Investigation of the Antitumor Activity and Toxicity of Tumor-Derived Exosomes Fused with Long-Circulating and pH-Sensitive Liposomes Containing Doxorubicin
Abstract
:1. Introduction
2. Materials and Methods
2.1. Chemicals
2.2. Cells
2.3. Isolation of Exosomes
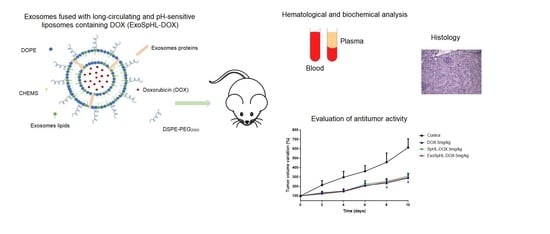
2.4. Preparation of ExoSpHL-DOX
2.5. ExoSpHL-DOX Characterization
2.5.1. Determination of the Diameter, Polydispersity Index, and Zeta Potential
2.5.2. Determination of the Content of DOX
2.6. Animals
2.7. Acute Toxicity
2.7.1. Hematology and Biochemistry Analyses
2.7.2. Histopathological Analysis
2.8. Evaluation of the Antitumor Activity
2.9. Statistical Analyses
3. Results
3.1. ExoSpHL-DOX Characterization
3.2. Acute Toxicity Study
3.2.1. Evaluation of Animal Mortality and Morbidity
3.2.2. Hematological Analysis
3.2.3. Biochemical Analysis
3.2.4. Histological Analysis
3.3. Antitumor Activity Evaluation
3.3.1. Evaluation of Body Weight Loss
3.3.2. Histological Analysis
4. Discussion
5. Conclusions
6. Patents
Author Contributions
Funding
Institutional Review Board Statement
Acknowledgments
Conflicts of Interest
Appendix A


Appendix B




Appendix C



References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Zhao, N.; Woodle, M.C.; Mixson, A.J. Advances in delivery systems for doxorubicin. J. Nanomed. Nanotechnol. 2018, 9, 519. [Google Scholar] [CrossRef]
- Jamialahmadi, K.; Zahedipour, F.; Karimi, G. The role of microRNAs on doxorubicin drug resistance in breast cancer. J. Pharm. Pharmacol. 2021, 73, 997–1006. [Google Scholar] [CrossRef] [PubMed]
- Ngan, Y.H.; Gupta, M. A comparison between liposomal and nonliposomal formulations of doxorubicin in the treatment of cancer: An updated review. Arch. Pharm. Pract. 2016, 7, 1. [Google Scholar]
- Liang, Y.; Duan, L.; Lu, J.; Xia, J. Engineering exosomes for targeted drug delivery. Theranostics 2021, 11, 3183–3195. [Google Scholar] [CrossRef]
- Mukherjee, A.; Bisht, B.; Dutta, S.; Paul, M.K. Current advances in the use of exosomes, liposomes, and bioengineered hybrid nanovesicles in cancer detection and therapy. Acta Pharmacol. Sin. 2022, 43, 2759–2776. [Google Scholar] [CrossRef]
- Gomes, E.R.; Carvalho, A.T.; Barbosa, T.C.; Ferreira, L.L.; Calado, H.D.R.; Sabino, A.P.; Oliveira, M.C. Fusion of tumor-derived exosomes with long-circulating and pH-sensitive liposomes loaded with doxorubicin for the treatment of breast cancer. AAPS-PharmSciTech 2022, 23, 255. [Google Scholar] [CrossRef]
- Bangham, A.D.; Standish, M.M.; Watkins, J.C. Diffusion of univalent ions across the lamellae of swollen phospholipids. J. Mol. Biol. 1965, 13, 238–252. [Google Scholar] [CrossRef]
- Silva, J.O.; Fernandes, R.S.; Oda, C.M.R.; Ferreira, T.H.; Botelho, A.F.M.; Melo, M.M.; de Miranda, M.C.; Gomes, D.A.; Cassali, G.D.; Townsend, D.M.; et al. Folate-coated, long-circulating and pH-sensitive liposomes enhance doxorubicin antitumor effect in a breast cancer animal model. Biomed. Pharm. 2019, 118, 109323. [Google Scholar] [CrossRef]
