- Article
Antitumor Effects of a Recombinant Streptococcus pyogenes Strain on Pancreatic Cancer Progression and Metastasis in an Orthotopic Mice Model
- Anna N. Tsapieva,
- Nadezhda V. Duplik and
- Alexander N. Suvorov
- + 13 authors
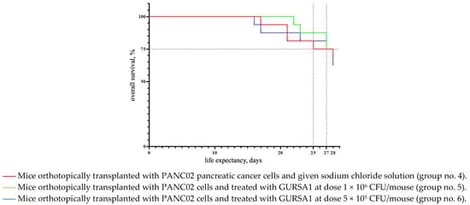
Objectives. Pancreatic cancer remains one of the most lethal malignancies, and the lack of effective therapies highlights the need for novel treatment strategies. In this study, we evaluated the antitumor potential of the attenuated Streptococcus pyogenes strain GURSA1—engineered to knockout the M protein completely—in a murine model of orthotopically transplanted pancreatic ductal adenocarcinoma. Methods. Female C57Bl/6 mice received intratumoral injections of GURSA1 at doses of 5 × 105 or 1 × 106 CFU per animal. Animal survival, body weight, tumor engraftment, metastasis intensity, tumor mass and volume, and hematological, biochemical, histological, and microbiological parameters were assessed. Results. Intratumoral administration of GURSA1 produced dose-dependent antitumor effects on tumor growth and metastatic burden, but did not result in a statistically significant survival benefit. The strain reduced tumor engraftment, the overall metastasis score, and the incidence of hemorrhagic ascites, while also decreasing tumor mass and volume, with the strongest effects observed at a dose of 1 × 106 CFU. Treatment increased platelet counts and reduced urea and ALT levels toward values observed in intact mice, without affecting anemia, neutrophilia, or changes in AST, alkaline phosphatase, glucose, and total protein levels. Conclusions. These findings demonstrate that GURSA1 attenuates partial reduction in primary tumor burden in vivo and support further investigation of this strain as a potential oncolytic agent.
5 February 2026



![Representative histologic section of cervical squamous cell carcinoma. Neoplastic cells (arrow) show an infiltrative growth pattern within a reactive stroma rich in inflammatory cells [Hematoxylin & Eosin stain. (A) Original magnification 100×; (B) Original magnification 200×, corresponding to the area outlined by the black box in (A)]. (Source: Original figure created by the authors for this review).](https://mdpi-res.com/cdn-cgi/image/w=281,h=192/https://mdpi-res.com/onco/onco-06-00009/article_deploy/html/images/onco-06-00009-g001-550.jpg)