- Article
Blood Flow Restriction Training Improves Cognition Performance and Sleep Quality in Middle-Aged Adults with Relapsing–Remitting Multiple Sclerosis
- Javier Cano-Sánchez,
- María del Carmen Carcelén-Fraile and
- Juan Miguel Muñoz-Perete
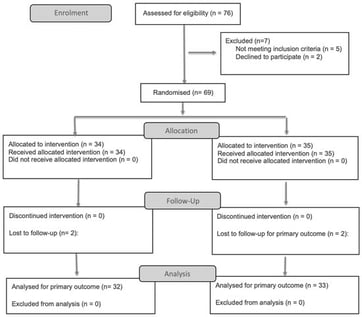
Background/Objectives: Cognitive impairment and sleep disturbances are highly prevalent in individuals with multiple sclerosis (MS), particularly during middle age, and negatively affect functional independence and quality of life. Although physical exercise has demonstrated cognitive and sleep-related benefits in MS, tolerance to high-intensity training is often limited. Blood flow restriction (BFR) training, which combines low-load resistance exercise with partial vascular occlusion, has emerged as a feasible alternative. This study aimed to evaluate the effects of a 12-week BFR training program on performance in specific cognitive domains and sleep quality in middle-aged adults with MS. Methods: A randomized controlled trial was conducted in 65 adults with relapsing–remitting multiple sclerosis (RRMS) aged 40–65 years and an Expanded Disability Status Scale score below 7. Participants were randomly assigned to a BFR training group or a usual-care control group. The intervention consisted of supervised low-load resistance training with BFR performed twice weekly for 12 weeks. Outcomes assessed before and after the intervention included processing speed (Symbol Digit Modalities Test), executive function (Trail Making Test A and B), verbal fluency (Isaacs Set Test), and self-reported sleep quality (Pittsburgh Sleep Quality Index). Results: Compared with controls, participants in the BFR group showed significant improvements in specific cognitive domains, including processing speed, executive function, and verbal fluency. Significant reductions were also observed in self-reported global sleep disturbance and daytime dysfunction. No adverse events were reported. Conclusions: A 12-week BFR training program improved performance in key cognitive domains and self-reported sleep quality in middle-aged adults with MS, supporting its feasibility and potential clinical relevance as an exercise-based intervention.
6 February 2026