- Ferreira, D.S.; Faria, S.D.; Lopes, S.C.d.; Teixeira, C.S.; Malachias, A.; Magalhães-Paniago, R.; Filho, J.D.d.; Oliveira, B.L.d.P.; Guimarães, A.R.; Caravan, P.; et al. Development of a bone-targeted pH-sensitive liposomal formulation: Physicochemical characterization, cytotoxicity, and biodistribution evaluation in a mouse model of bone metastasis. Int. J. Nanomed. 2016, 11, 3737–3751. [Google Scholar]
- OECD. Test No. 423: Acute Oral Toxicity—Acute Toxic Class Method. In OECD Guidelines for the Testing of Chemicals; Section 4; OECD Publishing: Paris, France, 2002. [Google Scholar]
- Silva, J.O.; Miranda, S.E.M.; Leite, E.A.; Sabino, A.d.; Borges, K.B.G.; Cardoso, V.N.; Cassali, G.D.; Guimarães, A.G.; Oliveira, M.C.; Barros, A.L.B.; et al. Toxicological study of a new doxorubicin-loaded pH-sensitive liposome: A preclinical approach. Toxicol. Appl. Pharmacol. 2018, 352, 162–169. [Google Scholar] [CrossRef]
- Lages, E.B.; Fernandes, R.S.; Silva, J.d.; de Souza, Â.M.; Cassali, G.D.; Barros, A.L.B.; Ferreira, L.A.M. Co-delivery of doxorubicin, docosahexaenoic acid, and α-tocopherol succinate by nanostructured lipid carriers has a synergistic effect to enhance antitumor activity and reduce toxicity. Biomed. Pharm. 2020, 132, 110876. [Google Scholar] [CrossRef]
- Rolland, C.L.; Dineen, S.P.; Lynn, K.D.; Sullivan, L.A.; Dellinger, M.T.; Sadegh, L.; Sullivan, J.P.; Shames, D.S.; Brekken, R.A. Inhibition of vascular endothelial growth factor reduces angiogenesis and modulates immune cell infiltration of orthotopic breast cancer xenografts. Mol. Cancer Ther. 2009, 8, 1761–1771. [Google Scholar] [CrossRef] [Green Version]
- Garcia, C.M.; de Araújo, M.R.; Lopes, M.T.P.; Ferreira, M.A.N.D.; Cassali, G.D. Morphological and immunophenotipical characterization of murine mammary carcinoma 4T1. Braz. J. Vet. Pathol. 2014, 7, 158–165. [Google Scholar]
- Qiao, L.; Hu, S.; Huang, K.; Su, T.; Li, Z.; Vandergriff, A.; Cores, J.; Dinh, P.; Allen, T.; Shen, D.; et al. Tumor cell-derived exosomes home to their cells of origin and can be used as Trojan horses to deliver cancer drugs. Theranostics 2020, 10, 3474–3487. [Google Scholar] [CrossRef]
- Sun, L.; Fan, M.; Huang, D.; Li, B.; Xu, R.; Gao, F.; Chen, Y. Clodronate-loaded liposomal and fibroblast-derived exosomal hybrid system for enhanced drug delivery to pulmonary fibrosis. Biomaterials 2021, 271, 120761. [Google Scholar] [CrossRef]
- Li, L.; Di He, D.; Guo, Q.; Zhang, Z.; Ru, D.; Wang, L.; Gong, K.; Liu, F.; Duan, Y.; Li, H. Exosome-liposome hybrid nanoparticle codelivery of TP and miR497 conspicuously overcomes chemoresistant ovarian cancer. J. Nanobiotechnol. 2022, 20, 50. [Google Scholar] [CrossRef]
