–2078. [Google Scholar] [CrossRef] [PubMed]
- Shum, J.; Poureslami, I.; Doyle-Waters, M.M.; FitzGerald, J.M. The application of health literacy measurement tools (collective or individual domains) in assessing chronic disease management: A systematic review protocol. Syst. Rev. 2016, 5, 97. [Google Scholar] [CrossRef] [PubMed]
- Kutner, M.; Greenberg, E.; Jin, Y.; Paulsen, C. The Health Literacy of America’s Adults: Results from the 2003 National Assessment of Adult Literacy; National Center for Education Statistics: Washington, DC, USA, 2006. [Google Scholar]
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Viera, A.; Crotty, K.; Holland, A.; Brasure, M.; Lohr, K.N.; Harden, E.; et al. Health literacy interventions and outcomes: An updated systematic review. Evid. Rep. Technol. Assess. (Full Rep.) 2011, 199, 1–941. [Google Scholar]
- Yin, H.S.; Forbis, S.G.; Dreyer, B.P. Health literacy and pediatric health. Curr. Probl. Pediatr. Adolesc. Health Care 2007, 37, 258–286. [Google Scholar] [CrossRef] [PubMed]
- Heerman, W.J.; Perrin, E.M.; Yin, H.S.; Sanders, L.M.; Eden, S.K.; Shintani, A.; Coyne-Beasley, T.; Bronaugh, A.B.; Barkin, S.L.; Rothman, R.L. Health literacy and injury prevention behaviors among caregivers of infants. Am. J. Prev. Med. 2014, 46, 449–456. [Google Scholar] [CrossRef] [PubMed]
- Harrington, K.F.; Zhang, B.; Magruder, T.; Bailey, W.C.; Gerald, L.B. The Impact of Parent’s Health Literacy on Pediatric Asthma Outcomes. Pediatr. Allergy Immunol. Pulmonol. 2015, 28, 20–26. [Google Scholar] [CrossRef] [PubMed]
- DeWalt, D.A.; Hink, A. Health literacy and child health outcomes: A systematic review of the literature. Pediatrics 2009, 124 (Suppl. 3), S265–S274. [Google Scholar] [CrossRef] [PubMed]
- Chari, R.; Warsh, J.; Ketterer, T.; Hossain, J.; Sharif, I. Association between health literacy and child and adolescent obesity. Patient Educ. Couns. 2014, 94, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Yokokawa, H.; Fukuda, H.; Yuasa, M.; Sanada, H.; Hisaoka, T.; Naito, T. Association between health literacy and metabolic syndrome or healthy lifestyle characteristics among community-dwelling Japanese people. Diabetol. Metab. Syndr. 2016, 8, 30. [Google Scholar] [CrossRef] [PubMed]
- Suka, M.; Yamauchi, T.; Sugimori, H. Help-seeking intentions for early signs of mental illness and their associated factors: Comparison across four kinds of health problems. BMC Public Health 2016, 16, 301. [Google Scholar] [CrossRef] [PubMed]
- Bathory, E.; Tomopoulos, S.; Rothman, R.; Sanders, L.; Perrin, E.M.; Mendelsohn, A.; Dreyer, B.; Cerra, M.; Yin, H.S. Infant Sleep and Parent Health Literacy. Acad. Pediatr. 2016, 16, 550–557. [Google Scholar] [CrossRef] [PubMed]
- Suka, M.; Odajima, T.; Kasai, M.; Igarashi, A.; Ishikawa, H.; Kusama, M.; Nakayama, T.; Sumitani, M.; Sugimori, H. The 14-item health literacy scale for Japanese adults (HLS-14). Environ. Health Prev. Med. 2013, 18, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Suka, M.; Odajima, T.; Okamoto, M.; Sumitani, M.; Igarashi, A.; Ishikawa, H.; Kusama, M.; Yamamoto, M.; Nakayama, T.; Sugimori, H. Relationship between health literacy, health information access, health behavior, and health status in Japanese people. Patient Educ. Couns. 2015, 98, 660–668. [Google Scholar] [CrossRef] [PubMed]
