- Article
Optimizing Quality of Care for Elderly Tuberculosis Patients in Shanghai, China: Insights from Patient Cascade of Care and Patient Pathway Analysis
- Yutong Han,
- Lixin Rao and
- Biao Xu
- + 3 authors
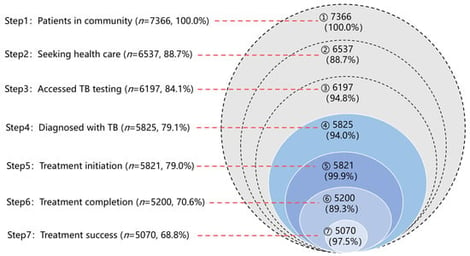
With population aging, the burden of tuberculosis (TB) among the elderly is rising. Older adults are at high risk of TB but susceptible to poor TB care. In this study, we enrolled TB patients aged over 60 years registered in Shanghai during 2019–2021. A seven-step care cascade from estimated TB burden in the community to treatment outcomes was constructed to quantify retention and attrition at each step of TB health service. Patient pathway analysis was carried out in two districts of Shanghai to describe patients’ care-seeking behaviors, service coverage, and diagnosis delays. Across the care cascade, the largest gaps occurred from symptom onset to care seeking (11.3%) and from treatment initiation to completion (10.7%). Male sex, older age, and mycobacterium tuberculosis positivity were associated with treatment discontinuation and unfavorable outcomes. The patient pathway analysis revealed that first contact at lower-level or non-TB-designated hospitals was associated with more complex pathways and may contribute to diagnostic delays. These findings highlight the need to promote proactive care seeking upon symptoms, strengthen targeted adherence support for older people, and improve diagnostic capacity and referral efficiency at lower-level health facilities.
12 February 2026