- Lv, Q.; Cheng, L.; Lu, Y.; Zhang, X.; Wang, Y.; Deng, J.; Zhou, J.; Liu, B.; Liu, J. Thermosensitive exosome-liposome hybrid nanoparticle-mediated chemoimmunotherapy for improved treatment of metastatic peritoneal cancer. Adv. Sci. 2020, 7, 2000515. [Google Scholar] [CrossRef]
- Roque, M.C.; da Silva, C.D.; Lempek, M.R.; Cassali, G.D.; de Barros, A.L.B.; Melo, M.M.; Oliveira, M.C. Preclinical toxicological study of long-circulating and fusogenic liposomes co-encapsulating paclitaxel and doxorubicin in synergic ratio. Biomed. Pharm. 2021, 144, 112307. [Google Scholar] [CrossRef]
- Toblli, J.E.; Rivas, C.; Cao, G.; Giani, J.F.; Funk, F.; Mizzen, L.; Dominici, F.P. Ferric carboxymaltose-mediated attenuation of doxorubicin-induced cardiotoxicity in an iron deficiency rat model. Chemother. Res. Pract. 2014, 2014, 570241. [Google Scholar] [CrossRef] [Green Version]
- Toffoli, G.; Hadla, M.; Corona, G.; Caligiuri, I.; Palazzolo, S.; Semeraro, S.; Gamini, A.; Canzonieri, V.; Rizzolio, F. Exosomal doxorubicin reduces the cardiac toxicity of doxorubicin. Nanomedicine 2015, 10, 2963–2971. [Google Scholar] [CrossRef] [PubMed]
- Dasa, S.S.K.; Suzuki, R.; Mugler, E.; Chen, L.; Jansson-Löfmark, R.; Michaëlsson, E.; Lindfors, L.; Klibanov, A.L.; French, B.A.; Kelly, K.A. Evaluation of pharmacokinetic and pharmacodynamic profiles of liposomes for the cell type-specific delivery of small molecule drugs. Nanomed. Nanotechnol. Biol. Med. 2017, 13, 2565–2574. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, L.O.F.; Fernandes, R.S.; Oda, C.M.R.; Lopes, S.C.; Townsend, D.M.; Cardoso, V.N.; Oliveira, M.C.; Leite, E.A.; Rubello, D.; de Barros, A.L.B. Paclitaxel-loaded folate-coated long circulating and pH-sensitive liposomes as a potential drug delivery system: A biodistribution study. Biomed. Pharm. 2018, 97, 489–495. [Google Scholar] [CrossRef]
- Wang, K.; Ye, H.; Zhang, X.; Wang, X.; Yang, B.; Luo, C.; Zhao, Z.; Zhao, J.; Lu, Q.; Zhang, H.; et al. An exosome-like programmable-bioactivating paclitaxel prodrug nanoplatform for enhanced breast cancer metastasis inhibition. Biomaterials 2020, 257, 120224. [Google Scholar] [CrossRef]
- Nie, H.; Xie, X.; Zhang, D.; Zhou, Y.; Li, B.; Li, F.; Li, F.; Cheng, Y.; Mei, H.; Meng, H.; et al. Use of lung-specific exosomes for miRNA-126 delivery in non-small cell lung cancer. Nanoscale 2020, 12, 877–887. [Google Scholar] [CrossRef] [PubMed]







| Blood Components | Control | Free DOX | SpHL-DOX | ExoSpHL-DOX | |||
|---|---|---|---|---|---|---|---|
| 10 mg/kg | 12.5 mg/kg | 15 mg/kg | 17.5 mg/kg | 15 mg/kg | 17.5 mg/kg | ||
| WBC (103/mm3) | 4.95 ± 1.13 | 4.55 ± 1.62 b | 9.53 ± 2.12 a | 4.20 ± 1.18 b | 4.85 ± 0.41 b | 5.83 ± 1.40 b | 4.48 ± 0.82 b |
| AGRANULOCYTES (103/mm3) | 3.68 ± 0.99 | 3.15 ± 1.25 b | 7.15 ± 2.58 a | 2.58 ± 0.95 b | 2.87 ± 0.30 b | 3.77 ± 0.97 b | 3.00 ± 0.60 b |
| GRANULOCYTES (103/mm3) | 1.27 ± 0.27 | 1.40 ± 0.41 b | 2.80 ± 1.05 a | 1.34 ± 0.46 b | 1.98 ± 0.36 b | 2.07 ± 0.59 b | 1.48 ± 0.26 b |