- Suka, M.; Odajima, T.; Okamoto, M.; Sumitani, M.; Nakayama, T.; Sugimori, H. Reading comprehension of health checkup reports and health literacy in Japanese people. Environ. Health Prev. Med. 2014, 19, 295–306. [Google Scholar] [CrossRef] [PubMed]
- Nakayama, K.; Osaka, W.; Togari, T.; Ishikawa, H.; Yonekura, Y.; Sekido, A.; Matsumoto, M. Comprehensive health literacy in Japan is lower than in Europe: A validated Japanese-language assessment of health literacy. BMC Public Health 2015, 15, 505. [Google Scholar] [CrossRef] [PubMed]
- Liechty, J.M.; Saltzman, J.A.; Musaad, S.M. Health literacy and parent attitudes about weight control for children. Appetite 2015, 91, 200–208. [Google Scholar] [CrossRef] [PubMed]
- Bernhardt, J.M.; Felter, E.M. Online pediatric information seeking among mothers of young children: Results from a qualitative study using focus groups. J. Med. Internet Res. 2004, 6, e7. [Google Scholar] [CrossRef] [PubMed]
- Paul, I.M.; Savage, J.S.; Anzman-Frasca, S.; Marini, M.E.; Mindell, J.A.; Birch, L.L. INSIGHT Responsive Parenting Intervention and Infant Sleep. Pediatrics 2016, 138, e20160762. [Google Scholar] [CrossRef] [PubMed]
- Lo, M.J. Relationship between Sleep Habits and Nighttime Sleep among Healthy Preschool Children in Taiwan. Ann. Acad. Med. Singap. 2016, 45, 549–556. [Google Scholar] [PubMed]
- Mitsutake, S.; Shibata, A.; Ishii, K.; Oka, K. Associations of eHealth Literacy With Health Behavior Among Adult Internet Users. J. Med. Internet Res. 2016, 18, e192. [Google Scholar] [CrossRef] [PubMed]
- Curtis, L.M.; Revelle, W.; Waite, K.; Wilson, E.A.; Condon, D.M.; Bojarski, E.; Park, D.C.; Baker, D.W.; Wolf, M.S. Development and validation of the comprehensive health activities scale: A new approach to health literacy measurement. J. Health Commun. 2015, 20, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Aihara, Y.; Minai, J. Barriers and catalysts of nutrition literacy among elderly Japanese people. Health Promot. Int. 2011, 26, 421–431. [Google Scholar] [CrossRef] [PubMed]
- Campbell, M.J. Statistics at Square Two, 2nd ed.; BMJ Books; Blackwell: London, UK, 2006. [Google Scholar]
- Wamsley, E.J.; Tucker, M.; Payne, J.D.; Benavides, J.A.; Stickgold, R. Dreaming of a learning task is associated with enhanced sleep-dependent memory consolidation. Curr. Biol. 2010, 20, 850–855. [Google Scholar] [CrossRef] [PubMed]
- Fukuda, K.; Ishihara, K. Routine evening naps and night-time sleep patterns in junior high and high school students. Psychiatry Clin. Neurosci. 2002, 56, 229–230. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, T.; Matsumoto, S. Actual conditions of work, fatigue and sleep in non-employed, home-based female information technology workers with preschool children. Ind. Health 2005, 43, 142–150. [Google Scholar] [CrossRef] [PubMed]