| RBC (106/mm3) | 6.26 ± 0.72 | 5.95 ± 0.45 b | 4.18 ± 0.36 a | 6.06 ± 0.25 b | 5.79 ± 0.18 b | 5.30 ± 0.26 b | 6.10 ± 0.14 b |
| HGB (g/dL) | 12.68 ± 2.26 | 11.43 ± 1.06 b | 8.40 ± 1.35 a | 11.72 ± 0.64 b | 11.53 ± 0.45 b | 10.23 ± 0.43 | 12.10 ± 0.41 b |
| HCT (%) | 30.90 ± 3.47 | 30.00 ± 2.05 b | 21.55 ± 1.52 a | 29.68 ± 1.30 b | 28.87 ± 1.01 b | 26.82 ± 2.03 b | 30.04 ± 0.86 b |
| PLT (103/mm3) | 338.20 ± 22.66 | 254.2 ± 24.70 | 335.50 ± 78.57 | 351.80 ± 57.90 | 333.80 ± 61.90 | 314.20 ± 40.51 | 314.00 ± 79.53 |
| Biochemical Parameters | Control | Free DOX | SpHL-DOX | ExoSpHL-DOX | |||
|---|---|---|---|---|---|---|---|
| 10 mg/kg | 12.5 mg/kg | 15 mg/kg | 17.5 mg/kg | 15 mg/kg | 17.5 mg/kg | ||
| Creatinine (mg/dL) | 0.30 ± 0.09 | 0.22 ± 0.07 | 0.29 ± 0.12 | 0.19 ± 0.04 | 0.20 ± 0.03 | 0.31 ± 0.06 | 0.22 ± 0.04 |
| Urea (mg/dL) | 35.54 ± 3.92 | 40.51 ± 18.06 b | 149.10 ± 14.89 a | 34.82 ± 9.91 b | 39.20 ± 13.33 b | 31.16 ± 1.73 b | 30.63 ± 1.37 b |
| ALT (U/L) | 44.09 ± 7.34 | 52.97 ± 15.68 | 48.01 ± 9.34 | 45.54 ± 11.21 | 56.39 ± 10.01 | 47.72 ± 5.86 | 51.67 ± 7.71 |
| AST (U/L) | 124.30 ± 24.72 | 93.78 ± 25.79 | 127.80 ± 10.44 | 109.20 ± 41.60 | 128.00 ± 26.19 | 110.70 ± 30.26 | 126.30 ± 24.95 |
| CK-MB (U/L) | 28.31 ± 6.36 | 33.46 ± 13.55 b,c | 89.34 ± 8.03 a | 33.90 ± 10.33 b | 52.49 ± 13.51 a,b | 25.99 ± 7.47 b,c,d | 49.11 ± 6.58 a,b |
| Treatment | RTV | TGI (%) |
|---|---|---|
| HBS (control) | 6.1 ± 0.9 | - |
| ExoSpHL | 6.1 ± 0.6 | - |
| Free DOX 5 mg/kg | 2.9 ± 0.4 a | 52.5 |
| SpHL-DOX 5 mg/kg | 2.8 ± 0.1 a | 54.1 |
| ExoSpHL-DOX 5 mg/kg | 2.7 ± 0.4 a | 55.7 |
| HBS | ExoSpHL | DOX | SpHL-DOX | ExoSpHL-DOX | ||
|---|---|---|---|---|---|---|
| Animal 1 | + | + | 0 | + | 0 | |
| Animal 2 | ++ | 0 | ++ | 0 | 0 | |
| Score | Animal 3 | + | + | + | + | + |
| Animal 4 | ++ | 0 | 0 | 0 | 0 | |
| Animal 5 | ++ | 0 | 0 | + | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gomes, E.R.; Souza, F.R.; Cassali, G.D.; Sabino, A.d.P.; Barros, A.L.B.d.; Oliveira, M.C. Investigation of the Antitumor Activity and Toxicity of Tumor-Derived Exosomes Fused with Long-Circulating and pH-Sensitive Liposomes Containing Doxorubicin. Pharmaceutics 2022, 14, 2256. https://doi.org/10.3390/pharmaceutics14112256
Gomes ER, Souza FR, Cassali GD, Sabino AdP, Barros ALBd, Oliveira MC. Investigation of the Antitumor Activity and Toxicity of Tumor-Derived Exosomes Fused with Long-Circulating and pH-Sensitive Liposomes Containing Doxorubicin. Pharmaceutics. 2022; 14(11):2256. https://doi.org/10.3390/pharmaceutics14112256
Chicago/Turabian StyleGomes, Eliza Rocha, Fernanda Rezende Souza, Geovanni Dantas Cassali, Adriano de Paula Sabino, André Luis Branco de Barros, and Mônica Cristina Oliveira. 2022. "Investigation of the Antitumor Activity and Toxicity of Tumor-Derived Exosomes Fused with Long-Circulating and pH-Sensitive Liposomes Containing Doxorubicin" Pharmaceutics 14, no. 11: 2256. https://doi.org/10.3390/pharmaceutics14112256