- Xiao, G.; Ye, Q.; Han, T.; Yan, J.; Sun, L.; Wang, F. Study of the sleep quality and psychological state of patients with hepatitis B liver cirrhosis. Hepatol. Res. 2017, 48, E275–E282. [Google Scholar] [CrossRef] [PubMed]
- Sedov, I.D.; Cameron, E.E.; Madigan, S.; Tomfohr-Madsen, L.M. Sleep quality during pregnancy: A meta-analysis. Sleep Med. Rev. 2017, 38, 168–176. [Google Scholar] [CrossRef] [PubMed]
- Menear, A.; Elliott, R.; Aitken, L.A.; Lal, S.; McKinley, S. Repeated sleep-quality assessment and use of sleep-promoting interventions in ICU. Nurs. Crit. Care 2017, 22, 348–354. [Google Scholar] [CrossRef] [PubMed]
- Iwadare, Y.; Kamei, Y.; Usami, M.; Ushijima, H.; Tanaka, T.; Watanabe, K.; Kodaira, M.; Saito, K. Behavioral symptoms and sleep problems in children with anxiety disorder. Pediatr. Int. 2015, 57, 690–693. [Google Scholar] [CrossRef] [PubMed]
- Angelhoff, C.; Edell-Gustafsson, U.; Morelius, E. Sleep quality and mood in mothers and fathers accommodated in the family-centred paediatric ward. J. Clin. Nurs. 2017, 27, e544–e550. [Google Scholar] [CrossRef] [PubMed]
- Sekine, M.; Chen, X.; Hamanishi, S.; Wang, H.; Yamagami, T.; Kagamimori, S. The validity of sleeping hours of healthy young children as reported by their parents. J. Epidemiol. 2002, 12, 237–242. [Google Scholar] [CrossRef] [PubMed]
- Takemura, T.; Funaki, K.; Kanbayashi, T.; Kawamoto, K.; Tsutsui, K.; Saito, Y.; Aizawa, R.; Inomata, S.; Shimizu, T. Sleep habits of students attending elementary schools, and junior and senior high schools in Akita prefecture. Psychiatry Clin. Neurosci. 2002, 56, 241–242. [Google Scholar] [CrossRef] [PubMed]
- Kohyama, J.; Shiiki, T.; Hasegawa, T. Sleep duration of young children is affected by nocturnal sleep onset time. Pediatr. Int. 2000, 42, 589–591. [Google Scholar] [CrossRef] [PubMed]
- Kitamura, S.; Enomoto, M.; Kamei, Y.; Inada, N.; Moriwaki, A.; Kamio, Y.; Mishima, K. Association between delayed bedtime and sleep-related problems among community-dwelling 2-year-old children in Japan. J. Physiol. Anthropol. 2015, 34, 12. [Google Scholar] [CrossRef] [PubMed]


| When you read instructions or leaflets from hospitals or pharmacies, how do you agree or disagree about the following? | ||||||
| Strongly Disagree | Disagree | Not Sure | Agree | Strongly Agree | ||
| 1 | I find characters that I cannot read | 5 | 4 | 3 | 2 | 1 |
| 2 | The print is too small for me (even though I wear glasses) | 5 | 4 | 3 | 2 | 1 |
| 3 | The content is too difficult for me | 5 | 4 | 3 | 2 | 1 |
| 4 | It takes a long time to read them | 5 | 4 | 3 | 2 | 1 |
| 5 | I need someone to help me read them | 5 | 4 | 3 | 2 | 1 |
| If you are diagnosed as having a disease and you have little information about the disease and its treatment, how to you agree or disagree about the following? | ||||||
| Strongly Disagree | Disagree | Not sure | Agree | Strongly Agree | ||
| 6 | I collect information from various sources | 1 | 2 | 3 | 4 | 5 |
| 7 | I extract the information I want | 1 | 2 | 3 | 4 | 5 |
| 8 | I understand the obtained information | 1 | 2 | 3 | 4 | 5 |
| 9 | I tell my opinion about my illness to my doctor, family or friends | 1 | 2 | 3 | 4 | 5 |
| 10 | I apply the obtained information to my daily life | 1 | 2 | 3 | 4 | 5 |
| If you are diagnosed as having a disease and you can obtain information about the disease and its treatment how do you agree or disagree about the following? | ||||||
| Strongly Disagree | Disagree | Not sure | Agree | Strongly Agree | ||
| 11 | I consider whether the information if applicable to me | 1 | 2 | 3 | 4 | 5 |
| 12 | I consider whether the information is credible | 1 | 2 | 3 | 4 | 5 |
| 13 | I check whether the information is valid and reliable | 1 | 2 | 3 | 4 | 5 |
| 14 | I collect information to make my healthcare decisions | 1 | 2 | 3 | 4 | 5 |
| Characteristic | Total (n = 279) | High Health Literacy Group (n = 210) | Low Health Literacy Group (n = 69) | t-Value or χ2 Value * | p Value |
|---|---|---|---|---|---|
| Child | |||||
| Age (months) | 56.4 ± 10.0 | 56.3 ± 9.9 | 56.6 ± 10.6 | −0.15 | 0.88 |
| Sex (girls) | 119 (42.7%) | 89 (42.3%) | 30 (43.4%) | 0.15 * | 0.87 |
| BMI (kg/m2) | 15.6 ± 1.3 | 15.5 ± 1.2 | 15.7 ± 1.6 | −0.65 | 0.52 |
| Birth weight (g) | 3012.0 ± 451.1 | 2995.3 ± 431.8 | 3063.7 ± 506.2 | −1.09 | 0.28 |
| Number of siblings (n) | 1.2 ± 0.8 | 1.3 ± 0.8 | 1.1 ± 0.8 | 2.20 * | 0.03 |
| Sleep duration (Continuous h) | 9.4 ± 0.9 | 9.5 ± 0.9 | 9.1 ± 1.1 | 2.50 | 0.01 |
| Breakfast (everyday eater) | 261 (93.6%) | 199 (94.8%) | 62 (89.6%) | 1.47 * | 0.14 |
| Parent | |||||
| Age (years) | 36.2 ± 5.1 | 35.9 ± 5.2 | 37.2 ± 4.9 | −2.02 | 0.05 |
| Sex (female) | 258 (92.4%) | 199 (94.7%) | 59 (85.5%) | 2.58 * | 0.01 |
| BMI (kg/m2) | 21.1 ± 2.9 | 21.1 ± 2.8 | 21.1 ± 3.1 | −0.19 | 0.85 |
| Marital status (married) | 258 (92.4%) | 195 (92.8%) | 63 (91.3%) | 0.70 * | 0.50 |
| Education (years) | 13.3 ± 1.6 | 13.3 ± 1.6 | 13.2 ± 1.7 | −0.59 | 0.56 |
| Household income <5 million Yen (n) | 143 (51.3%) | 111 (52.9%) | 32 (46.4%) | 0.93 * | 0.35 |
| Alcohol consumption (non-everyday drinker) | 255 (91.4%) | 193 (91.9%) | 62 (89.9%) | 1.02 * | 0.31 |
| Smoking behavior (non-smoking) | 225 (80.6%) | 170 (81.0%) | 55 (79.7%) | 0.22 * | 0.82 |
| Sleep duration (h) | 6.4 ± 1.1 | 6.4 ± 1.2 | 6.4 ± 1.1 | −0.53 | 0.60 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ogi, H.; Nakamura, D.; Ogawa, M.; Nakamura, T.; Izawa, K.P. Associations between Parents’ Health Literacy and Sleeping Hours in Children: A Cross-Sectional Study. Healthcare 2018, 6, 32. https://doi.org/10.3390/healthcare6020032
Ogi H, Nakamura D, Ogawa M, Nakamura T, Izawa KP. Associations between Parents’ Health Literacy and Sleeping Hours in Children: A Cross-Sectional Study. Healthcare. 2018; 6(2):32. https://doi.org/10.3390/healthcare6020032
Chicago/Turabian StyleOgi, Hiroto, Daisuke Nakamura, Masato Ogawa, Teruhiko Nakamura, and Kazuhiro P. Izawa. 2018. "Associations between Parents’ Health Literacy and Sleeping Hours in Children: A Cross-Sectional Study" Healthcare 6, no. 2: 32. https://doi.org/10.3390/healthcare6020032





